The Government on Wednesday published the evidence informing its recent controversial decision to recommend all secondary school pupils wear face masks in classrooms.
The new document from the Department for Education (DfE) explains that the decision “has been taken on the recommendation of UKHSA and is based on a range of evidence”. It says the Government has “balanced education and public health considerations, including the benefits in managing infection and transmission, against any educational and wider health and wellbeing impacts from the recommended use of face coverings”.
While conceding that the “direct COVID-19 health risks to children and young people are very low” – and rejecting SAGE’s advice to recommend masks in primary school classrooms (yes, really) – it claims that “the balance of risks for secondary classrooms has changed at this point in time, in accordance with the evolving evidence and the phase of the pandemic”.
The document summarises its evidence as follows:
Face coverings can be effective in contributing to reducing transmission of COVID-19 in public and community settings. This is informed by a range of research, including randomised control trials, contact tracing studies, and observational studies – assessed most recently by UKHSA, described in a review conducted in November 2021. The review’s conclusions were broadly in line with those of a previous Public Health England review; however, the addition of randomised control trials and substantially more individual-level observational studies increases the strength of the conclusions and strengthens the evidence for the effectiveness of face coverings in reducing the spread of COVID-19 in the community, through source control, wearer protection, and universal masking.
In fact, though, the UKHSA review from November 2021 found no high quality studies (except, it claims, the ONS study, which really isn’t high quality). Of the two randomised controlled trials (RCTs) that have been done and which were cited by the UKHSA, the one from Denmark found no statistically significant reduction in COVID-19 incidence from surgical masks (the study didn’t look at cloth masks) while the Bangladesh mask study found no benefit from cloth masks and the reported benefit from surgical masks was just 11%, with a 95% confidence interval that included zero. The UKHSA review also considered 23 observational studies, which it said had “mixed” results and many of which were of low quality and small.
This does not seem a strong basis to claim a large effect for mask wearing. A recent more comprehensive review (which included earlier evidence for other flu-like viruses) by Ian Liu, Vinay Prasad and Jonathan Darrow for the Cato Institute, entitled “Evidence for Community Cloth Face Masking to Limit the Spread of SARS‐CoV‑2: A Critical Review“, concluded that: “More than a century after the 1918 influenza pandemic, examination of the efficacy of masks has produced a large volume of mostly low- to moderate-quality evidence that has largely failed to demonstrate their value in most settings.”
That is a better summary of the evidence than the DfE managed.
Needless to say, the DfE gives the propaganda value of masking a nod: “It can be a visible outward signal of safety behaviour and a reminder of COVID-19 risks.”
Notably, there is no mention in this document of the potential harms of wearing a mask for an extended period, such as the impact on breathing, the heart, or the skin. Contamination gets a brief mention, though it’s quickly dismissed:
Face masks and coverings will become highly contaminated with upper respiratory tract and skin micro-organisms. Disposal of single-use face coverings could theoretically pose a risk of transmission for inappropriately discarded face coverings, but it is very likely that the reduction in transmission risk due to reduced droplet and aerosol emissions from wearing a face covering significantly outweighs any potential for enhanced risk of transmission through inadvertent contact with a contaminated face covering. This is likely to hold regardless of duration that the face covering is used.
The reference provided for these claims is a SAGE document from September 2020, “Duration of Wearing of Face Coverings.” This is an interesting document, but it can scarcely be said to support the claims the DfE is making. On harms from masks, for example, it says:
Neither surgical masks nor face coverings are designed for use for extended periods. Wearing a face covering for an extended period can maintain a higher moisture level around the face which can be uncomfortable for some people and may increase the likelihood of skin complaints. Masks will become highly contaminated with upper respiratory tract and skin micro-organisms. A review of the downsides of face masks and face coverings (by Bakhit et al) found 20 studies reporting irritation and discomfort from using masks. Participants in studies with surgical or cloth masks reported difficulty breathing (12%-34%), facial irritation and discomfort (11-35%). More serious symptoms of headache, acne, rashes were associated with use of N95 and goggles. A study among healthcare workers (by Han et al) associates acne with extended duration of wearing. …
In a clinical study of extended wearing (by Chughtai et al), 124/148 participants reported at least one problem associated with mask use including pressure on face, breathing difficulty, discomfort, trouble communicating with the patient and headache. …
Measurements of heart rate during activity (by Li et al) showed significantly lower rates with a surgical mask compared to N95. In a study (by Fikenzer et al) of healthy young male volunteers surgical masks and FFP2/N95 respirators, both had a significantly marked negative impact on pulmonary capacity (FEV, PEV and PEF) while wearing the mask (with a spirometry mask) during exercise.
The DfE document omits to mention any of these issues. It does, however, include some recognition of the negative impact on education. It mentions a survey conducted by the Department in March 2021 that found “80% of pupils reported that wearing a face covering made it difficult to communicate, and more than half felt wearing one made learning more difficult (55%)”. It also mentions a DfE survey from April 2021 that found “almost all secondary leaders and teachers (94%) thought that wearing face coverings has made communication between teachers and students more difficult, with 59% saying it has made it a lot more difficult”. It adds:
Research into the effect of mask wearing on communication has found that concealing a speaker’s lips led to lower performance, lower confidence scores, and increased perceived effort on the part of the listener. Moreover, meta-cognitive monitoring was worse when listening in these conditions compared with listening to an unmasked talker. A survey of impacts on communication with mask wearing in adults reported that face coverings negatively impact hearing, understanding, engagement, and feelings of connection with the speaker. People with hearing loss were impacted more than those without hearing loss. The inability to see facial expressions and to read lips have a major impact on speech understanding for those with hearing impairments. The worse the hearing, the greater the impact of the mask.
What about the evidence for the claims the document does make – that it is “very likely” that the transmission reduction from wearing a mask “significantly outweighs any potential for enhanced risk of transmission through inadvertent contact with a contaminated face covering” and that “this is likely to hold regardless of duration that the face covering is used”. This is what the cited SAGE document says:
There is a lack of good evidence relating to the wearing of face coverings, with very little data relating to duration of wearing. In particular we suggest that the following aspects would benefit from further research:
• Effectiveness of face coverings as a source control after longer duration wearing, including analysis of the influence of moisture on the performance of different types of face coverings.
• Analysis of the potential risk of transmission due to contaminated face coverings (during and after removal).
• Assessment of the prevalence of skin complaints associated with face coverings, including an understanding of the factors that contribute and potential mitigation.
• Analysis of user acceptability of face coverings for long duration use in different settings.
In other words, there was no good evidence on the things the DfE is claiming are “likely” or “very likely”, or on much else really.
The DfE also carried out its own analysis of the impact of masks in schools.
DfE has also undertaken initial observational analysis based on data reported by 123 secondary schools that implemented face coverings during a 2-3-week period in the autumn term 2021, compared to a sample of similar schools that did not. The preliminary findings demonstrate a potential positive effect in reducing pupil absence due to COVID-19.
What did it find? It found that COVID-19 absences fell by 0.6% more (absolute reduction) in secondary schools that used face masks compared to similar schools that did not over a 2-3-week period, which amounts to an 11% relative reduction.
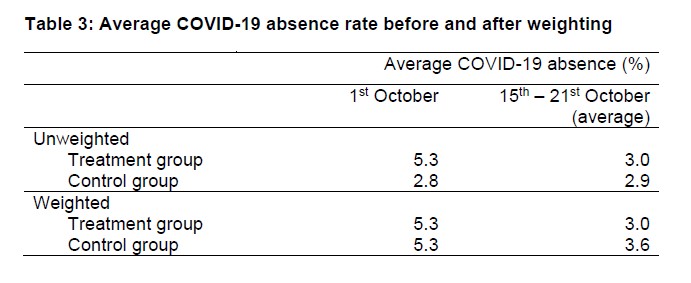
In a weighted sample of secondary schools that did not use face masks, the average COVID-19 absence rate fell by 1.7 percentage points from 5.3% on October 1st 2021 to 3.6% in the third week of October. This is equivalent to a 32% decrease.
In secondary schools that did use face coverings (either face coverings only or a combination of face masks and additional communications e.g. providing more communications to parents but not introducing any further measures such as increased testing), the average COVID-19 absence rate fell by 2.3 percentage points from 5.3% on October 1st 2021 to 3.0% in the third week of October. This is equivalent to a 43% decrease.
At surface level, this suggests that COVID-19 absence fell by 0.6 percentage points more (an 11% relative difference) in secondary schools that used face masks compared to similar schools that did not over a 2-3-week period.
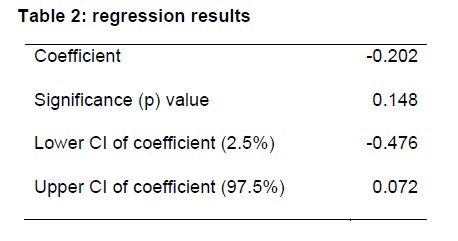
However, the study had numerous limitations, which made the finding a “non-statistical and unknown clinical significant” reduction, i.e., it may just be chance.
There is a level of statistical uncertainty around the result. The analysis is non-peer reviewed and with the current sample size, shows a non-statistical and unknown clinical significant reduction in infection in a short follow up period, including that a ‘false positive’ (i.e. finding that face coverings saw reduced absence when the finding is actually by chance) would emerge around 15% of the time; a 5% threshold is widely used to declare statistical significance in academic literature.
Therefore, further work should be done to extend the analysis in terms of scope: for example, looking at different statistical methodologies, capturing different and longer treatment time periods and controlling for a wider number of school and local area variables to ensure this is a consistent finding.
The statistical uncertainty around the result was such that the 95% confidence interval for the effect size included zero (note in the below the upper CI is positive).
What’s more, the control group of 1,192 schools that didn’t use masks were very different to the 123 treatment schools which did, so that the above findings only emerged after substantial weighting was added to the control group schools using a process the document calls “entropy balancing”.
Exploration of the data showed that the control and treatment group had differing characteristics, so weights for the control group schools were calculated using entropy balancing.
Prior to this weighting, the non-mask schools actually had lower average absence rates throughout the study period – though the treatment schools reduced more from their higher starting point.
Prior to weighting, the mean absence rate of the control group increases across the treatment period, whereas the mean absence rate of the treatment group decreases. However, the absence rates in the control group remain lower overall than those in the treatment group.
All-in-all, not exactly robust, compelling evidence of the benefits of masking, particularly given all the well-documented harms, which the document itself either sets out or cites other documents which do.
The document at one point hints at what I suspect is the real reason masks were brought back into classrooms: “In a Unison survey of support staff, 71% said face coverings in secondary school classrooms are an important safety measure.” Conservative MP Jonathan Gullis wrote in the Times this week that: “Face masks have been a central demand of teaching unions.” Sounds vey much like politics rather than science to me. (See this recent Daily Sceptic article by Ben Irvine on the role the teaching unions played in forcing the Government to lockdown in March 2020.)
When are we going to stop harming our young people with pointless interventions to deal with a virus that poses no threat to them and let them live normal lives again?
Stop Press: Oxford Professor of Evidence Based Medicine Carl Heneghan tells Julia Hartley-Brewer he is unimpressed by the Government’s “evidence” for masking in classrooms.
Stop Press 2: The Telegraph reports that some schoolchildren are rebelling. According to Damien McNulty, a national executive member of the National Association of Schoolmasters Union of Women Teachers: “Sadly, we have had reports in the last 24 hours of at least six secondary schools in the north-west of England where children, in huge numbers, are refusing to take lateral flow tests or to wear masks. We’ve got one school in Lancashire where only 67 children out of 1,300 [5%] are prepared to have a lateral flow test and wear masks. This is a public health emergency.” Hats off to these young people for standing up for themselves against the unions and authorities who would force them to do harmful and pointless things. May their rebellion grow!












To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.