An important pre-print was published last week by Public Health Scotland looking at how all 204,913 people eligible for shielding (the “clinically extremely vulnerable”) – about 3% of the population – have fared during the COVID-19 pandemic. The researchers matched all 160,307 positive cases of COVID-19 (as of January 28th) to individuals in Scotland to form a complete picture of the course of their illness in order to evaluate the effectiveness of the shielding programme.
Their striking conclusion was they found “no evidence that the shielding programme per se reduced COVID-19 rates”, though they allowed for the possibility that “without shielding advice and support the outcome in this group would have been worse”.
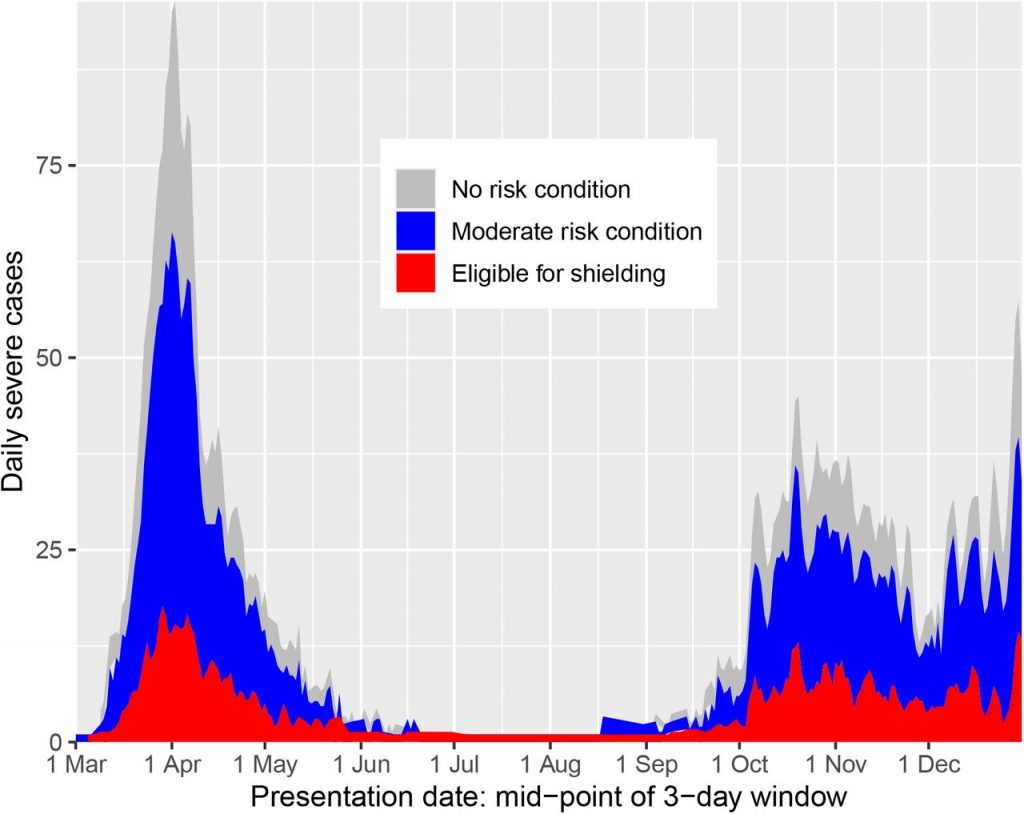
People eligible for shielding were 7.6 times more likely to have a severe case of COVID-19 (defined as requiring intensive care or dying) than the general population with no risk condition (care home residents were excluded from the analysis). This rose to 13.6 times more likely in solid organ transplant recipients (whose immune systems are suppressed by drugs to assist acceptance of the transplant).
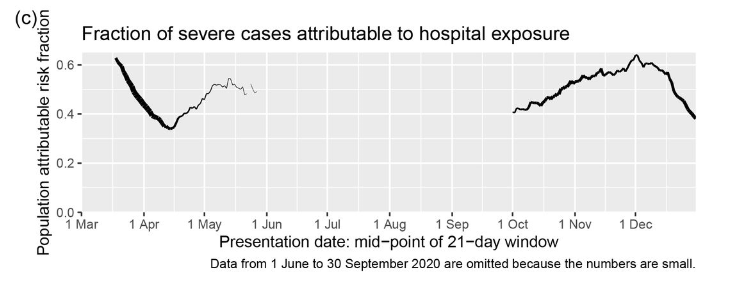
The main problem for shielding was the high rate of infection acquired in hospital, an environment the clinically extremely vulnerable can scarcely avoid. Thirty-six percent of severe Covid cases among this group were linked to recent hospital exposure. This compared to around 50% of severe cases in the general population, peaking at 64% or almost two thirds in December (see graph above). Sharing a household with other (non-shielding) adults was also a major risk factor – again, hard to avoid.
They write:
We have identified two sources of exposure that are associated with severe disease and cannot easily be avoided by those advised to shield: in-patient hospital care, and sharing a household with other adults. We recommend that consideration should be given to special measures to allow these vulnerable individuals to reduce their exposure. This could include special measures to protect these individuals from nosocomial infection, and support for other household members to co-isolate with the vulnerable individual.
The study shows once more the extent to which COVID-19 is a disease caught in hospital, particularly those who have a severe course or die. Since we know from elsewhere that up to 40% of Covid deaths are among care home residents, infections acquired in hospitals and care homes, when added together, account for a substantial majority of COVID-19 deaths. This helps explain why lockdowns, despite the intuitive logic of keeping people apart, are consistently found to have little or no relationship to mortality or infection rates.
The study also underlines the challenges of focused protection of the vulnerable as advocated by the Great Barrington Declaration, with shielding even under lockdown conditions proving difficult. On the other hand, by showing that lockdowns don’t help (and elucidating why), it makes plain that resources should be put into protecting the vulnerable as far as that is feasible and not into confining the healthy population.











To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
The article shows the futility of interventions in the spread of flu-like illness. A far bigger worry for transplant/immune-compromised patients is the resistant bacteria being created through chronic use of unregulated hand sanitizers.
my medic researcher wife is very worried about this. wont use the hand sanitisers or let the kids. says handwashing alone is good enough
Good old soap! (Who’d ‘ve thunk it?)
Agree, I haven’t use the rubbish for months
Hand sanitizer, that is.
Indeed, its not exactly new or novel is it?
They knew full well before they started fire hosing sanitiser about what would happen, this article is from 2018:
“In the early 2000s, hospitals across Australia began installing more hand-sanitizer dispensers in their rooms and hallways for staff, visitors and patients to use. Research showed these alcohol-based disinfectants helped battle staph infections in patients and certain kinds of drug-resistant bacteria. And rates of these infections went down.
But other infections didn’t drop when people started using the sanitizer stations. In fact, certain infections went up.
In particular, enterococcal infections — caused by bacteria that affect the digestive tract, bladder, heart and other parts of the body — started increasing.”
https://www.npr.org/sections/goatsandsoda/2018/08/02/635017716/some-bacteria-are-becoming-more-tolerant-of-hand-sanitizers-study-finds?t=1611846494692&t=1612447906319
The link “fro elsewhere” to the ons site is giving a 404 error.
Looks like the URL was incomplete.
And excellent piece. Links a lot of threads of information on lockdowns and their effects together.
It makes a very strong case for no more lockdowns and why on earth vaccine passports have anything to do with solving the issues outlined here I have no idea. Unless it was never about a virus
“infections acquired in hospitals and care homes, when added together, account for a substantial majority of COVID-19 deaths”
NHS and PHE are really not fit for purpose
Lockdown just slows the gaining of immunity by the wider community that would then shield the more vulnerable. Imperial modelling suggests that lockdown causes more deaths than non-lockdown from covid – let alone the lockdown deaths
Add in schools and universities and you have about 100%. Hospitality has been hung out to dry.
Its been the case over recent years that unless their is a dire need, the last place to go if you want to stay healthy is a hospital. The covid numbers just show how this is even more true for respiratory illnesses.
This is not about a virus, never has been. Its about changing society to allow the resource constrained capitalism to take place under a biosecure fascist totalitarian regime. Many anglosphere countries are well on their way, but there are issues about splits in the US and Europe.
Re. Your second paragraph and the NWO. There’s a good piece on this in yesterdays Off-Guardian:
The New Normal (Phase 2)
https://off-guardian.org/2021/03/09/73943/
Underlying the fact that Covid is a nosocomial infection.
As highlighted on here and by Yeadon et al months ago.
The longer this farce progresses, the more right the Great Barrington Declaration’s proposals appear.
Worth noting that the only hospitals to get their Nosocomial infection rate down to statistical zero were those in Singapore last year, which proceeded on the assumption that Covid is primarily contact transferred through oro-foecal contamination, same as polio or Norovirus.
They went absolutely rabid on proper soap n water handwashing.
It worked – go figure as the USians say.
https://market-ticker.org/cgi-ticker/akcs-www?post=239747
The lesson one can draw is that neither GBD nor the official policy-which, after all, includes shielding, can work well. Shielding properly would need identification, effort and resources, all of which are being misdirected or squandered in a generalist approach. The age structure and vulnerability (ie co-morbities, obesity & diabetes) were known from Italy a year ago. The tragedy is that no lessons were learned then and few now.
Given the well-know BME propensity for diabetes and the significantly worse health of Asian elders, shielding here would mean deliberately breaking up the extended family. This would have to be done by compulsion-and good luck with that.
Although Prof. Whitty acknowledged that infections were slowing before lockdown he insists that opening up after May 17th (my birthday!) is a grave risk. He cannot have been looking at the US states which have reopened and can be compared to (often neighbouring) ones with stringent measures. Doubling down on an error is a very human mistake and it will cost us dear unless we end the obsession with lockdown. As the 2011/14 Influenza Prep. Plan outlined, a generalist approach cannot work. That we knew this is another tragedy and why however disheartening it can be ‘la lutta continua.’.
Does anyone know how I can locate the round up from previous days? It no longer seems to appear on the relevant days update?
Having A Laugh