A new study published this week adds to the evidence that social distancing rules like the two-metre, one-metre-plus and six-foot rules offer no additional protection against COVID-19.
Professors Martin Bazant and John Bush from the Massachusetts Institute of Technology use mathematical modelling to show that the risk of catching the virus is unaffected by keeping your distance from infected people when in the same room because of the way the virus spreads via aerosols in the air.
Prof Bazant told CNBC that the six-foot rule “really has no physical basis because the air a person is breathing while wearing a mask tends to rise and comes down elsewhere in the room so you’re more exposed to the average background than you are to a person at a distance”.
While distancing offers some protection against larger droplets, it offers none against aerosols, which are a very common mode of transmission.
The peer-reviewed study, published in the Proceedings of the National Academy of Sciences of the USA, uses a model to calculate indoor exposure risk based on time spent inside, air filtration and circulation, immunisations, respiratory activity, variants and mask use. Their conclusion is that it’s not social distancing that reduces risk but primarily the amount of time people spend in an enclosed space. The authors advise in the paper:
To minimise risk of infection, one should avoid spending extended periods in highly populated areas. One is safer in rooms with large volume and high ventilation rates. One is at greater risk in rooms where people are exerting themselves in such a way as to increase their respiration rate and pathogen output, for example, by exercising, singing, or shouting.
Prof Bazant explains in his CNBC interview that this means many venues that have been closed can reopen at full capacity without increasing exposure risk.
What our analysis continues to show is that many spaces that have been shut down in fact don’t need to be. Often times the space is large enough, the ventilation is good enough, the amount of time people spend together is such that those spaces can be safely operated even at full capacity and the scientific support for reduced capacity in those spaces is really not very good. I think if you run the numbers, even right now for many types of spaces you’d find that there is not a need for occupancy restrictions.
The authors suggest that instead of an exposed person being defined as someone who has been within six feet of an infected person for more than 15 minutes (as per the current CDC definition), whole rooms should be considered to be exposed depending on whether or not they exceed their cumulative exposure time (CET) with the infected person.
This does seem to be a more scientifically credible definition of exposure, but it also invites the possibility of yet more public health tyranny. And indeed, the authors propose regular mass testing at a frequency regulated by the CET for the space in question – and they’ve helpfully provided an app to enable us to calculate that. They explain:
For a group sharing an indoor space intermittently, for example, office coworkers or classmates, regular testing should be done with a frequency that ensures that the CET between tests is less than the limit set by the guideline.
The need for this mass testing arises because they assume in their model that asymptomatic infections are no less infectious than symptomatic infections, so that simply asking people to isolate when ill is not enough to prevent exposure. Yet it is well-established now that asymptomatic infection is considerably less infectious than symptomatic infection and contributes very little to spread.
It’s worth stressing, then, that this is very much a model, not a study of real world transmission data and patterns, so is highly dependent on the assumptions and parameters that go into it. Some of those assumptions are more sound than others.
The assumptions relating to masks, for instance, are highly dubious.
The model tells you that if a restaurant with 50 people in it includes one infected person then people should spend less than 40 minutes there to avoid being infected. But if they are all wearing masks then this would be 28 hours! How does it arrive at that incredible difference?
The authors state that surgical masks filter out 95-99% of aerosol droplets. To back up this claim they refer to two papers. The first says it found the mask filtered out 30-75% of aerosol droplets and concludes: “Although surgical mask media may be adequate to remove bacteria exhaled or expelled by health care workers, they may not be sufficient to remove the submicrometer-size aerosols containing pathogens to which these health care workers are potentially exposed.” The second concludes: “None of these surgical masks exhibited adequate filter performance and facial fit characteristics to be considered respiratory protection devices.” The basis of their 95-99% claim is therefore unclear.
They do not cite the Danmask randomised controlled trial (RCT) into the benefits of wearing surgical masks, which found no significant protection for the wearer from contracting COVID-19.
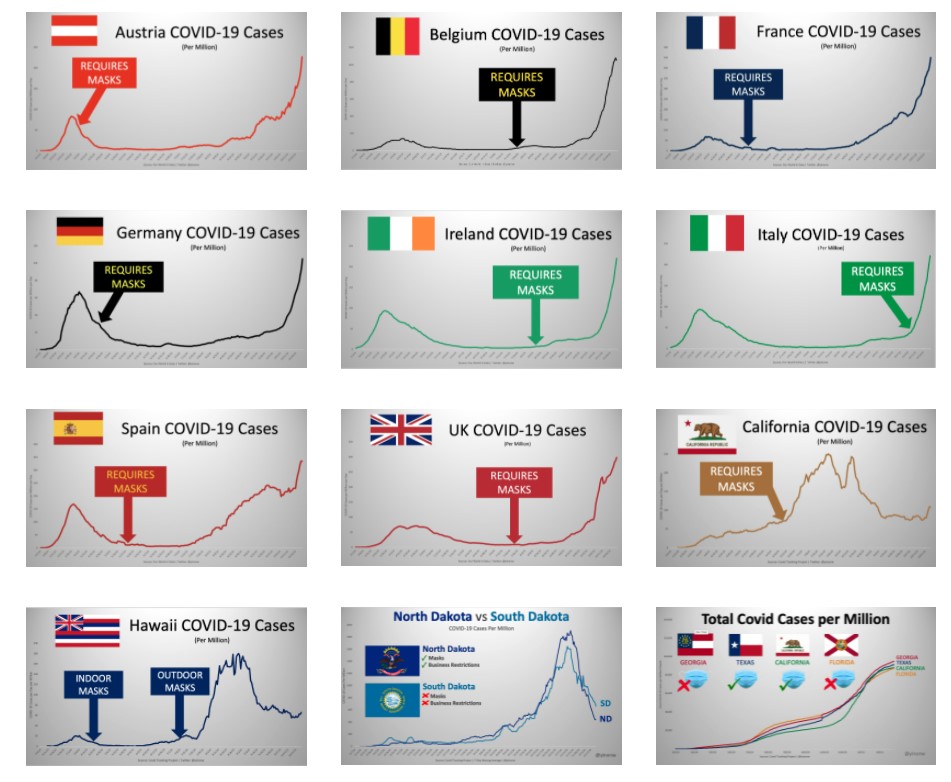
In defence of the massive protective value their model grants to masks they refer to “the fact that face mask directives have been more effective than either lockdowns or social distancing in controlling the spread of COVID-19”. It’s certainly welcome to have some honesty about the ineffectiveness of lockdowns and social distancing, but the claim about the effectiveness of face masks is very questionable.
They cite two modelling studies in support, both published in June 2020. One, by Zhang and colleagues, purported to show that “the difference with and without mandated face covering represents the determinant in shaping the trends of the pandemic. This protective measure significantly reduces the number of infections.” The other reported “the results of two mathematical models” that showed “that facemask use by the public could make a major contribution to reducing the impact of the COVID-19 pandemic”. Yet such studies have clearly been superseded by the events of the autumn (see below) as well as by the Danmask RCT. The decline in infections they attributed to masks, while correctly not attributed to lockdowns and social distancing, should properly have been credited primarily to seasonal factors along with growing population immunity.
![(200312) -- HAWALLI GOVERNORATE, March 12, 2020 (Xinhua) -- People sit with a certain distance away from each other while waiting to receive medical tests at a makeshift medical test center in Hawalli Governorate, Kuwait, March 12, 2020. TO GO WITH "Feature: Arrivals in Kuwait rush for coronavirus tests as gov't tightens precautions" (Photo by Asad/Xinhua) - -//CHINENOUVELLE_1.0902/2003121601/Credit:CHINE NOUVELLE/SIPA/2003121602 (Newscom TagID: sfphotosfour530454.jpg) [Photo via Newscom]](https://dailysceptic.org/wp-content/uploads/2021/04/Coronavirus_social_distancing_1280x720.jpg)











To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.