A pre-print study (not yet peer-reviewed) by U.S. Government researchers shows vaccinated people produce a less comprehensive immune system response following SARS-CoV-2 infection than unvaccinated people.
The researchers examined data from the Moderna Covid vaccine trial and found that, compared to unvaccinated controls, vaccinated participants produced far fewer N-antibodies. These are antibodies against the nucleocapsid protein inside the virus particle, in contrast to S-antibodies against the spike protein that the vaccines target. N-antibodies were detected in 40% (21 of 52) of infected vaccine recipients versus 93% (605 of 648) of placebo recipients. This means those infected after being vaccinated produced N-antibodies at less than half the rate of the unvaccinated.
The researchers found that N-seroconversion (producing N-antibodies following infection) was more likely for infections with higher viral loads. So they checked to see if the difference was due to the vaccinated having milder infections with lower viral loads owing to the vaccine. They found that it wasn’t: for the same viral load the unvaccinated were around 14 times (13.67, 95% confidence interval 5.17-36.16) more likely to have detectable N-antibodies following infection than the vaccinated. Look at the contrasting curves below: the yellow unvaccinated curve is much higher than the blue vaccinated curve, showing that for any given viral load (x-axis) the probability of detecting N-antibodies following infection (y-axis) is much lower for vaccinated than unvaccinated.
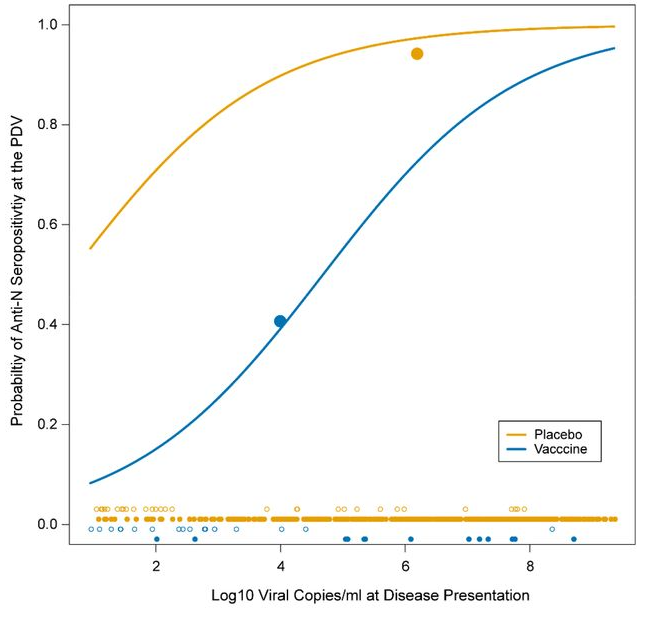
This means that although a vaccinated person may have S-antibodies from the vaccine, following infection he or she is much less likely to gain N-antibodies following infection than an unvaccinated person. This weaker immune response may make him or her more susceptible to future re-infection, particularly by variants which evade the S-antibodies, such as Omicron.
This also means, as the study authors point out, that a population survey of N-antibodies after a vaccination campaign will significantly underestimate the total number of people previously infected, as many of the vaccinated will not have produced N-antibodies following infection. This is likely one reason why the UKHSA reports around 42% of blood donors in England with N-antibodies to the end of February 2022, while the ONS estimates from its infection survey that around 71% of the country has been infected by February 11th (see below). The high infection rate among the vaccinated during the Delta and Omicron waves supports this explanation.
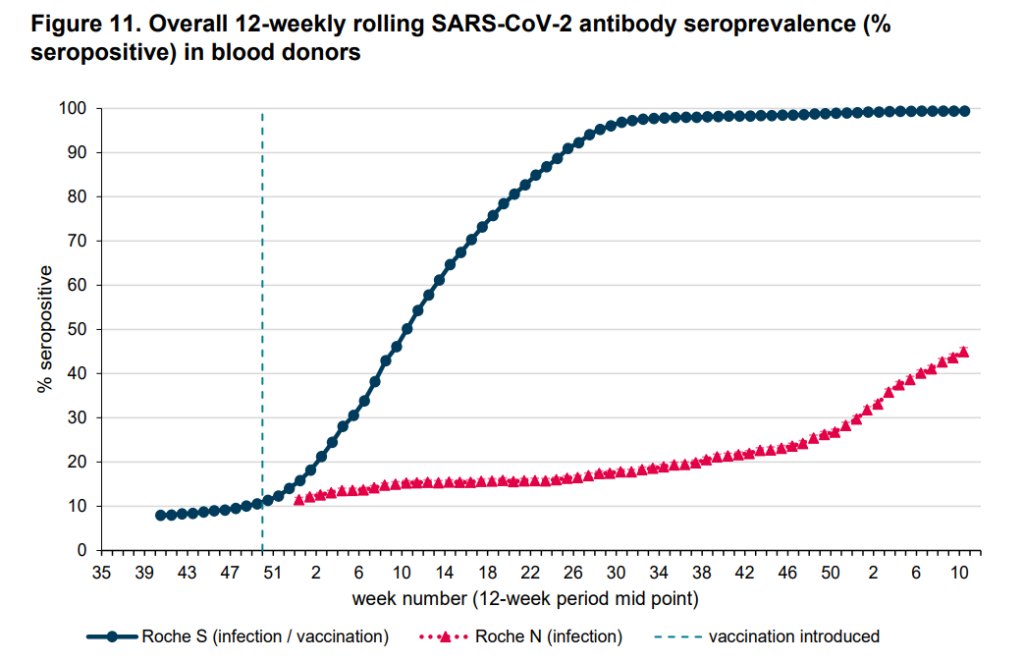
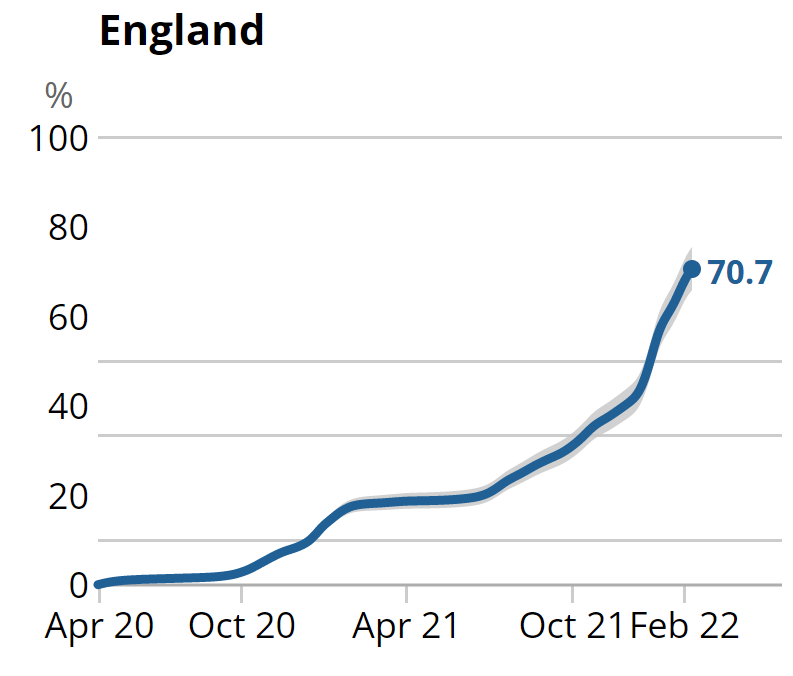
Let’s break those data down into successive Covid waves so we can see how many were infected in each wave according to the ONS and how many developed N-antibodies according to the UKHSA. In the below I’ve read 8% off the antibody graph above for the initial wave and, assuming the same proportion were infected in that wave, added a six point uplift to the cumulative infection total to allow for the pre-April 2020 infections.
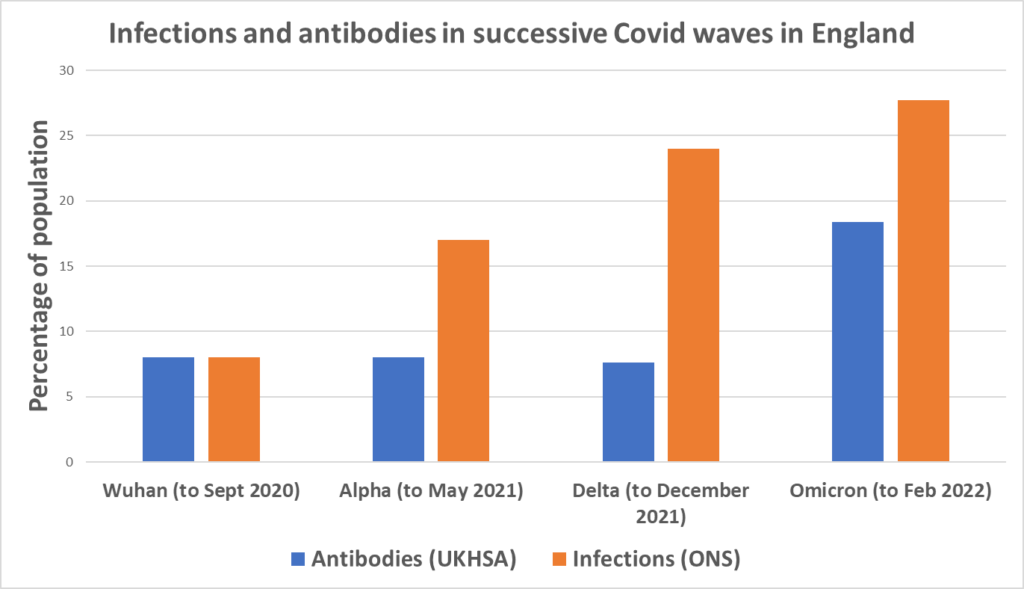
The most striking aspect of this chart is how much bigger the Delta wave was in infections than in antibodies – a result, we can assume, of the vaccines inhibiting N-seroconversion. It’s also notable that the pre-vaccine Alpha wave (almost all the infections for which occurred before February 2021, when very few were vaccinated) was around twice as large in infections than in antibodies, suggesting a relatively low rate of seroconversion despite the lack of vaccines, the reason for which is unclear. Then for Omicron, the ratio between the two gets much smaller, around 1.5, meaning infections were only 50% higher than antibodies. Here are those figures with the ratios.
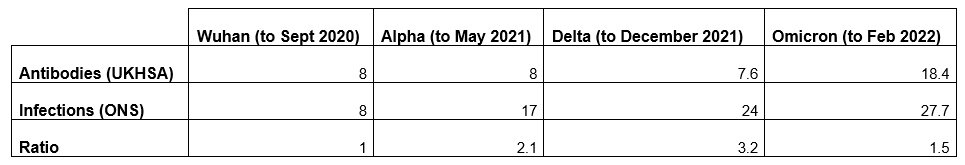
The low ratio of antibodies to infections for Omicron is a strong indicator that the vaccine is no longer inhibiting N-seroconversion. This may be because Omicron is so different to earlier variants; in particular, it has many immune-evading mutations in its spike protein, so that the S-antibodies from the vaccines are largely ineffective against it. This means the immune system must engage with it more comprehensively to fight it off, thus producing N-antibodies. The evasion of S-antibodies, of course, is also why the vaccines do so little to protect against Omicron. The lack of N-seroconversion following infection is likely why many vaccinated people caught Omicron not long after catching Delta. Additionally, the relatively small size of the Omicron wave in South Africa, where vaccination rates are low, adds to the evidence that vaccination played a significant part in driving the Omicron wave in the U.K. and other highly vaccinated countries.
To sum up: antibody surveys appear always to underestimate the number of Covid infections, as a significant proportion fail to seroconvert. This is particularly true following vaccination with vaccines which target a specific protein, such as the current Covid vaccines, though was also true in the pre-vaccination era with the Alpha wave, albeit to a lesser extent. While antibodies are generally a better guide for infections with high viral load, this doesn’t hold following vaccination. Antibody surveys particularly underestimate the size of the Delta wave in populations with high vaccination rates. The vaccine inhibition of N-seroconversion appears to fade with a vaccine-evading variant like Omicron as the wider immune system re-engages.














To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
Based on the evidence it appears to me that virruses do not exist as pathogenic entities, the preponderance of evidence certainly indicates this to be the case.
In which case what is this world of make believe these ‘experts’ have built for themselves trying to explain things that simply are not so because the very foundation of their rational is faulty?
Part 2 of the viral delusion series looks at the series of errors and frauds that have led virologists to believe as they do. It is a 6 part series and well worth a watch, I find their arguements convincing.
The VIRAL DELUSION [EP: 02] ‘MONKEY BUSINESS’ [POLIO, MEASLES & HOW IT ALL BEGAN…’]
https://www.bitchute.com/video/jn9TEz3p5Mcf/
Man who thinks viruses do not exist recommends ‘truth-telling’ video on ‘bitchute’ which includes comments such as:
“This was my question for a long time….my mom got it and had it pretty bad…bad enough my little brother flipped out cuz she refuses to get a shot or go to the doctor because he already told her no for the medicine she needed…we got her the medicine finally and got her detoxing and real supplements…but in the meantime I read everything”
and
“They killed us. Were a nasty evil species that preys on other species without mercy. Goodbye satanic predatory arrogant humanity. It was a nasty mistake to make flesh eating predatory humans. They aren’t spiritual, they’re selfish arrogant demonic creatures.”
The Truth Is Out There (plays music from The X-Files)
In order to criticise a documentary and the information it presents you would of course need to view the documentary first and then present your evidence that showed the content was incorrect.
Have you viewed it?
Yes people can indeed write comments about a documentary on bitchute but the comments neither validate or invalidate the conent of the documentary itself.
To suggest that unsupported comments made about a documentary prove that the information contained within the documentary is fasle would be really rather silly.
If you can present evidence that shows that the content of the documentary is incorrect and that the view you hold is correct as supported by credible scientific evidence then I would abandon my previous position and adopt yours.
https://calmatters.org/health/2021/02/conspiracy-theory-doctor-surrenders-medical-license/
Many thanks for the link. I assume you already know about Virus Mania by Dr Sam Bailey et al?
Dr Sam is a legend.
Yes I have the book Virus Mania it is awesome and should be read in conjunction with Disssolving Illusions by Dr Suzzanne Humphries
I ask again: what agent caused smallpox, and how was it eradicated?
Do you mean the agent did not exist and smallpox is not as advertised?
Genuine question. I’m not familiar with this argument and am curious.
I know that you weren’t replying to me but in answer to your question the book Dissolving Illusions by Dr Suzanne Humphries is an in depth demolition of the the orthodox medical paradigm in that vaccines and antibiotics are not the magnificent stories of the 20th century that transformed our lives.
The book overview –
Not too long ago, lethal infections were feared in the Western world. Since that time, many countries have undergone a transformation from disease cesspools to much safer, healthier habitats. Starting in the mid-1800s, there was a steady drop in deaths from all infectious diseases, decreasing to relatively minor levels by the early 1900s. The history of that transformation involves famine, poverty, filth, lost cures, eugenicist doctrine, individual freedoms versus state might, protests and arrests over vaccine refusal, and much more.Today, we are told that medical interventions increased our lifespan and single-handedly prevented masses of deaths. But is this really true?Dissolving Illusions details facts and figures from long-overlooked medical journals, books, newspapers, and other sources. Using myth-shattering graphs, this book shows that vaccines, antibiotics, and other medical interventions are not responsible for the increase in lifespan and the decline in mortality from infectious diseases. If the medical profession could systematically misinterpret and ignore key historical information, the question must be asked, “What else is ignored and misinterpreted today?”Perhaps the best reason to know our history is so that the worst parts are never repeated.
I have seen the occasional presentation by Dr Humphries on Youtube but they tend to get deleted for expressing wrong think.
Virus Mania is a great work taking things a step further.
The book overview –
“The book ‘Virus Mania’ has been written with the care of a master-craftsman, courageously evaluating the medical establishment, the corporate elites and the powerful government funding institutions.” Wolfgang Weuffen, MD, Professor of Microbiology and Infectious Epidemiology “The book ‘Virus-Wahn’ can be called the first work in which the errors, frauds and general misinformations being spread by official bodies about doubtful or non-virus infections are completely exposed.” Gordon T. Stewart, MD, professor of public health and former WHO advisor – – – The population is terrified by reports of so-called COVID-19, measles, swine flu, SARS, BSE, AIDS or polio. However, the authors of “Virus Mania,” investigative journalist Torsten Engelbrecht, Dr. Claus Köhnlein, MD, Dr. Samantha Bailey, MD, and Dr. Stefano Scoglio, BSc PhD, show that this fearmongering is unfounded and that virus mayhem ignores basic scientific facts: The existence, the pathogenicity and the deadly effects of these agents have never been proven. The book “Virus Mania” will also outline how modern medicine uses dubious indirect lab tools claiming to prove the existence of viruses such as antibody tests and the polymerase chain reaction (PCR). The alleged viruses may be, in fact, also be seen as particles produced by the cells themselves as a consequence of certain stress factors such as drugs. These particles are then “picked up” by antibody and PCR tests and mistakenly interpreted as epidemic-causing viruses. The authors analyze all real causes of the illnesses named COVID-19, avian flu, AIDS or Spanish flu, among them pharmaceuticals, lifestyle drugs, pesticides, heavy metals, pollution, malnutrition and stress. To substantiate it, the authors cite dozens of highly renowned scientists, among them the Nobel laureates Kary Mullis, Barbara McClintock, Walter Gilbert and Sir Frank Macfarlane Burnet as well as microbiologist and Pulitzer Prize winner René Dubos
Thank you for posting. Will read up on it.
I’ve often wondered what the effect was of our general improvement in society e.g. sanitation, diet etc.
I just found this from Dr Humphreys it was on Youtube but was apparently deleted for reasons of wrong think.
She explains how the evidence proves that vaccines did not end smallpox but that improvements in sanitation and nutrition were responsible.
https://odysee.com/@drsuzanneh:f/smallpoxillusionsautismone:9
I can see the sense in this but..but..as Mike Yeadon said in his recent Delingpod interview: without viruses how do you explain disease transmission? Does the Humphries book offer a theory?
How could someone in Iceland succumb to the same sort of illness (I can’t say with confidence the same pathogen as I don’t fully understand the notion) as someone in India or Wuhan?
I can only suggest that you watch the linked video and read the books as the topic is very involved and the different authors offer different perspetives and of course their views alter as they learn more.
Some think viruses exist but are harmless if a host is healthy, some think viruses do not exist but are simply misidentified exosomes, an exosome being a particle of a cell that has broken down due to the cell dying, I am inclined towards the latter.
I have a great deal ofrespect of Dr Yeadon I think he is a brave man. I would ask him prove to me that there is a thing called a virus and that this virus is an independent organism that can be transmitted from person to person and in so doing cause a similar disease to spread, the thing is, in relation to claimed viral illness this has simply never been done for anytype of claimed virus.
A good example is scurvy, which was originally thought to be an infection which spread through ship’s crews but of course we now know it was malnutrition with a simple remedy.
At any given moment there are a lot of people with similar symptoms and it would suggest disease transmission but this could just coincidental and these symptoms are just bodies regaining balance by eliminating unwanted stuff through the lungs, skin and gut etc.
My own experience of being ill is always much the same each time – sore throat, cough and runny nose – irrespective of what-is-going-around. But of course those are often the symptoms that are ‘going around’! And it’s only when you mention your cold that loads of people say they’ve had it too and there-is-a-lot-of-it-about. (Always! With more in the winter and less in the summer).
I reckon that if you have a dodgy test it will find whatever it is you’re looking for no matter what your symptoms (if any) are, and wherever you are in the world.
Malnutrition and filth are the agents that caused smallpox.
I posted the same response to you the last time you asked but sometimes posts do not appear.
Hopefully this one will.
what about chicken pox? It has a very predictable 14 day incubation period, and characteristic symptoms. And I assure you my baby and toddler who caught it were not malnourished or stressed.
I’m open minded on viruses, but it does seem like there is some kind of infectious agent.
There are childhood diseases that are no problem if the child is reasonably healthy. Chickenpox and Measles being very common, and not serious for most children – just two of many ways of cleansing the body.
Healthy bodies will regularly have uncomfortable symptoms. Unhealthy, malnourished or stressed bodies will have more severe symptoms.
Also there is evidence of people who live together tuning in with each other – women’s periods syncronising for instance.
And maybe there is an external trigger for disease – pollen for hay fever, dust for colds, change of season etc etc.
The bottom line being that nothing gives you an illness but your body makes you ill. For a reason.
I think your tin foil hat needs repositioning
If you are going to throw insults about at least make an effort and come up with something original.
Are you sat there with your computer tripple masked and wearing latex gloves to keep yourself safe from a deadly computer virus?
It seems you need a new scriptwriter.
Interesting link which confirms my initial thoughts re covid-2019 as being a perfectly executed global exploitation of ignorance, still running today and so unbelievably successful that a follow-up is probably already in production.
Do any subatomic particles exist? They’ve never been seen only inferred.
Do holes in p-type semiconductors exist? They’ve never been seen only inferred.
What is a force?
It is impossible to prove a positive only a negative, which is why Einstein’s theory of general relativity is always being tested to see where it fails.
As germ theory and domain theory are called theories and not hypotheses there must be evidence for both.
Do any subatomic particles exist?
I don’t know.
Do holes in p-type semiconductors exist?
I don’t know.
What is a force?
You tell me.
I don’t dispute that both germ and terrain theories put forward evidence to support their relative position I am just putting forward information that shows that orthodox medicine is deluded in relation to viral theory.
This is a good presentation with Dr Kaufman where he dissects a video of a virologist and his statements:
Virus-Isolation Is It Real? Andrew Kaufman MD Responds To Jeremy Hammond
https://www.bitchute.com/video/UnpfmjmXNH0O/
The (very small) risk from the original bioweapon strain of SARS-COV-2 was that it caused cytokine storm, an over-blown reaction from our immune systems that killed off our own lung tissue and organs.
Damping that down a bit was the point of the pharmaceutical prophylactic treatments. We didn’t actually need our immune systems trained to fight the virus as such, just not go into full screeching alarm mode when we encountered it.
Now that pretty much everyone has been exposed to variants of it, there’s no further purpose to those treatments. But let’s please not re-invent history for the sake of a headline.
We forget this aspect. The pharmaceutical companies were approached by governments and asked to produce a vaccine quickly. They were immediately told this was impossible, years of work. But they could possibly produce a medical treatment that would dampen the severity of any disease, and may be worthwhile in the vulnerable groups.
I believe it was the Behavioural Insights Team who focus tested various terms and concluded few would take a medical treatment developed at short notice. So it was rebranded using the word “vaccine”. The pharmaceutical companies originally used the term “biological agent”.
Not suggesting any of them are innocent. There was money to be made after all. But I believe we are witnessing the downside of big government primarily, not conspiracy theories in action. They aren’t very good, and they are prone to hijacking because politicians focus myopically on what the audience seem to want and miss important cues.
I don’t go along with this. The pharmaceutical companies had been recruited to the Scamdemic from the beginning i.e. before it allegedly kicked off.
The suggestion that big pharma were recruited to ‘help out’ is laughable. The “vaccines” were brewed to a recipe and the adverse effects that we are now seeing were integral to the recipe. Furthermore, if it was a helping out exercise why were these “vaccines” mandated in many occupations and even some countries?
Governments and the RPTB new early doors that the IFR was only in the region of 0.05% so why the relentless propoganda?
Politicians focusing on what people want? Unfortunately, this too is way off the mark. Politicians are focused on the agenda they have been given and that agenda has bugger all to do with what is best for the people, in fact just the opposite.
All part of the reset.
Not all of them were. Moderna probably, Pfizer possibly. The others, pure opportunism. AZ are regretting ever getting involved.
I think the fact that the people running the scamdemic went to the trouble of assassinating multiple African heads of state who didnt play ball and who expelled the WHO from their countries, with their replacements reversing their truly patriotic policies, puts to bed any “cockup theories” that the in house misdirectors may be promoting
But that being the case why then did they go so hard on supressing the existing and natural treatments? why demonise Ivermectin and Hydroxychloroquinine?
Indeed I have often thought that those who were affected by the virus in this way are arguably the only people to have died FROM covid who would not have died around about this time anyway and are the only people for whom the vaccines might be worthwhile,
though of course this depends on being able to identify those at risk and making sure the vaccines didn’t trigger similar autoimmune responses- things that take time to establish.
The “vaccines”, like Covid, were egregiously oversold.
Thanks Rogerborg. interesting. wouldn’t it be really helpful if some of these BBC science “journalists” could put this about a bit to inform people – but then that wouldn’t sell many vaccines would it?
Please stop writing ‘vaccines’
THEY ARE NOT VACCINES’
They were largely compliance tests in my view. Especially when the government moved on to very low risk groups.
No one could explain why a 25 year old marathon runner should take one, for example. Except for psychological reasons; explicitly excluding one group because of good health opens the floor to others questioning their usefulness. Such is the nature of large scale psychological exercises; they are brittle.
It’s still interesting that china locked down fast and hard and are pursuing 0 covid even though everyone else see’s covid as not that dangerous a thing for non vulnerable groups which is the majority.
what is it that china know that no one else is talking about?
That’s easy. What China knows is obedience is a learned trait, and it requires reinforcement to stick. The most effective form of reinforcement is intermittent reinforcement using a non-predictable schedule.
This is aided by commentators asking, what do they know we don’t? When you do that you skip over the important bit; no one has the right to impede your movements except under very explicit conditions e.g. you are charged with a crime.
Our model is the opposite. Everything is permissible unless explicitly verboten. A little factoid our betters are hoping we will forget.
All these things are about eroding our rights using seemingly plausible excuses. Here in the UK we now know the threat from covid was vastly overstated. This was postulated in February 2020 when scientists analysed the data from the Diamond Princess incident. It was a theory then, albeit using good data from an event that lent itself to this analysis (a floating petri dish with old people). But that theory has since been comprehensively validated. The rest is propaganda.
China is an authoritarian culture. We traditionally are not. It does not suit our character so we require some fluff to make it work. But the underlying dynamic is about power and nothing more. The health aspect, the virus, the response, the drugs and interventions, are just the props to gain power.
It is not clear to me what confident conclusions can be drawn from the study at this stage.
I read a discussion a couple of years among non-sceptical ‘experts’ who said that the widespread use of mRNA treatments would be the biggest medical experiment ever carried out.
The results of that experiment are coming home to roost.
The experiences of the people I know have been worrying to say the least. Some of these had the mRNA treatments and others Astra Zeneca. A couple have had life threatening events and several others less dramatic experiences. Although only a couple of them associate these with the jabs, the number and nature of their experiences suggest a link.
More recently it seems that a majority of the jabbed people I know have tested positive for ‘covid’ or whatever and many have had lengthy colds that they have still not thrown off.
We have one poor woman where I work who was against being jabbed but gave in as she felt pressured to do so, she is now relentlessly ill, always coughing and complaining that she feels lathargic and generally unwell.
She has been like that for months, I assume she was jabbed with mRNA as they were no longer serving up Astra Zeneca by the time she got it.
My sister is like this. Nothing specific, although does seem more prone to colds. But hasn’t been right since the booster.
I’m expecting a lot more of this. The final effect could be the jabbed have shorter lifespans which will take decades to manifest itself. That’s my real fear; not instant death, but reduced quality of life and prone to low level ill health. All difficult to prove of course.
My sister’s are twins; one fully jabbed because she needs to travel, the other has had no jabs because she’s as bloody minded as me. There is no difference in their health. No problem from vaccine; no problem from Covid.
This is, of course, only one pair of twins so we can’t draw a firm conclusion but it’s interesting nevertheless.
I’m in a bit of a quandary. This tells me something I already knew to be true, but this time it’s the US Government’s researchers telling me. In the New World, this does not compute, and my mind has imploded.
Fear not, they will be sacked pronto!
Unless it’s ground prep for Vax MKII with added N protein…
This is fascinating. Perhaps I’m late to the party, but the more I listen to the likes of Drs Cowan, Kaufman and Bailey (Mark Bailey in this instance), and the more I listen to the likes of Drs McCullough, Malone and Cole, the more I notice that the latter do not understand the former’s arguments and are unaware that their (the latter’s) basic, unexamined presuppositions are preventing them from being able to look at the issue objectively:
https://odysee.com/@drsambailey:c/SARS-CoV-2-Bailey-Cowan-Kaufman-respond-to-Cole–McCullough-and-Malone:3
Kaufman is a Grifter, period. Kevin McCairn & Dr Flemming paid for one of his “consultations” (after he was called out for selling a consultation with a medical disclaimer for $1500 and reduced the price to $50) and presented a walkthough of papers showing him the virus had been isolated, including the TEM pictures and protien analysis, Kaufman just kept repeating “I’d have to read the full paper and references” an embarrasing number of times reminisant of Clintons testomony.
You can find it with a bit of effort on McCairns archive https://www.mccairndojo.com/past-episodes/ try searching on Kaufman.
FTR I’ve read Virus maina (both volumes) and watched far too many of the videos from Bailey and the rest of the patrion farmers. Flemming & McCairn make a better case, and can explain the details from experience, unlike any of the patrion farmers/Book promoters.
Calling people ‘Grifters’, ‘patrion [sic] farmers’ and offering a vague reference does nothing to refute anything. I’m not invested in any way in denying the existence of disease causing viruses, but you’re going to have to do a lot better than smearing these people if you’re looking to convince anyone that they’re wrong.
I’m not “refuting” anything, McCairn is a Neuro Scientist, Flemming is an MD and PhD, they do the refuting, I only pointed you to their stream.
Andrew “I’ve never worked with Viruses” Kaufman needs no qualification to be a grifter, and you need non to discover this, just look at his website shop, then search Amazon for regular prices of that resin stuff he’s selling for 10 x the regular price, it was more obvious when he was selling “consultations” (with a medical disclaimer) for $1500 an hour. A fool and his money…
I’m not trying to convince you of anything, it’s pointless with die hard terrain theory proponents who accept the theory without any questions regarding their own experience with transmission of diseases, it’s your choice to seek truth, or not. I read all the virus mania stuff, watched hours of the GNM stuff, and find it all less than convincing because they get transmission all wrong IMO.
See Dan Sirotkins theory of “Viral Swarms” for something that can bridge both terrain and germ theory, it cover the “transmission” holes in terrain quite nicely.
You gave me a vague reference.
Okay, let’s grant he’s a grifter. Improper ad hominem. How does that negate his arguments?
Do you have a reading comprehension issue? I said:
You seem to be emotionally invested here. Slow down and read what others are saying.
Which begs the question by assuming that which is in dispute.
Funnily enough, you are exhibiting the exact traits the doctors highlight in the video I shared.
That’s a silly attempt at piousness, and it is meaningless. It’s a diversion.
Terrific.
Okay.
It’s a logical deduction, if there’s no viruses, there can be no transmission.
Unless you have another theory about transmission without a virus/germ?
Do you? lets not bother with THAT level of nonsense eh
1)click the link, 2)enter “Kaufman” in the search box, 3)watch stream
is this too hard?
And again, you are begging the question by assuming transmission. I’m not saying you’re wrong, but you are assuming the very thing being disputed. You are exhibiting the exact traits highlighted in the video, and you are blissfully unaware. This is bizarre.
do you have another hypothesis for transmission or not?
Are you dense? ‘Transmission of virus’ is the very thing being disputed by those who deny or question the existence of disease causing virus particles. Saying ‘do you have another hypothesis for transmission’ yet again begs the very question in play. And again, I’m not the one making the arguments. You have a serious reading comprehension issue.
Just when I thought you couldn’t embarrass yourself further you go and make yourself look like even more of a berk
It is not nonsense when you are clearly overemotional and not reading what I am saying!
Moreover, that’s a bit rich coming from the person who engages in the nonsense/pseudo piousness of ‘it’s your choice to seek truth, or not’!
It’s official. You’re dense. Many videos pop up when you type ‘Kaufman’ into the search bar.
You’re a shirker.
correction: it was $1750 not $1500
you know Kaufmans been stuck off twice right?
https://neilsandersmindcontrol.com/index.php/blog/covid-misconceptions-debunked
That article is an absolute mess. It is a pro-PCR, pro-mask, anti-‘alt media’ propaganda piece aimed at smearing opponents, and again, it does nothing to disprove the doctors’ arguments outlined in the video I presented.
For example:
Once again, this is an issue addressed in the video, and you’re just begging the question. You didn’t even watch the video, did you?
does it contain the words I quoted?
Does it contain the evidence kaufman is a grifter?
OK job done then.
The refutation is on the McCairn link
No, it is not ‘job done’ at all since, granting Kaufman is a grifter, this does nothing to refute his arguments, and you are engaging in an improper ad hominem argument.
Blatant lies from your source:
Absolute complete and utter bullcrap, even according to official sources which put SARS COV 2 fatality rate at around 0.2percent. He also conveniently fails to mention that in the HCID document published by GOVUK, they cite low mortality rates as the primary rationale for the downgrade.
https://www.gov.uk/guidance/high-consequence-infectious-diseases-hcid#status-of-covid-19
More likely to be infected multiple times? What can we do to protect our jabbed elderly and the unvaccinated against the menace of the triple jabbed, going about spreading this KILLER DISEASE several times a year?!
Also this
https://www.sciencedirect.com/science/article/pii/S027869152200206X
Apologies if it has been referred to before on D.S.
That said, I have no doubt that UKHSA and vaccine regulatory bodies have read it, absorbed it and understood it.
I thus await the vax for kids at least to be withdrawn. Lol.
The vax for kids is not about science or health. It is about continuing a narrative which itself has many benefits for those who wish to rule us. Why would they withdraw that?
The worst thing about this ‘discovery’ is that it’s not new information. El gato malo discusses this study in article dated 27 April and points out that the data is from murderna’s actual phase 3 trial – i.e. this data was available prior to the vaxx roll-out.
In addition, the UKHSA vaccine surveillance report notes in every weekly report that double vaxxed have a poorer N-antibody response than unvaxxed, but say they don’t know why – from week 17 2022:
“(ii) observations from UKHSA surveillance data that N antibody levels are lower in individuals who acquire infection following 2 doses of vaccination. These lower N antibody responses in individuals with breakthrough infections (post-vaccination) compared to primary infection likely reflect the shorter and milder infections in these patients.”
The last sentence is pure speculation.
It was known before vaxx roll-out that there was the unexplained lack of N-antibodies in vaxxed compared to unvaxxed. They have been noting this week after week in the official UK vaxx surveillance reports, still claiming no knowledge of *why* this is happening, other than guesswork. And still they insist on pushing ahead with boosters, with most countries planning a 5th shot for the fall.
It’s one or the other – they either know full well that this toxic sludge causes immune suppression and are imo guilty of criminal negligence by continuing, or they really have zero clue what is going on – and by nevertheless still pressing ahead, are imo guilty of criminal negligence. And this they call ‘science’.
Natural News) The official US embassy website recently REMOVED all evidence of bio-labs in Ukraine. These bio-labs are funded and jointly operated by the US Department of Defense (DOD). The laboratory documents were public knowledge up until February 25, 2022. These documents include important construction, financing and permit details for bioweapon laboratories in Ukraine. But now the US government is scrubbing these documents from the internet and becoming less transparent with this critical information. This comes at a time when the world population is waking up to the reality of gain-of-function bioweapons research, lab leaks and predatory vaccine and diagnostics development. These bio-labs generate pathogens of pandemic potential that exploit human immune systems and are the foundation for which medical fraud, malpractice, vaccine-induced death and genocide originates.
Every day more evidence of the clear and present danger posed to human health by the Poison Gene Therapy Experimental ‘Vaccines’ emerges and is simply ignored or censored by a Government machine and our Health Care Institutions – still vaccinating children.
How can anyone even begin to explain the Gross Moral Turpitude and betrayal of their absolute ‘duty of care’ that this manifest evil represents on the part of the entire Government Elite?
So how come it is being allowed to continue without even a whimper from MPs -too busy perhaps watching porn in the Commons, changing their gender unable to define a ‘woman ‘and waving Ukraine flags to be the least “bovvered” ?
And what is the political message for what is left of the intelligent section of the electorate, who can still be bothered to vote for these dangerous charlatans?
But do get another jab.
Unfortunately my Mum probably will. Because she is, regrettably, a bit naive, and far too trusting of authority.
Mask Study Finds No Impact on Covid Infections From Mask-Wearing and an INCREASE in Deaths
https://dailysceptic.org/2022/04/30/mask-study-finds-no-impact-on-covid-infections-from-mask-wearing-and-an-increase-in-deaths/
By Will Jones
Stand for freedom with our Yellow Boards By The Road next events
Monday 2nd May 2pm to 3pm
Yellow Boards
Junction A3095 Foresters Way &
B3430 Nile Mile Ride
Bracknell RG40 3DR
Thursday 5th May 5.30pm to 6.30pm
Yellow Boards
A4130 White Hill (between Henley Bridge
& A321 Wargrave Road)
Henley-on-Thames RG9 2LP
Saturday 7th May 3pm to 5pm
Yellow Boards LONDON
Junction Victoria St/Bressenden Place
London SW1E 5NA
Stand in the Park Sundays from 10am – make friends & keep sane
Wokingham
Howard Palmer Gardens
(Cockpit Path car park free on Sunday)
Sturges Rd RG40 2HD
Bracknell
South Hill Park, Rear Lawn, RG12 7PA
Telegram http://t.me/astandintheparkbracknell
That’s rather a nice finding. The vaccines are so useless against Omicron, that the body has to start providing the protection it was prevented from doing by the vaccine. So the uselessness of the vaccine engenders a more healthy outcome.
What does this mean for patients receiving blood donations?
Commonsense would suggest that unjabbed patients would want to receive blood only from unjabbed donors.
Any ideas on this, anyone?
I asked this question many months ago and didn’t get a reply.
It is scary to think that being sensible and unjabbed you could have ‘spiked blood’ transfused should you require it, say, after an accident.
Seems the more jabs you have the more times you get Covid. Not been jabbed, don’t do masks and I’ve never had it.
Prior to the jab roll-out I didn’t know a single person who had the ‘rona. However since then I know loads of people who have had ‘it’. I have pointed out that the tests are dodgy and non-specific for ‘rona19 but they are all determined that they have ‘it’.
Why only 52 people in one arm of the trial and 600 in the other? This reduces the credibility of the paper for me.
The medical technocrats have focussed on The Spike as it is readily targetted by patentable drugs. But how does the normal unimapired immune system actually work against SARS-CoV-19? My guess is that there is a multi-faceted response that enables rapid mutation to be dealt with. But who knows? Has there been any real research done on how the immune system really works against something like SARS-CoV-19?
You either follow the scientific view, by “experts” who were not experts prior to Covid-19, in 2019 – or you do my simple cure – it is as simple as that: 3 minutes from preparation to job done!!
Everything else you have read, or heard, is totally irrelevant – how simple is that?
Covid Crusher: Mix one heaped teaspoon of Iodine table salt in a mug of warm clean water, cup a hand and sniff or snort the entire mugful up your nose, spitting out anything which comes down into your mouth. If sore, then you have a virus, so continue morning noon and night, or more often if you want, until the soreness goes away (2-3 minutes) then blow out your nose and flush away, washing your hands afterwards, until when you do my simple cure, you don’t have any soreness at all, when you flush – job done. Also swallow a couple of mouthfuls of salt water and if you have burning in your lungs, salt killing virus and pneumonia, there too.
My simple salt water cure, kills all Coronaviruses and viruses, as soon as you think you have an infection, or while self isolating, before the viruses mutate into the disease in your head and body, for which there is no cure – that is, after you have been out shopping, or mixing with people with potentially, Omicron or Delta viruses, or any other virus.
It washes behind the eyes, the brain bulb, brain stem (Long Covid), The Escutcheon Tubes to the inner ears and the top of the throat which is at a point roughly level with half way up your ears and not where your mouth is and down the back of your throat, when sore.
I have been doing this simple cure for over 28.5 years and I am and others, never sick from viruses and there is no reason why any of you should be either – when your only alternative are those vaccines!!
I do my simple preparation, after I have been out and about, or come into contact with people who have been vaccinated – it has kept me safe – and I hope it keeps me safe for the foreseeable future as Graphene Oxide is in the very air we breathe, outside, as well, but now from the vaccinated!!
Simply put, if the inside of your nose is dry and crusty, you are OK, if your nose is runny, you really need to do a salt water sniffle as quickly as possible and monitor the results, to see if further salt water sniffles are necessary, but later on in that evening – so far – I remain immune from potential Covid infections, doing just this.
No vaccines for me – ever – what have you got to lose, apart from your life?
Richard