In a recent article, I noted that vaccine effectiveness against death may have been overestimated due to the ‘healthy vaccinee’ effect – the tendency for people who get vaccinated to be healthier and more risk-averse than those who don’t.
Likewise, Will Jones recently reported on a large Swedish study, which observed declining effectiveness against severe outcomes, particularly after six months. Discouragingly, the decline in effectiveness was most pronounced among older, frail individuals – the group most at risk from Covid.
Now a new study (which hasn’t yet been peer-reviewed) has made a similar finding. Maxime Taquet and colleagues analysed data from a large database of electronic health records in the U.S.
Their sample comprised ~19,000 individuals who’d had a confirmed SARS-CoV-2 infection between January 1st and August 31st 2021. There were two groups: those who had been vaccinated at least 14 days prior to infection, and those who had not been vaccinated prior to infection.
The two groups were matched not only on basic demographic characteristics, but also on a large number of medical risk factors. In addition, the unvaccinated individuals were selected from among those who’d ever received a flu vaccine. Overall, substantial efforts were made to ensure the two groups were comparable.
Taquet and colleagues’ main finding is shown in the figure below. The lines on each chart show the cumulative probability of death for vaccinated and unvaccinated people, respectively. (Note: they also looked at other severe outcomes; see Fig. 3.)
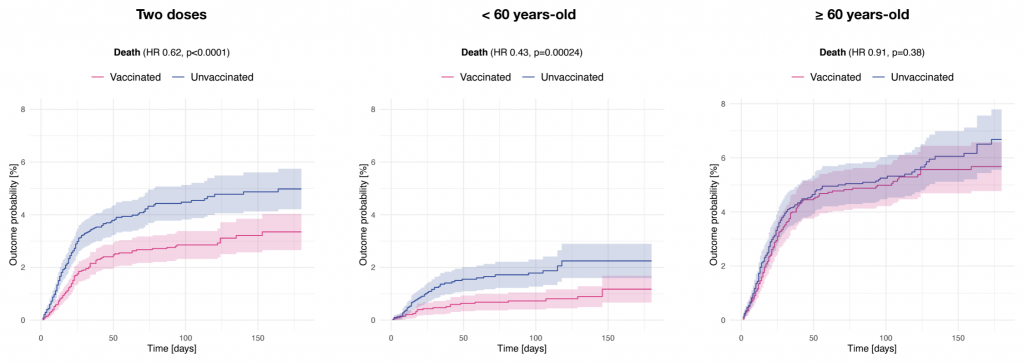
The chart on the left indicates that, on average, vaccinated people had a lower risk of death than unvaccinated people. However, as the other two charts indicate, this difference was seen primarily in those under 60. Among those over 60, it was small and not statistically significant. The authors note:
Receiving 2 vaccine doses was associated with lower risks for most outcomes. Associations between prior vaccination and outcomes of SARS-CoV-2 infection were marked in those < 60 years-old, whereas no robust associations were observed in those ≥ 60 years-old.
Why would vaccination have a stronger effect among those under 60? The researchers speculate that:
In younger patients, effective B-cell response to vaccination might be followed by infection with variants against which antibodies have less neutralising activity … In older patients, the B-cell response to vaccination might itself be ineffective
It’s important to keep in mind that their finding concerns the risk of death conditional on SARS-CoV-2 infection. To the extent to that the vaccine protects against infection, it will protect against serious illness and death too.
However, it’s still noteworthy that effectiveness against death in over 60s was minimal among those who had been infected. Of course, this is just one study, so it shouldn’t be given too much credence. But the researchers did make substantial efforts to ensure the two groups were comparable and thereby obviate the ‘healthy vaccinee’ effect.
If their finding is true, it would suggest that previous observational studies have overestimated vaccine effectiveness against severe outcomes in older age-groups. It would also suggest that most of the protective effect for these age-groups comes from immunity against infection, which we know wanes rapidly in the absence of boosters.
The evidence from Taquet and colleagues’ paper could therefore be taken as supporting voluntary boosters for high-risk groups, as well as the continued build-up of natural immunity in the rest of the population.











To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.