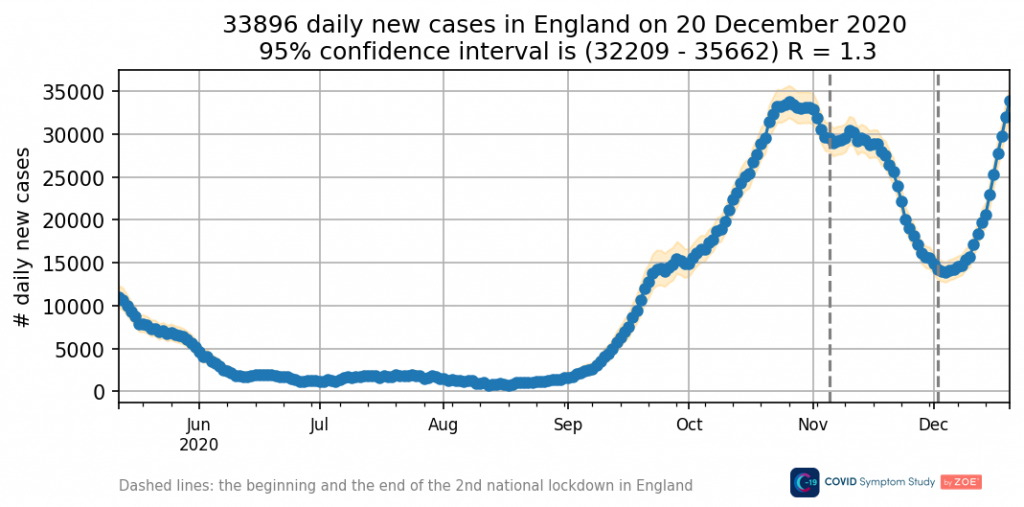
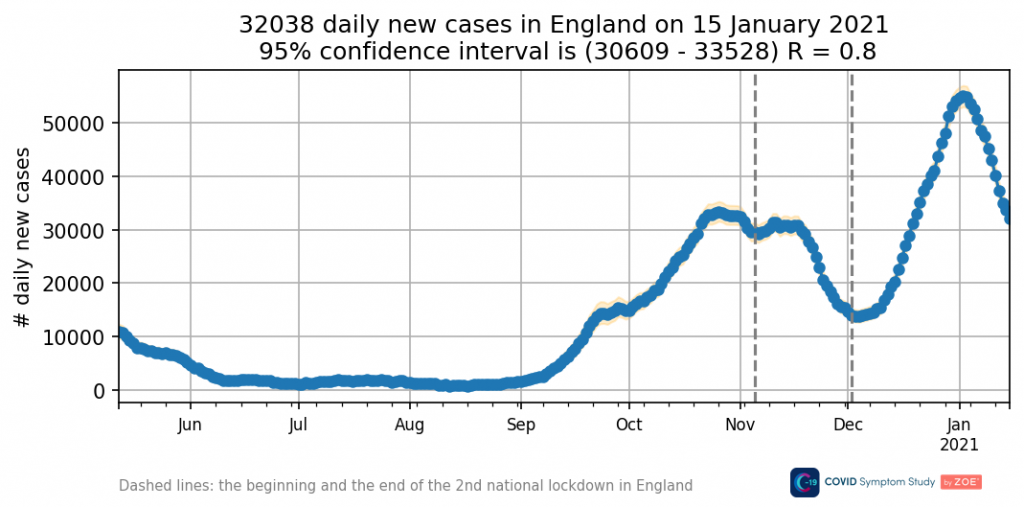
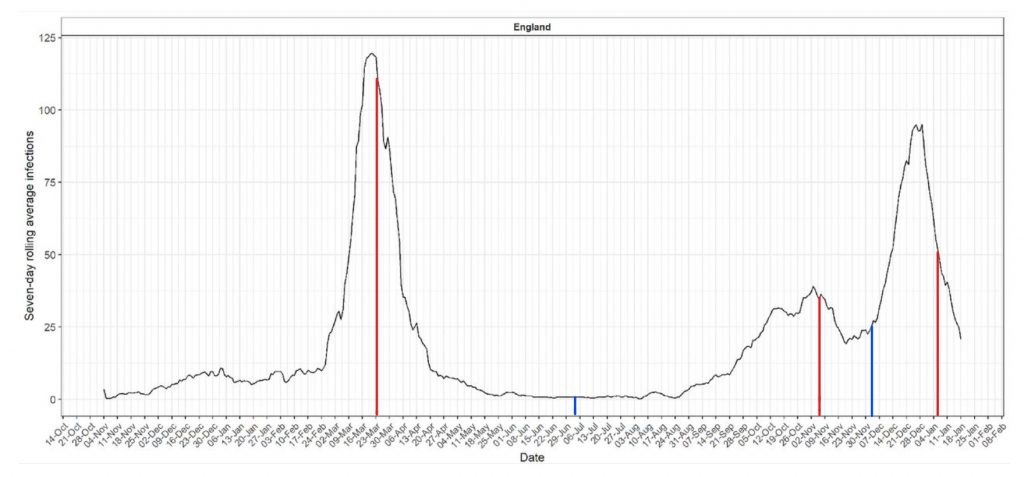
I wanted to come back to the question of what causes COVID-19 occasionally to have explosive outbreaks. We’ve had two in England so far. Using the graph below (produced by Imperial’s REACT study using symptom-onset reports from their antibody survey, so no PCR tests involved) we can see when they occurred. The first occurred from around February 25th to March 19th 2020, ending after about three and a half weeks, as abruptly as it began. The second got going around December 2nd, and ended – once again abruptly after three and a half weeks – on December 25th. As the lines below indicate, these starts and stops bear no relation to when lockdowns were imposed or lifted (the red and blue lines respectively).
Given that (as we can see) Covid was around in England throughout the winter of 2019-20 (arriving in November according to this graph) and was also simmering away in the autumn of 2020 without taking off, a key question is what triggers the beginning and end of the more explosive outbreaks?
Another way of putting the same question is: why does COVID-19 occasionally, Jekyll and Hyde-like, transform from a relatively gentle, not very infectious disease into a super-infectious disease for a few weeks, before suddenly returning once more to its largely benign form?
Perhaps surprisingly, Covid in England has only been in ‘Hyde’ form for about seven weeks in total so far, with the R rate (the speed at which the epidemic is growing) only going significantly above one (indicating an exponentially growing epidemic) for around three and a half weeks in February/March 2020 and three and a half weeks in December 2020. The rest of the time it’s been up and down in different regions, particularly in the autumn, but there’s been no nationwide surge. What, then, on those two occasions triggered the disease to become briefly so much more infectious across the country?
It’s tempting just to say it’s seasonal, and indeed it does appear to be. But not predictably so, given the virus has been around now for two winters and two springs, yet broke out in its first spring but not its second, and in its second winter but not its first. Besides, calling it seasonal only begs the question as to what triggers seasonal outbreaks of infectious diseases, a question which is widely debated.
We would expect the difference in infectiousness during surges and outside them to show up in the secondary attack rate (SAR – the proportion of contacts an infected person infects), and sure enough it does. Public Health England (PHE) estimated the SAR of the Alpha (British) variant at around 15% between November 30th and December 20th during the winter surge, going a bit higher in some regions. Afterwards, in the period January 5th to March 7th, it went down to 11%. (More recently it went down to 8%.)
This may not seem like a big difference in absolute terms, but in relative terms it’s a considerable drop to around two thirds of the value between December and January. This is, not coincidentally, the same kind of change that we see in R over the same period. According to the ZOE Covid symptom study, R was about 1.3 during the December surge and around 0.8 during the January decline (see charts below) – again, around two thirds of the value. (Note that R will also include people infected with no known contacts, say via aerosols in a supermarket or in a restaurant from an infected person at a different table. Since such anonymous transmission likely increases during a surge as there is more virus around, this may explain why R changes a bit more than the SAR.)
This suggests that the difference between Covid surging or not comes down to whether each infected person passes it on to closer to 10% of their contacts or 15%. Or in other words, depends on only around 5% of a person’s exposed contacts being more susceptible to infection. Since we can assume about 90% of a person’s contacts are usually protected by their immune system in some way (not just antibodies but innate immunity and T cells as well), this means just one in 18 of a person’s contacts needs to succumb to infection who wouldn’t normally to result in an outbreak.
What could produce this effect in a population? Two possibilities present themselves: a seasonal weakening of the immune system that would result in around one in 18 more people succumbing to infection on exposure; or a change in the virus that makes it more able to evade the initial defences of around one in 18 people and develop into infectious, symptomatic disease.
With regard to the first possibility, it is now well-established that the human immune system involves numerous seasonal cycles (with “more than 4,000 protein-coding mRNAs in white blood cells and adipose tissue” having “seasonal expression profiles”) that go a long way to explaining why people are more susceptible to contagious diseases like flu and Covid during the winter months. However, by itself that wouldn’t account for why outbreaks are suddenly and irregularly triggered, rather than occurring in, say, regular fashion during the winter according to the stages of the cycle.
Perhaps then the second possibility, a change in the virus, plays a part. This would come in the form of new variants that can evade the initial defences of around one in 18 additional people. Thus, on this theory, it was the arrival of the Alpha variant in winter that pushed enough people over the threshold to trigger an outbreak.
If this is right, then what ends the outbreak a few weeks later is when enough people become immune through infection to restore the temporarily disturbed herd immunity and push the SAR back down close to 10% and the R below one. (Another factor that could play a role in increasing the SAR temporarily is vaccination, perhaps by suppressing the immune system briefly, or by increasing exposure through the vaccination programme, or in some other way.) We can reasonably expect that this iterative process will not go on forever, and SARS-CoV-2, like other seasonal viruses, will before long be supplanted by a new dominant virus.
The lack of outbreak in winter 2019-20 might be due to competition with flu, which was subsequently out-competed as it faded in spring. Or maybe it was new variants arriving in February and March 2020 which triggered the spring surge – the genomic data is a little hazy.
The upshot? Primarily, further confirmation that COVID-19 is a seasonal disease to which most people have some immunity and which relies on new variants to produce enough disruption to population immunity to produce short but sharp outbreaks. Further confirmation, too, that models that predict mass infection of a highly susceptible population whenever restrictions are lifted are fundamentally misconceived, hence why they have been invalidated time and again. (Texas has now gone almost four months since reopening without a surge, and likewise Florida and other open states.)
Confirmation, in other words, that Covid is not, and never has been, a reason to impose harmful restrictions on society.













To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
If the Zoe data is to be believed, there is a third surge which started at the end of May. Not quite as steep as the December one, but close, and still going. Perhaps another variant? It has lasted slightly longer than the December one. Given that a lot of people had been vaccinated by June, you’d expect it to have had more impact.
So what’s the policy now?
I’ve lost track of things. What are we meant to be doing now? vaccinating everybody to kill off this virus, or locking everybody in their own homes to kill the virus, or something else? And how come the plots of cases is still shooting up? What’s the current big idea?
I’m not sure thinking about “policies” is going to get you very far, if what you mean is thought-through actions, backed by logic and evidence, designed to achieve a specific, measurable and meaningful result, monitored and modified as necessary, and related to actual public health goals. What we get is just stuff that is thrown together to sound good, tweaked according to what they think the public will put up with, and justified by whatever measures suit them at the time, preferably ones that are easily manipulated, and when none of the measures suit them they produce ridiculous models, all of which have utterly failed to come true.
The Big Idea is to stay in power and keep the Big Lie going, by any means necessary.
The ZOE website also says that the common symptoms of this latest ‘variant’ are runny noses and sneezes. Sounds remarkably like hay fever to me which i am told by friends who suffer from it is very bad this year. A useful way to prolong ‘cases’?
Like hay fever or the common cold, yes. It’s very odd – could be misreporting or that the virus has changed a lot in the way that it affects people. Shame there appears to be no real desire from the govt to learn much. I think they realise the less they know the easier it is to pretend what they are doing is for the best.
“Shame there appears to be no real desire from the govt to learn much. ”
Re that last point, consider the observations at the end of this piece:
PCR test cycles are different depending on vaccination status (from Livestream #85)
DarkHorse Podcast
Yes, I had read about that. A desire to obscure rather than reveal the truth.
Yes, I think Clare Craig suggested Covid was perhaps mutating towards being a cold. As had been predicted.
The grass is infected!!! The virus lives on the pollen. We must cut it all down immediately.
The sensible policy would be and would have been to treat people who became ill with effective and available treatments and leave everyone else alone. It’s perfectly clear that lockdowns and masks etc make no difference and a vaccine was never needed, except of course, to make a great deal of money.
Indian variant and asymptomatic or overwhelmingly mild, amongst the young? spreading natural immunity, so to be welcolmed.
CNN Celebrates 100th Anniversary Of Chinese Communist Party, Claims Xi Is ‘The Real Star’.
https://thenationalpulse.com/breaking/cnn-celebrates-100th-anniversary-of-chinese-communist-party-claims-xi-is-the-real-star/
Stand in South Hill Park Bracknell every Sunday 10am meet fellow lockdown sceptics, keep yourself sane, make new friends and have a laugh.
Join our Stand in the Park – Bracknell – Telegram Group
http://t.me/astandintheparkbracknell
‘What, then, on those two occasions triggered the disease to become briefly so much more infectious across the country?’
‘The lack of outbreak in winter 2019-20 might be due to competition with flu, which was subsequently out-competed as it faded in spring.’
‘….the genomic data is a little hazy.’
Until the PCR test is completely discredited, any analysis of the data is fraught with difficulty, uncertainty as to the reliability of that data.
‘The MVZ Laboratory in Augsburg made wrong diagnoses in 58 of 60 tests it identified as positives over a one-week period….’ and so on and so forth…….
https://www.reuters.com/article/uk-health-coronavirus-germany-tests-idUKKBN27D1FD
How much, for example, of the covid 19 ‘outcompeting’ of flu in spring 2020 was due to the hospital clearances? How many, who died, died of complications caused by influenza but were incorrectly diagnosed with covid 19 through flawed testing?
It seems unlikely, now, that we will ever get the answers to these kind of questions in this democratic socialist and now profoundly illiberal country.
Apparently some very wealthy individuals have already fled to their idea of ‘Galt’s Gulch’
And what was the location they selected……..?
……….New Zealand……..(……..the ribs….I have to stop now…..)
https://moneyweek.com/economy/people/601023/peter-thiel-utopian-elite-flee-for-galts-gulch
Will pointed out that the data didn’t rely on the PCR test.
The data on covid ‘outcompeting’ flu is, of course, based on PCR test results
More fascinating stuff from Will, which I only have time to read very quickly and respond to right now.
I like the idea of ‘temporarily disturbed herd immunity’, whatever the mechanisms might be – seems like a goer to me.
This suggests that the difference between Covid surging or not comes down to whether each infected person passes it on to closer to 10% of their contacts or 15%.
I’m not so keen on this – if this were true, wouldn’t lockdowns and other non-pharmaceutical interventions be likely to have a significant effect? NPIs probably do reduce the number of contacts, and by this hypothesis they wouldn’t have to reduce them that much to have a dramatic effect. But the empirical evidence says they have almost no effect whatsoever, and what net effect they do have in fact makes things worse.
… the difference between Covid surging or not comes down to whether each infected person passes it on to closer to 10% of their contacts or 15%.
I suspect this is the mathematical description of an observed phenomenon, rather than something that gets to the heart of what is going on.
Perhaps then the second possibility, a change in the virus, plays a part.
‘A change in the virus’? This seems highly plausible to me, and something that hasn’t received nearly enough attention. Although what that change is anyone’s guess right now. We tend to think of the virus as this dumb, reactive organism (after all, ‘it’s just a virus’, and we like to think we are able to predict what such simple organisms will do, clever beings that we are …). But is this correct? I suspect not. I suspect that all so called ‘simple’ life forms are innately a lot smarter than we like to think.
I may have this wrong, but I recall ages ago hearing on the radio that in experiments tree roots have been shown to grow towards water sources which they have no way of knowing are there. How do they know do this? I also recall a programme of ages ago which depicted just how astonishingly clever an oak tree is over its seasonal and multi-seasonal life cycles.
So why not a virus? One over-riding theme runs through all life forms: the goal of replicating itself, improving itself as it does so, and thus ensuring the species life span. Perhaps the virus somehow ‘knows’ when to let a surge die down and let itself go endemic, such that it can return later, perhaps in other mutations giving it new opportunities, and thus prolong its life cycle.
But I’m getting so far into the realms of speculation here I’m almost into theology, which probably isn’t a good idea.
Time to make another cup of tea and deal with the children …
Ecellent thoughts. Will’s piece too. Food for thought outside of the box presented by The Science.
When making graphs, I think that we should be very careful about when to say that the lockdown started. For us, the November lockdown ended in tiers which were almost as bad as the lockdown itself for many people. My family was put into Tier 4 over Christmas and the difference between Tier 4 and the lockdown that was announced on 6 Jan was only that Tier 4 didn’t cancel school. But, it was a school holiday…
Also, when I look at the graphs on worldometers.info for the United States, it looks like they had two waves. If you drill into New York, however, you note that New York didn’t have much of a second wave to speak of. And, if you look at California, you don’t see much of a first wave. Is it possible, using regional data, that we are just seeing the disease hit different cities or regions at different times?
Sorry to reply to myself, but we’ve also been under various lockdown provisions since 23 Mar 2020. Even over the summer, we had rules of six, limited indoor gatherings, etc. And last Christmas was cancelled for most of the country. There’s a lot more nuance to it than a simple line can provide. Another thing to note is that the second national lockdown didn’t include the schools. And, so, as far as my family was concerned November was less locked down in than late December which had Tiers, but school holidays.
At the end of the day, many of those who come up with graphical expressions like that are pretending to be so-called ‘experts’. The wrong people for the job, in effect, with a gross negative effect on the society they are supposed to serve (in theory).
So the question is, why are there small, but widespread, increases in secondary infections? Like you say, amongst all the noise, this suggests a fundamental causal factor. As with many viruses driven by aerosol spread, as we now know is the case with SARS-COV-2, this is human behaviour itself. In Winter, in colder climates, people congregate together into smaller, heated spaces: a mass change of behaviour. Viral aerosol concentrations rise and, as a result, so do infections. The number and variety of contacts in this setting doesn’t change however, and so the virus rapidly runs out of new contacts to infect. The virus then retreats until there is another mass change of behaviour, with the same fundamental factors in play, and new targets for the virus, and so another surge in secondary infection rates. The first wave was a result of a novel virus, low levels of immunity, with a target population already indoors in Winter, and as they became more fearful of the virus. The lockdown didn’t have much effect as the change in behaviour had long since occurred, and personal contacts established and stable. A mass change in behaviour over the Summer caused infections to gather pace and surge again over Winter, finding previously uninfected households, with lockdown affecting the timing and pace of the surge. The rapid decline again caused by settled behaviour as the number of personal contacts are stable and established and the virus runs out of targets.
And it’s probably also true in farming, if you ask a vet (if any of them are prepared to speak, that is).
How do we know how many cases there were in the winter of 2019/20 – there was no testing? I know lots of people who think they had it then.
Just going to say the same thing! I’m pretty damn sure it was circulating in the community in December 2019 as I knew so many that were ill at that time, myself included. I’ve also heard since that it is strongly believed by certain sources that this was actually the case. My symptoms were exactly as described as the main ones: very bad cough felt deep in lungs, fever, and loss of taste and smell for a much longer period than what is usual for a virus. I was ill for a week and it took a couple of weeks to fully get back to normal. I was over the initial symptoms fairly quickly though. This could have due to the fact I have to take hydroxychloroquine and VitD everyday for an autoimmune condition. I didn’t connect this until much latter, though!
Yes I know far more people here in Suffolk who had “it” between october 2019 and february 2020 than had “official covid” later. Same for parts of the west country and elsewhere.
This strongly suggests the previous infection caused immunity.
And another one. I was a bit like that in late Dec 19, most likely acquired in the run up to Christmas. I did offer a blood sample to the usual place later on when offered the jab. No reply to that, though; they’re not interested.
I have data, albeit from a single hospital trust, that shows the number of influenza admissions in the autumn of 2019 as being all but non existent, but the admissions for pneumonia started to increase from September 2019 peaking in the winter of 2020. As soon as I am able to get to the data I’ll post the graphical data here.
Yes it seems a great idea to track symptoms changes than try and track COVID and it’s flawed direct stats..
I wonder what the so-called “second wave” would have looked like without the vaccination programme.
From above:
“The first occurred from around February 25th to March 19th 2020, ending after about three and a half weeks, as abruptly as it began. The second got going around December 2nd”
From wikipedia:
“The UK’s vaccination rollout was the world’s first mass immunisation programme when it began on 8th December 2020 after Margaret Keenan received her first dose of two. ”
About 1 million people were vaccinated in the UK during the month of December, and the people who were vaccinated first were those at most risk of infection and death from COVID and most likely to be in hospitals and care homes which, as we know, were and still are the main centres of virus transmission.
Everywhere in the world where a mass vaccination programme has started (and where the virus was already in the community) we have seen a coincident explosion of cases. Most likely because the vaccine depresses immune systems making them more susceptible to new infection (or activation of an existing low-level or dormant infection).
I also wonder about the effect of the flu vaccine rollout. It makes sense that after the flu jab (which I have never had) one’s immune system would concentrate on making antibodies for the specific flu strains, while ignoring infections that might actually be present.
I recall someone (but not who) who made he observation that most of the deaths and hospitalisations in Italy had been vaccinated against flu.
I suspect the flu vaccination this coming season will have the same effect but it will be covered up by the “booster jab” programme. Some idiot said they would inject the covid booster in one arm and the flu vax in the other to save time. . . .
Worth noting that last winter (2020/21) they widened the age range for the ‘flu jab, a bit late in the day (it makes more sense to use it in the Autumn, I think). I didn’t take one, but many might have done. That said, I wouldn’t be surprised if there is a lot of stock to be chucked out when out of it’s shelf life, if they were planning for the range increase, the way it was run.
This is an interesting discussion, but such discussions for me mainly serve to highlight the fact that we do not understand something key about the underlying mechanisms and are flailing around trying to find descriptive accounts that would produce these effects. Nothing wrong with doing that, but in what must surely be a hugely complex multi-variable system with feedback effects, it’s unsurprising that it’s tricky.
As I’ve noted previously, we still don’t understand how flu works, and we’ve been studying that one for centuries.
“I wanted to come back to the question of what causes COVID-19 occasionally to have explosive outbreaks. We’ve had two in England so far. “
Worth noting also that the data appears to show an abortive such outbreak in September/October before the disease properly got going in December.
All very true and further reason for authorities to avoid hasty, massive, damaging, novel interventions.
Absolutely.
As promised, data from Frimley Heath NHS trust
Wasn’t a similar effect observed following the “Hong Kong flu” in 1968 where the “new flu on the block” displaced the other strains for a period, before the new flu became endemic and then the old flu strains staged a comeback?
Lockdown probably contributes to these outburst. Whereas normally the population is homogeneous, in lockdown you get pockets of variants. Each area might have their own mutation strain, and when they interact with each, they get infected with the other strain and you get a burst.
As the majority of ‘cases’ are results of infection in hospitals and care homes, can I politely suggest this analysis is built on sand.
And ‘seasonality’ of virus is as a result of human behaviour patterns and short-term changes in natural local herd immunity levels.
Clearly ‘hay fever’ has now been amalgamated into ‘covid’.
It may be true to say that most actual cases are from hospitals and care homes, but if we’re talking simply about positive test results, I am not sure that’s the case. The table at the bottom of this page https://coronavirus.data.gov.uk/details/testing suggests that many more tests are being done in Pillar 2 (community) than in Pillar 1 (hospitals etc.). What I can’t find is the proportion of each pillar that is positive. Maybe others have found this data.
Ah, ‘but if we’re talking about positive test results’ – that is the crux of the matter, is it not? Just how accurate are the tests in identifying the virus. Not very, it would seem.
used to have these stats reported on websites, but no longer it appears, have to dig deep to find out. What I remember vividly is that false positives were vastly more prevalent in Pillar 2 tests because of the lousy way they were collected and analysed ie it wasn’t just statistical it was physical errors.
Excellent article and analysis.
The Winter 20-21 curve is consonant with a vaccine effect, affecting the vulnerable, on which group there had been no testing. The first spike is essentially the normal autumn rise.
The minor variant issue is unlikely.
The basic problem re. investigation is that the official policy is more interested in keeping up the narrative and sustaining NPIs and vaccination rather than looking at the evidence and the nature of the virus.
BTW – Usual problem with ‘infections’ definition etc.
“To which most people have some immunity”. Exactly so, and proved beyond doubt in the Diamond Princess.