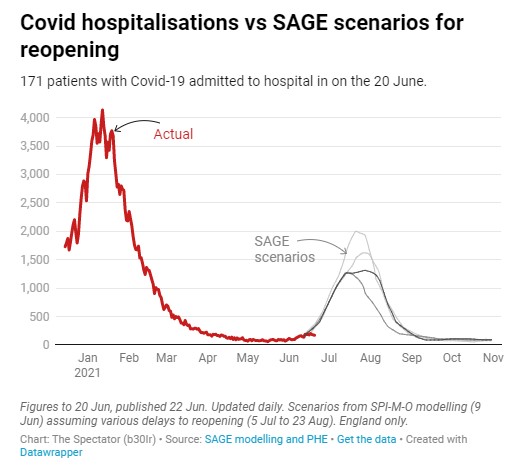
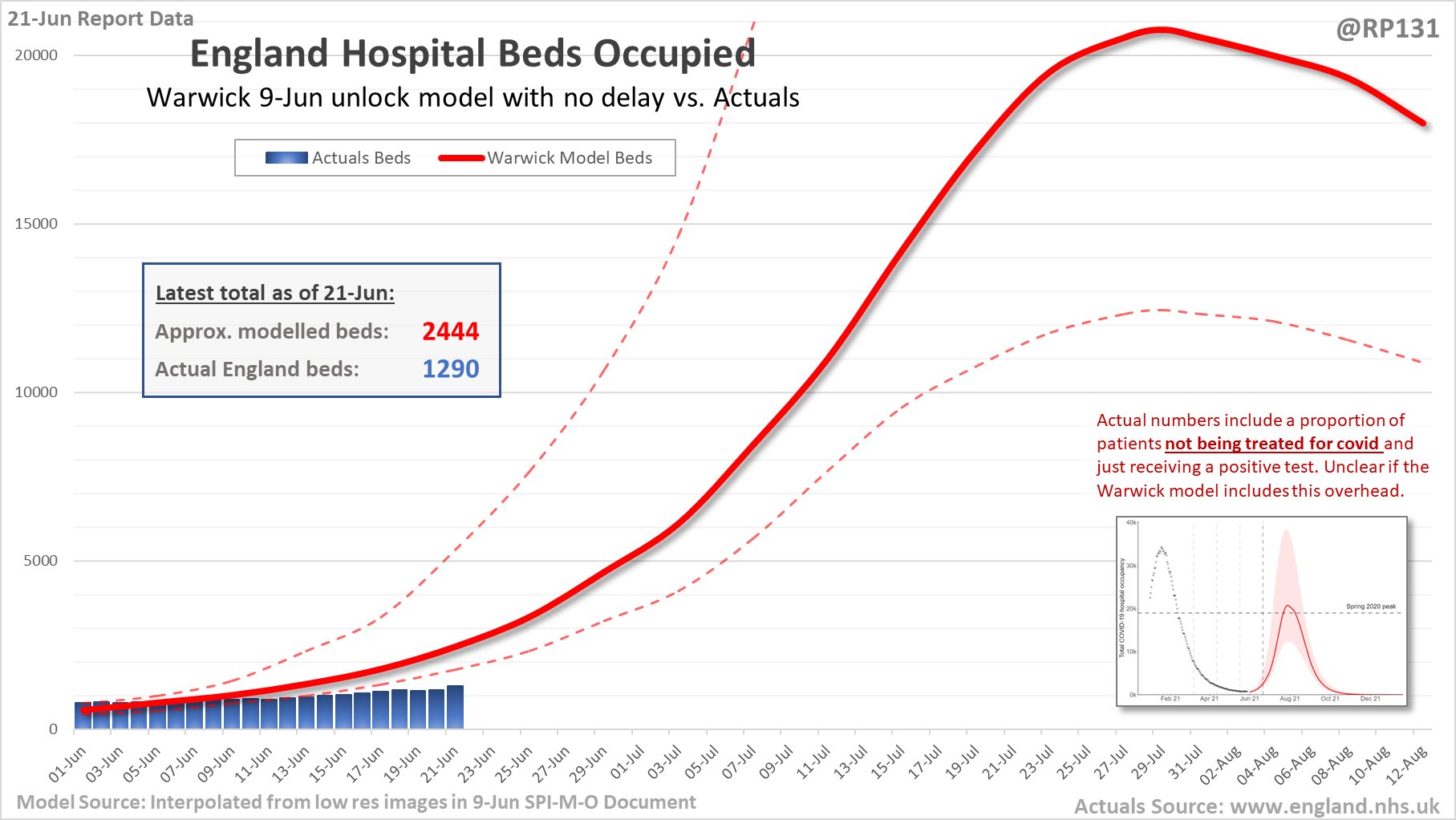
The models the Government is relying on to justify continuing lockdown have not got off to a good start. The projections of the huge summer wave should “freedom day” not be delayed are, as of June 21st (so before any delay could make a difference), almost twice as high for hospital occupancy as the actual number of Covid patients in hospital (see graph above).
Here’s a similar graph from the Spectator with the hospital admissions data superimposed on various SAGE projections (keep track of it here).
Fraser Nelson at the Spectator seems to share our scepticism at Lockdown Sceptics about Government modelling, reminding readers of the notorious SAGE autumn projections that envisaged up to 4,000 deaths a day by early December, but which were inaccurate the day they were published.
However, he then endorses scarcely less pessimistic modelling from Bristol University, which predicts that “hospitalisations peak at just over 900 on August 20th”.
While he admits that “no scenario points to the NHS being overwhelmed” since “Covid patients would occupy 2.5% of hospital beds” (at most), nonetheless he thinks the Government was right to delay the end of restrictions. This is because:
Under the current Dido Harding regime we’d see pubs shut because a waiter tested positive; entire classes of kids pinged and told to self-isolate, offices closed – and, as far as we can work out, on a scale larger than anything we seen so far. There would be anger, confusion – and no shortage of people willing to blame the June 21st unlocking. This would risk panic, damaging the confidence needed to rebuild the economy and society. It would have been a self-defeating liberalisation.
Without a hint of doubt, he asserts: “If we unlock this summer, a big third wave will get underway: it has started now and will become much bigger in days ahead.” In this he is following Professor Philip Thomas, leader of the Bristol modelling team, who wrote in the Spectator earlier in the month: “My model shows an enormous final wave, peaking during the middle of next month at anywhere between two million and four million active infections.” While vaccines are expected to keep hospitalisations and deaths down, this summer wave is still expected to eclipse the winter surge in terms of infections. Fraser explains:
The Bristol model reckons 85% of adults in England have detectable antibodies, with just two-thirds of whole population (i.e., including kids) immune. It assumes the Indian variant is infectious enough to work its way through everyone who remains susceptible, even if they end up with nothing more than a runny nose. The good news is that this will, at least, rule out a winter wave: by September there will be almost nobody left to infect.
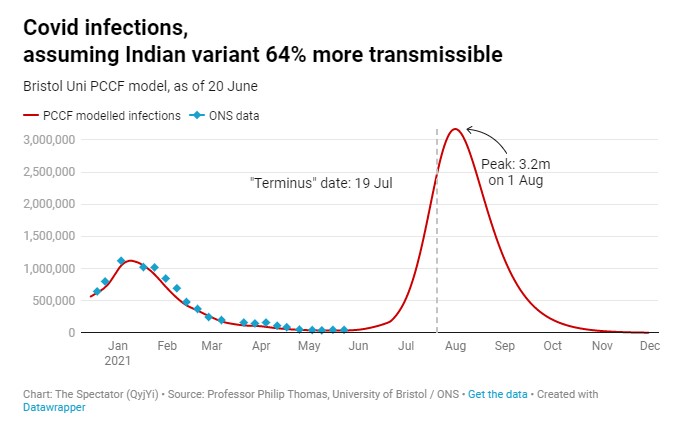
It works on the assumption that the Delta (Indian) variant is 64% more transmissible than the Alpha (British) variant, as per PHE’s claim in Technical Briefing 15.
However, as I noted when the briefing was published, the researchers admit that they did not control for household size. Since there is reason to think the small sample of Delta variant infections is biased towards ethnic groups with larger households, this makes the finding very unreliable (since larger households are more likely to have more secondary infections).
On the other hand, if we look at the secondary attack rate (SAR – the proportion of contacts that infected people infect) of the Delta and other variants as PHE has measured it over time we see that the claims of greater infectiousness fail to account for the fact that this quantity changes over time and tends to decline.
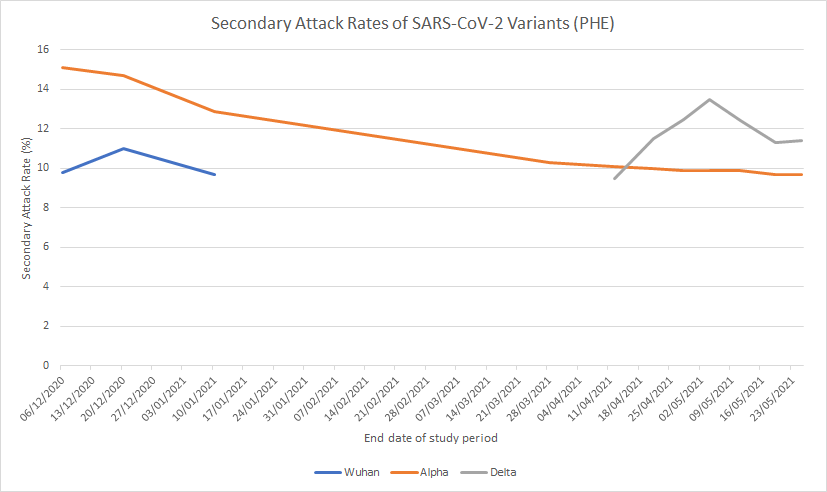
We also see that the Delta variant’s SAR is currently only a little above the Alpha variant’s: 11.4% of contacts infected versus 9.7%, a difference of just 1.7%. In addition, the Delta variant’s current SAR is no different to the Alpha variant’s at the start of March, undermining the idea that it is intrinsically more infectious.
Professor Thomas says he assumes “someone with the Indian variant will pass it on to 6.8 others in a fully susceptible population, a far higher multiple than the Kent variant (4.5 others)”. 6.8 is 51% more than 4.5. However, on the data above, the Delta variant SAR is only 18% higher than the Alpha variant SAR, and 24% lower than the Alpha variant SAR at the start of December. So there is no reason to assume the Delta variant is 51% (or 64% – it appears to have been revised up) more transmissible.
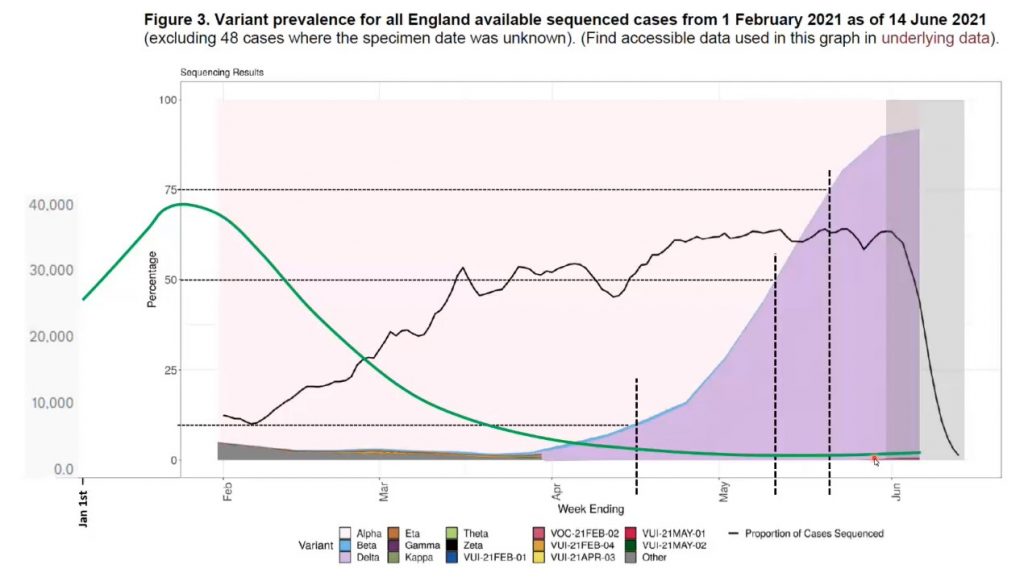
Further countering the idea of a hyper-transmissible Delta variant, Ivor Cummins has shown that the growth in dominance of the Delta variant has not coincided with a spike in infections (see graph below – the green line is positive cases superimposed on a graph of variant proportions, with the Delta variant in purple).
A further big problem with the Bristol model is that it assumes that anyone who does not have “detectable antibodies”, including children, is susceptible to the virus and will inevitably get infected during this summer wave – to the extent that it rules out a winter wave, since “by September there will be almost nobody left to infect”. This is reminiscent of the Imperial modelling from spring 2020 which assumed everyone was susceptible and predicted the majority of the population would quickly be infected.
All such models fail to allow for the fact that even without “detectable antibodies” (and that is an ill-defined concept anyway, as there are different kinds of antibodies and how detectable they are depends on the sensitivity of the test) many people have varying degrees of immunity to viruses like SARS-CoV-2. This is why even at the height of the winter surge, 85% of contacts of those with the new variant in town (then the Kent variant) did not contract the virus. Similarly, according to current data, 85% of those who live with people infected with the Delta variant do not become infected. Why then assume that everyone who does not have “detectable antibodies” will become infected in the next few weeks?
This is not to say that these people are entirely immune and will never be infected by any variant at any time. Viral transmission patterns remain somewhat mysterious, being affected by seasonality (itself likely influenced by temperature and humidity) and by various factors that make people more infectious or more susceptible at a given time. But we have enough data now to know that viral waves and surges will come and go without infecting everyone who is exposed, even if they lack “detectable antibodies”, and even if they may later become infected.
Professor Thomas – and Fraser Nelson – have now nailed their colours firmly to the mast. Professor Thomas is clear that he expects this big final wave regardless of the delay to reopening, as “the model shows that the virus is growing exponentially already; the final step on the roadmap out of lockdown makes little difference”. Within the next few weeks we will see whether he is right that everyone without detectable antibodies (including children) becomes infected. His graph of infections shown above indicates that he expects infections to enter a sustained spike lasting over a month any day now, climbing to over three million people infected by the end of July, so it won’t be long before we know whether his projections are in any way on the money.
If, as I suspect, nothing anywhere like this will come about, will Professor Thomas and Fraser abandon their faith in this simplistic form of modelling that has shipwrecked our country and come round to the more nuanced way of thinking of Professor Sunetra Gupta and others?
We’ll revisit this in a few weeks’ time to see if Professor Thomas and Fraser were right, or whether we need to put these questions to them again.












To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
He is a complete fucking knob! That’s why!
He cannot think for himself, he is doing his masters bidding.
If only he weren’t so bloody indoctrinated, he’s become the Derek Draper to Gordon Brown, but for the fat pig cunt
‘The good news is that this will, at least, rule out a winter wave: by September there will be almost nobody left to infect.’
Holmes: ‘There are over 160 identified common cold viruses, and many more as yet unidentified, against which there are no vaccines. A large number of these viruses are just as lethal to the elderly, infirm, immunosuppressed, obese, as covid 19. That is why the NHS is ‘overwhelmed’ by a ‘winter wave’ every winter and this coming winter will be no different. That is also why overall all cause mortality for 2021 is plumb normal (with thanks, again, to the author of the chart).’
Dr Watson: ‘No shit.’
It constantly annoys me now that the ‘overwhelmed NHS’ is simply accepted as a method for deploying govt policy.
They have had 18 months and spaffed literally billions at useless white elephant schemes when a fraction of that money could have gone to mitigating the problem but instead they did nothing. They built the nightingales and then left them empty.
How can this admittance of failure (for its the govt responsibility that adequate NHS resources be available) simply be accepted 18 months down the line?
Why is no one asking WHY there are not enough beds? The govt have systematically reduced occupancy numbers over the years so they are responsible. Instead they are going to lock everyone up? WTF?
We know the modelling is garbage – nothing new here.
What is new, and what requires investigation, is how Fraser Nelson has been got at to induce him produce such rubbish.
I originally read his article with a mix of shock and amusement. Journalism in this country is now incorrigibly corrupt.
How has the editorial integrity of the editor of The Spectator been so shockingly compromised? That’s the story here.
One of the problems with journalism is the lack of science and maths backgrounds amongst journalists. The other is the collapse of the industry due to advertising moving online. That means papers are wide open to influence from ads and vanity supplements, And that journalists are quickly fired and cheaper, inexperienced ones on short contracts and a promise brought in. They are not in a position to argue with their bosses, and all journalists are thinking about the lifeboat job – and a PR job linked to magic science money is potentially a big lure. This isn’t aimed at FN, it’s a general explanation.
… and the biggest advertiser at the moment is Her Majesty’s Government… Pipers and tunes comes to mind.
“One of the problems with journalism is the lack of science and maths backgrounds amongst journalists.”
A fallacy. Just bring to mind all the ‘scientists’ who are spouting crap.
You don’t have to have a science or maths ‘background’ to understand basic scientific principles – and many who do simply lack the critical reasoning that is the crucial element.
I span both sides of this nominal divide, and what I see is that having a PhD in a particular area does, indeed, give you technical insight into a narrow field, but it doesn’t ensure that you have a grasp of wider scientific reasoning, the weighing of evidence and the fundamental principles of statistical inference outside your own discipline.
What you see is simply bad journalism (‘churnalism’) that also ignores those basics.
Just bring to mind all the ‘scientists’ who are spouting crap.
That’s a good point. Scientists are generally chasing the next bit of grant funding, rather than pursuing knowledge.
Perhaps Sandra’s point may be adjusted to:
One of the problems we face is the lack of science and maths backgrounds amongst the general public.
If vast swathes of the Great British Public hadn’t been so scientificaly ignorant we would never have come to this. Perhaps our journalists, and our politicians, merely reflect a much wider problem with our society.
This is precisely why I cancelled my subscription to The Spectator. It’s now become part of the MSM BULLSHIT WAGON.
Yes, they’re one more dishonest article like that away from me cancelling as well, and I’ll let them know why.
A cynic might observe that they have shot themselves in the foot, if there really is an increase in somewhat harmless infections, with all the graphs moving in the wrong direction (from their perspective), even if they are not real infections (being faked, for example).
The NHS has not been overwhelmed throughout the Covid-19 programme. It has been underwhelmed for long periods. With record numbers on NHS waiting lists, it is the public that has been overwhelmed.
And what does the NHS becoming overwhelmed even mean? What would it look like? All hospitals collapsing at the same time across the UK? It’s another catastrophe meme that doesn’t bear analysis.
Yet it has been an article of faith since March 2020 that the NHS must not be allowed to become overwhelmed. My local MP still cites it as the primary justification for continued restrictions. It will be the rationale for further lockdowns later this year.
The creepy clapping ritual, the TikTok dancing, the privileging of hospital staff at the expense of other workers, the dangling fear of an overrun NHS – of all the emotive and mendacious bollocks cooked up to provide cover for the descent of this country into a medtech fascist shit-hole, the NHS cult has been the most potent and egregious.
Indeed, the NHS as a whole has been twiddling its thumbs, to the chagrin of those good people in it who actually want to do their job.
But of course we’re only allowed to hear from the critical care bedpan changers about how awful it is to watch people die alone in the isolation that they’ve chosen to enforce.
The end-of-life narrative has been weaponised – ‘I held their hand as they slipped away’; ‘We watched helplessly as the oxygen levels plummeted’ etc. Of course it must be harrowing to experience such things but death has been a fact of hospitals for as long as they have existed and none of the sad moments health workers have described over the last fifteen months can have been unique to the Covid-19 period – apart from the cruel and unnatural isolation aspect, as you say.
Absolutely agree. One of the things that made my blood boil during the first lockdown was the sight of self righteous NHS workers, full of their own importance pushing to the front of queues because ‘they’d just come off duty” or “I work for the NHS”, most of the time dressed in their presumably biohazardous uniforms.
Spot on.
Hospitalisations go up: “Lockdown isn’t working, we need more lockdowns”.
Hospitalisations don’t go up: “Lockdown is working, we need more lockdowns”.
Davos will continue to pick whatever models push us to the social credit score apps. Believing otherwise is magical thinking.
I don’t need this government regime to grant me a ‘freedom day’, I’ll decide that, and I did, back in April 2020. April the 8th to be precise.
Articles like this are very interesting but as 16 months of similarly logical and well-researched articles have got us absolutely nowhere with the government, I have had to come to the conclusion that they never will. When will we accept that there is another agenda here and fighting with logical scientific argument just doesn’t seem to be working?
Correct. The government, SAGE et al know it’s all bollocks. Going through a repeated cycle of indignation and exasperation doesn’t change anything.
As can be seen the modellers hedge their bets with ridiculously wide margins of error, relying on Witless and Unbalanced to ignore them when presenting. In the first graph reality is not too far below the lower range (at the moment).
Have any SAGE models ever been right? Even close?
No.
A question I’ve often asked myself (because it would be against the odds not to get something right by chance.
… but I’ve come up with zilch.
… which, given the random probabilities, tends to confirm that this wrongness is, indeed, designed.
Yes, I think there can be little doubt about that. As Yeadon points out, they know what he knows. The only question is whether they are following orders or pursuing their own agendas, or a bit of both – but one could compare it to a gang killing in which all took part in some form or other, willingly and with enthusiasm – they all stand condemned, regardless of whose idea it was to start with.
Fraser Nelson is Boris Johnson’s Bitch
Being wrong is SAGE’s default position. Have they ever got anything right?
I don’t see the problem with everyone getting a runny nose and then being immune, job done and the quicker the better, while the sun is shining and the vitamin D is naturally boosting our immune system. If only we had opened up last summer we would have seen more people exposed to the virus with the sun on their backs rather than in the depths of winter when immune systems are so much less resilient… lockdown kills…
When this ludicrous wall of death fails to materialise they will just say it was the extra monf wot dunnit. There is no arguing with those who prefer delusion.
The Spectator graph states “171 patients with Covid-19 admitted to hospital on June 20”
This is a lie. First of all, Covid-19 is a disease, and I’ll bet my house 171 people were not admitted to hospital because they had a Covid-19 disease and NO OTHER medical problems.
What I imagine happened on June 20 is that 171 people with issues ranging from ingrowing toenails to car accidents gave a positive PCR or LF test result as they entered hospital, and were thus deemed to be suffering from a disease called Covid.
What a disgusting scam the whole thing is. Journalists deserve to be hanged for their part in it.
When has SAGE ever been right? They are malicious liars.
We must remember to keep banging home the point – It doesn’t matter how many people are infected so long as those infections don’t turn into serious or fatal illness. But it’s more than that, isn’t it. In a perfect world we should have the entire population infected (but not suffering illness!). Welcome to the stand – herd immunity!