We’re publishing a new piece today by Dr. Alan Mordue, a retired Consultant in Public Health Medicine, who is alarmed and disappointed that longstanding and important principles of public health have been jettisoned in the pandemic. Alan worked as a Public Health Consultant in England and then in Scotland for 28 years, retiring in 2016. He has extensive experience of teaching and training in public health and was an Honorary Clinical Senior Lecturer at the University of Edinburgh for many years.
Here is the introduction, where Dr. Mordue highlights the difference between what the media often mean by a ‘public health expert’ and an actual trained and accredited Public Health Specialist.
During this Covid pandemic I have heard much in the media from ‘public health experts’ and ‘public health officials’, but rarely from colleagues in my own specialty – Public Health! This is very surprising since the specialty, which I practised for 28 years as a Consultant in England and Scotland before my retirement in 2016, usually leads the management of all outbreaks of infectious diseases in the U.K., and also has had the responsibility for leading the production of pandemic plans in the U.K.
But is there any difference between a Public Health (PH) official, expert and specialist? Certainly you wouldn’t think so listening to most broadcast media. Here are my definitions:
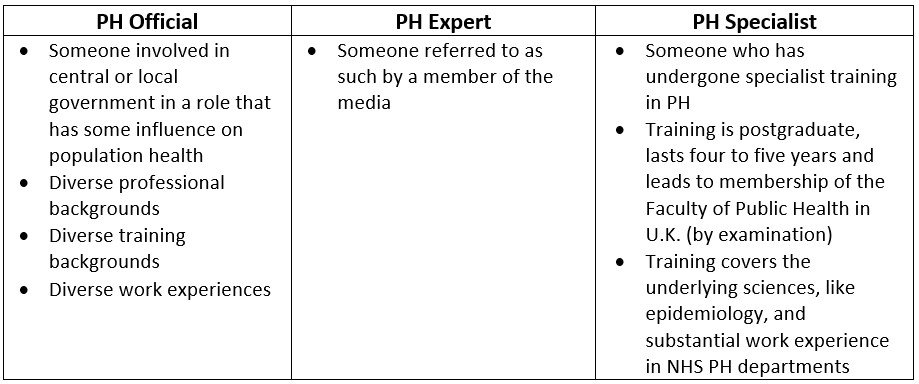
So these three groups are very different. Only one group has undertaken an in-depth specialist training and has theoretical and practical experience in outbreak control and management (as well as other areas of PH specialist practice).
When a PH ‘expert’ expresses views in the media about the management of the Covid pandemic it is therefore essential to know a little about their background training and experience. Even if they have an exalted title like ‘professor’, their chair may be in anthropology or their main experience in nutrition or dentistry. This is not to dismiss the contributions of diverse disciplines – given the inevitable complexity of a national response to a pandemic we certainly need to draw upon a wide range of expertise. However, over the last 18 months I have kept asking myself whether PH Specialist knowledge, skills and experience have had sufficient influence during the Covid pandemic. I will attempt to answer my question by referring to some of the key principles of Public Health and considering whether they have been followed or not during the pandemic response.
Among other things, Dr. Mordue criticises the redefinition of ‘case’ in the pandemic, where for the first time a positive PCR test alone in the absence of clinical symptoms has been counted as a case of the disease, causing big problems with false positives and over-diagnosis.
Either symptoms or a positive test alone is insufficient, both must be present to be counted as a confirmed case. It follows that there is no such thing as an asymptomatic case.
This standard definition was not adopted at the start of the pandemic. Because of this we don’t know how many real cases of COVID-19 we have had or have currently – the numbers recorded include real cases of people with relevant symptoms and a positive PCR test for viral RNA, but also include people with no symptoms of COVID-19 and only a positive PCR test. This has been further complicated by mass population testing in the community and hospitals of those without COVID-19 symptoms, the use of high cycle thresholds in the PCR test, and inevitably large numbers of false positive tests.
The piece is worth reading in full.














To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
Well said Dr. Mordue. Keep it going folks. The truth is coming out now thick and fast. Expect more Van-Tam manoeuvres in the coming hours, days and weeks. The dam has burst.
Van Tam will be off to collect his rewards from pharma.
A knighthood, followed by a golden facemask?
I’ve just been informed that free Vitamin D for the vulnerable groups was withdrawn in February last year. Why would that simple and cheap measure, be stopped before knowing what the effect of the more expensive measure ( vaccines ) would be?
Vit D was introduced as a sop, Matt Hancock having previously denied its efficacy in the House of Commons. Maybe that’s why it was given out in far too low a dose, starting at the height of the flu/COVID season in January. I’m not surprised if it was withdrawn soon afterwards.
The cost to give it to every man, woman, and child in Britain would have been a tiny fraction of the cost of test and trace, let alone the vaccines. \but saving lives was never, apparently, the plan, because the evidence was clear and freely available..
This year I was pleased to be able to roll out free Vit D at proper doses to the vulnerable in my church last autumn, as at least a small counter to the ineffective measures of masks, registers, hand-washes and social distancing that HMG insisted on for such “COVID-safe” venues.
Hancock’s’ charge sheet’ just gets longer by the day! All the mounting evidence is hiding in plain sight!
Tescos, 3 months supply £3.50.
Similar prices elsewhere, e.g. https://groceries.morrisons.com/products/vitabiotics-ultra-vitamin-d-293210011 Take your hat off to the supermarket management, though. They’ve spotted the market.
Yes and they have banned the use of safe and effective Ivermectin, which saves lives for no money ( as being proved right now in India, Bangla Deh and Japan)
It is still banned in the UK by Johnson, Whitty and Javid – why are no MPs interested in stopping early infection with Covid 19 developing and saving lives ?
What is the answer to this constantly posed question? The obvious sone involves a great crime being committed.
A medic friend of mine recently told a Consultant Cardiologist about Ivermectin use i the treatment of Covid …the Cardiologist asked: ” What’s Ivermectin?”
I understand that Ivermectin works by preventing the spike protein from being able to access the cells, there is also research I’ve read that shows ivermectin has the same effect on the spike protein in the ‘vaccine’…….
I believe this to be true which is why they have suppressed its use – nothing could be clearer.
I do hope the Police in Hammersmith are informing themselves of the implications of a “duty of care” which applies to all in Government in relation to the people they serve.
Existing effective measures had to be suppressed because there is a legally mandated hierarchy of drug use.
i) Medicine approved to treat the disease
ii) Approved medicine that can be used ‘off label’ to treat the disease
iii) Unapproved or untested experimental drugs
Ivermectin and the like got in the way of the massive windfall profits for Big Pharma with their level iii) drugs.
And to make it clear, the so-called ‘vaccine’ products are iii), and in effect, the Emergency Use Authorisation (EUA) would not be valid – not that one can sue the pharma trade yet.
Much, much more than that. There are multiple effects on disabling the virus: stopping bonding to the ACE2 receptor, inhibiting access through the cell membrane, and disrupting viral replication within the cell as a last defence.
Add to that its anti-inflammatory properties and slight anticoagulant properties and one has a very useful medicine for all stages: prophylaxis, early treatment, treatment if the virus it gets to the lungs, and then if it gets into the bloodstream.
Another important feature about ivermectin is that it is one of the few medicines with anti-viral properties against RNA viruses (such as coronaviruses) that can get into the ‘air side’ of the lungs from the bloodstream. It can thus stop the viral replication before the lungs are damaged and the virus invades the body through the lungs.
A paper in the Journal of Antibiotics listed out the multiple mechanisms of action thus:
The targets of activity of Ivermectin can be divided into the following four groups:
And if there’s any left over you can worm your horse with it. Try that with the quacksines!
Deworm please. It’s an antiparasitic drug and not a parasitic one. If it was, one should rather use it to worm the likes of Devi Sridhar than poor horses!
As described in summary by Drs Ryan Cole, Peter McCullough, Richard Fleming and many others and they were all trashed by the “Full Fact” stormtroopers including the health quangos, CMO and CSO types – I read some summaries and if I did so did SAGE/NERVTAG Fauci’s emailed brigade including Drosten, Farrar, Vallance to fire up the attack dogs.
I predict a torrent of weasel word excuses throughout 2022 from those on the increasingly longer charge sheet.
JAG_Docs_pt1_Og_WATERMARK_OVER_Redacted.pdf
They knew and covered up that Ivermectin worked against COVID.
Not only that: they also denied the efficacy that was demonstrated in Uttar Pradesh.
‘It must have been a coincidence…’
The problem with Invermectin is nothing to do with medicine. It is to do with bureaucratic rules.
Vaccines need to pass full safety tests before being approved
Vaccines MAY be given ’emergency approval’, if, and only if:
No. 3 above is the sticker. Because Invermectine and Hydroxychloroquine are ALREADY APPROVED medicines. They are just not accepted as alternative treatments.. If they were, you COULD NOT approve emergency vaccines.
So they have to be found to be ineffective against Covid….
“There is no magic money tree”, as someone once said.
Bought? Threatened? If so by whom?
https://youtu.be/XataZMWV2rM?t=105
This press conference was 30 mins before Boris had a party!
https://www.fightaging.org/archives/2022/01/senescent-cells-negatively-affect-t-helper-cell-differentiation/
Aging and senescence impact CD4 T helper cell (Th) subset differentiation during influenza infection. In the lungs of infected aged mice, there were significantly greater percentages of Th cells expressing the transcription factor FoxP3, indicative of regulatory CD4 T cells (Treg), when compared to young. TGF-beta levels, which drive FoxP3 expression, were also higher in the bronchoalveolar lavage of aged mice and blocking TGF-beta reduced the percentage of FoxP3+ Th in aged lungs during influenza infection.
Since TGF-beta can be the product of senescent cells, these were targeted by treatment with senolytic drugs. Treatment of aged mice with senolytics prior to influenza infection restored the differentiation of Th cells in those aged mice to a more youthful phenotype with fewer Th cells expressing FoxP3. In addition, treatment with senolytic drugs induced differentiation of aged Th toward a healing Type 2 phenotype, which promotes a return to homeostasis. These results suggest that senescent cells, via production of cytokines such as TGF-beta, have a significant impact on Th differentiation.
i.e. this might be why old people suffer from COVID more and it can be reversed quite cheaply.
So cheaply Pharma make no money and Gates doesn’t’ get his “vaccines” into the arms of the whole planet – there is your problem!
Why on earth would we listen to somebody like Mordue when we can parachute somebody like Devi Sridhar into our “expert groups” and let them make it up as they go along?
Is Mordue “diverse”? Is he even female? I think not.Does nothing for our affirmative action credentials. Is he perhaps at least a sexual pervert of some kind?
Is he young and photogenic, uncorrupted by prejudicial issues such as wisdom accrued through living life, and long years of actual experience in the field of his expertise? I see no evidence of such.
Does he have the imprimatur of approval by the global elites? Some fellowships or scholarship awarded by worthy elite-funded bodies, decorative involvement in virtuous globalist “charity”, at the least some kind of informal associations with celebrities, billionaires and political high flyers?
Away with your nonsense about “expertise” and “experience” and “competence”. That’s not what technocracy is all about!
The diverse the author used in the graphic is nothing to do with diversity in a gender or race sense; rather, diverse work experiences simply means different jobs… imho….
R = 0.88 and still falling
That exlains why the statistic is no longer pimped in the fear-mongering media. It is totally off-message.
Excellent piece.
“in my view what has happened amounts to a betrayal of the Specialty of Public Health and all the principles and values it used to stand for; and a betrayal of the Public’s Health, in other words the health of the population. The excess non-Covid deaths we have seen so far, I fear, is just the beginning. What mystifies me is why my former colleagues and the U.K. professional body charged with developing and maintaining standards in the PH Specialty, namely the Faculty of Public Health, have been so quiet thorough the whole of this pandemic.”
Let’s hope there’s a proper reckoning.
He needs to understand that our government has been hijacked by a bunch of traitors who are deliberately subverting and destroying the UK and other parts of the western world. It is deliberate and co-ordinated, with stooges in place throughout the governments of the western world to make this nightmare a reality. Some of these are graduates of the World Economic Forum for example. These are easy to identify traitors who are put in place to do the dirty work of the criminal WEF. They are committing treason in doing so. Treason is illegal.
Here is a recent broadcast from Brendon O Connell where he lays out a lot of what he has uncovered and condenses it down. His work is key to understanding a lot of the geopolitics of what is happening in the world. This has the Henry Kissinger banking conference clip where he says that the “world centre of gravity” will shift from the west (America) to the east (China) and that the US needs to decide what it is going to do about that ie become subservient to China. Thats my interpretation of it anyway.
91. Jan 6, Proud Boys Kissinger Shadowgate
https://www.youtube.com/watch?v=-Q–v67NgxE
Kissinger apparently coined the phrase “power is the greatest aphrodisiac ” and enjoyed talk to fellow ‘researcher’ Mao about the thousands (?) of women involved in testing out the theory.
He appears to have no particular loyalty to the West – it is all just a Great Game to him.
Looking like Kissinger did, you’d need something as an aphrodisiac for your intended partners.
Here is a must watch clip – check Bourla talking at the WEF saying they (presumably Pfizer – the company with the dubious honour of the maybe the worlds worst criminal records under their belt – good decision by HMG to get them to jab everyone – I assure you the decision making traitors in HMG always get criminals in to do their home maintenance of course) are making a chip to insert in to tablets to ensure you have taken the tablet – for “compliance” he says. This is the mindset of these antihuman despicable people laid bare.
People need to be fully aware. There is a group of people – the likes of which infest and control groups like the WEF – who believe they are put on this Earth to rule over you and your family. They believe that you are there for their benefit only – to be their slave. These people believe that. Complying with this tyranny is akin to signing up to be their slave.
Evidence of Self Assembling Nano Circuitry in the Pfizer Vaccine
https://www.bitchute.com/video/XYbGmfr6EWWv/
Klaus Schwab and his great fascist reset
https://winteroak.org.uk/2020/10/05/klaus-schwab-and-his-great-fascist-reset/
Was the 7 year old Schwab a member of the Hitler Youth I wonder?
Ten year olds defended Berlin with Panzerfaust grenades. Where was he when the Reich collapsed ?
National Socialism was just Fascism ( Corporates, the Banks plus the State) plus Technocracy and Nationalism – exploited as a tool of conquest. Schwab has added digital technology and instant global reach – Tweats move faster than Tanks! He has replaced marching manipulated nationalist fanatics with his dreams of Transhumanism and Robots. He has replaced indoctrination and the Gestapo with medical tyranny and the syringe to enforce ‘self compliance’
But in the end Fascism is Fascism whether in business suits or SS Uniforms.
Those who have abused the term “Fascist” for so long for their own narrow adolescent Leftist ends finally have something to shout about …oh but wait …they are now all themselves just subverted into being part of the Great Reset Army!
What is very clear is that the British Labour Party, which ought to be defending our freedoms and the right of workers not to be forcibly jabbed , is morally bankrupt, and now just a confused, rotting Wokist Corpse.
The trilateral commission only has two wings David, Far Right and even Farther Right. If Starmer ever gets into power we just might find out which of those wings he belongs to.
Having his byob party is one of the only sane things Piffle has done in the last two years, there are a thousand reasons he should be ousted, even imprisoned, but if it brings Starmer into power it will not be worth it, he is about as socialist as Margaret Thatcher’s ghost and far more frightening.
Know lets see, what did he support by way of ineffective, unworkable, society destroying, mental health crisis causing, SAGE devised policies…basically they propped Johnson up on more than one occasion and offered precisely nil in the way of informed counter measures except to call for more lockdowns, earlier….worthless.
National Socialism was just Fascism ( Corporates, the Banks plus the State) plus Technocracy and Nationalism
Every bit of this statement is at odds with both actual history and its theoretical underpinnings. It’s nothing but Whomever I disagree with for whatever reason, I want to call them fascists or nazis! If you’re serious in your opposition to what you claim to be opposing, you’re terminally weakening your own position by this entirely inappropriate use of terms as the people on the other side will just claim that this proves you must be an antisemite, that is, a not-so-covert nazi, yourself, as is happening in the real world all the time, especially in Germany.
We really have to keep sane, sober, serious, qualified and experienced people like Dr Mordue out of the picture as his
misinformation could do incalculable harm topublic healththe digital ID rollout.It is an excellent piece. But like others now popping their heads above the parapet, its 18 months too late. Heneghan on the contrary has been preaching this throughout and putting his name out there behind the GBD no doubt at some considerable personal cost.
However better late than never.
The more heads pop up up the more will follow!
The invisible clothes are falling from the Emperor!
And the bastard’s being forced to don a clownsuit.
Early last year I think he made a point on Talk Radio that he had not signed the GBD. Whether he has done so since then, i know not. Nevertheless, he has unquestionably attempted to push back where most others in his postion have not.
He is named as a signatory.
“No such thing as an asymptomatic case”
So “Sir” Whitty lied.
He clearly doesn’t understand that determining if symptoms are present takes more effort than putting a spreadsheet up on a website. From what I understand there are well over 150 symptoms that are associated with the disease, only a handful of which come close to being unique and they require e.g. x-ray or mri technology to get a diagnosis.
Peyrole excellent comment. . Just beat me to it
The author is trying to be charitable. But it’s not just the faux experts. Not only epidemiologists and viruses, but doctors and nurses have been a part of the great betrayal.
The ignorance of so many Doctors and Nurses about the nature, contents, safety ,and function of the “vaccines” they are pushing is simply staggering!
“Informed consent” was just a fantasy for 90% of the trusting recipients !
When ignorance is keeping your job and pocketing £££££, ’tis folly to be wise.
TOH confirms many what used to be called Obs&Gobs consultants and Midwives as well have blindly followed the diktat and continually supported the jabs to pregnant women….very very scary that these “clinicians” suspend their faculty to think and just go with the flow; whilst they do that two NZ Doctors put their careers on the line to expose the cover up of Pfizer trial data , admitted by the CDC in the US, that shows how bad their jab was on the cohort in that trial ( see The Expose).
Public health is fully politicised.
Nothing more to be said.
Superb article, thank you.
When the fine-tooth review comb is applied in the years ahead we’re going to see how the government/media complex got the root cause wrong, the test criteria wrong, and the solution horrendously wrong.
And what cost! Lives lost. Education destroyed. Mental illness multiplied. Businesses destroyed (mine included). Billions of £££ squandered. Police powers multiplied.
And all for no signicant increase in the annual death toll.
Preserve those documents. Heads must roll.
Isn’t it the case that SAGE had not a single Public Health trained and qualified expert on its panel. Explains why the response was so disastrous.
Hopefully the author when he says “Bizarrely, early treatment approaches were not encouraged to prevent the development of more serious disease and the need for hospital admission” is having a laugh as there is incontestable evidence that from day one there was continuing suppression of the use of known successful treatments for those sick from the virus. It may be bizarre to a dispassionate observer, but from those dealing with sick patients it was a deliberate exercise in mass killing.
Oh but did they not have world class modellers to take shit advice from, and people like Farrar – until his resignation – whose dirty email fingerprints are all over this SARS COV2 scam.
Very well-reasoned analysis.
We do have to wonder why pretty much every previous tenet of Public Health doctrine was abandoned for covid-19. You can certainly make the case that in very early 2020, when we knew relatively little about the effects on the wider population, that some sort of non-pharmaceutical intervention was at least plausible. But by May or June of that year it was abundantly clear that covid posed no meaningful risk to the vast majority of the population. And that millions of people’s lives, occupations, and health were being sacrificed in pursuit of a goal (“zero-covid”) that was impossible to obtain. Why the British people (as well as the people of most every other industrialised country) were subjected to this outrage is a question for the ages.
The utter lack of interest among the “public health officials” and “public health experts” in subjecting their diktats to any form of cost-benefit analysis represents a level criminal negligence and incompetence unprecedented in modern European history.
I think the answer to that is twofold:
Let’s face it: an ‘expert’ nowadays is someone who purports to know something that the lazy journo interviewing him/her doesn’t.
This piece is sheer gold.
We have got used to the use of the term ‘Sceptic’ – but an antagonism to the current Covid narrative doesn’t essentially rest on ‘scepticism’, but on a long-standing, rational body of knowledge about Public Health.
It is the Narrative that is aberrant – based on false ‘expertise’ – and this is really well summarised here from a knowledgeable perspective.
Excellent!
This is the age of the expert.
I am a real, genuine and accepted expert.
Give me the money, and I will pronounce on anything.
Many thanks for all your interesting and often amusing comments – we do need to keep smiling even though what has happened over the last 2 years is so awful. However, I wanted to specifically respond to peyrole’s comment about heads popping up late in the day, unlike Carl Henneghan. Unfortunately we all don’t have the profile or credentials of Carl and many other stalwarts like him to get on JHB’s breakfast show or GBN, but I can assure peyrole that I have been speaking out since summer 2020 in numerous letters to the MHRA and JCVI with likeminded colleagues, letters to the Planet Normal podcast, my MP and MSP, and via membership of HART to mention a few.
Thanks for your work on this.
“I have been speaking out since summer 2020 in numerous letters to the MHRA and JCVI with likeminded colleagues“
The reality is that we will likely never know how much practical influence this kind of effort has had on those advising those making the decisions, but it’s quite possible things would have been significantly worse at crucial moments without such activity.
Bravo Sir
And yes I did sign the GBD very soon after it was developed.
Me too
As Mark says below with piercing irony, why should we listen to people like then author when it’s not about knowledge and professionalism but spin. Jason Leitch, the low wattage, garrulous gob technician who poses as Scotland’s National Clinical Director is like Van Tam good at spinning irrational directives into homespun wisdom for the innumerate and incurious journalist tribe. He is on STV tonight flanelling away the bad decisions he made on the basis of being a statistical dullard, and propping up Sturgeon’s control freakery. Devi Shridhar and Linda Bauld seem vacuous but “engaging” good for sound bites. Neither is a public health specialist. As an academic it’s very easy to be vacuous as long as you genuflect before commonplace verities like diversity and the precautionary principle. Then we have the screaming skull of behavioural panic nudging Stephen Reicher. Sadly I have met public health graduates and many of them are a combination of all of this. I was in a stats class with some as a masters student and I was appalled at how awful they were at stats, but they all got a free pass. Their real passion was banning alcohol, policing health behaviour and eradicating smoking. They really are a long term threat to freedom and democracy.
Reuters reporting Japan is at 1% of its COVID peak cases and falling. India is at 3% of its peak and falling. What did these countries do? Ditch vaccine mandates for ivermectin. Since April 28, India medical officials started providing hydroxychloroquine and Ivermectin to its massive population. As India is the major pharmaceutical manufacturer in the world, they were ready for this massive drug distribution. MIRACULOUSLY!, COVID cases have plummeted quickly since then. Meanwhile, all “first world” countries in Europe are reporting a rise in cases. Get your ivermectin before it is too late! https://ivmpharmacy.com
My sister is an A&E consultant. She said the Covid beds were almost entirely filled by obese patients in their 50s. Perhaps she was identifying some risk factor.
I like the thoughts in the article and it’s good that Dr Mordue has taken into account actual evidence. I would like to think I wouldn’t have been out of work for 10 months had evidence ever been considered at any point during this thing.
I think fewer people would have died and suffering would have been very much reduced if government had done nothing at all. I don’t understand why the government needed to get so involved in the first place.
Wasn’t the system just punt it of to the pre-2020 public health PHDs who have spent their lives thinking about this sort of thing? They would have probably have been able to communicate some useful info. A bit like what what the Swedish did.
I reject the idea that government was pressurised by press etc. Government has been the biggest funder of the press with all the double page covid ads which I suspect would have been withdrawn should the press have printed the wrong thing elsewhere.
I’m fully with the ‘conspiracy theorists’ now. I’m going to be very careful about anything I am coerced to do. Coercion is powerful. I’m not old and the last 2 years have helped me develop my own eating disorder so I’m not fat but 2 jabs were necessary to keep my job. Not doing 3. Not wearing pointless masks. Not doing stupid just because stupid mandates.
I seem to recall that someone in a hosp that had a well known individual in, allegedly with C-19, ‘accidentally’ published his Body Mass Index (BMI); not a nice number. The best you could say is that he must have used a good tailor to disguise it!
Dr Mordue confirms what I have been writing for many months, along with others. The experts have been the wrong experts; positive tests are not cases; tests have been misused. And it’s not just public health clinicians, it’s acute medicine clinicians whose expertise has been ignored. The proper treatment of severe COVID-19 was delayed by months because those in charge refused to listen to those who understood what caused it. They got there in the end, but wasted 6 months doing so.
The evidence points to transition to an endemic phase and downgrading of the coronavirus threat to that of a cold or flu, so maybe we can begin to relax, and prepare for the enquiry.
I suggest deleting a few characters from the last word in the headline. How about “dem”; that’s more like it!
I believe there was a study done years ago that when doctors in the USA went out on strike, the death rate plunged.
In the UK the death rate dropped a bit when there was a junior doctors strike. This was anticipated by Raspe, who wrote the adventures of Baron Munchhausen in the 18th century, in which the Baron hoists the College of Physicians into the air with a giant balloon; the fellows did not notice, continued feasting and the death rate dropped.
This is merely a reflection that disease can be iatrogenic on the one hand, and that people can to some extent think themselves well on the other..
It could also be as simple as there not being enough doctors around to officially reord cause of death. Reported fatalities always drop over the weekend, followed by a spike on Monday or Tuesday. That effect could also be caused by an abscence of bureaucrats that do the actual data entry/info dissemination.
Many thanks for the job role definitions. The Public Health Director in Devon has a BSc in Sports Science and another qualification (??!!) in Hypnotherapy. Says it all really.