by Dr. Alan Mordue
During this Covid pandemic I have often wondered about how two key principles central to medicine and public health have been used. The first is the Hippocratic oath “primum non nocere” or “first do no harm”, which all doctors used to swear to abide by on graduation. The second is the precautionary principle, used in public health, particularly where there is uncertainty about the health effects of a proposed intervention or exposure to a potential harmful agent. They often seem to have been applied selectively and even ignored, particularly in relation to illnesses other than COVID-19.
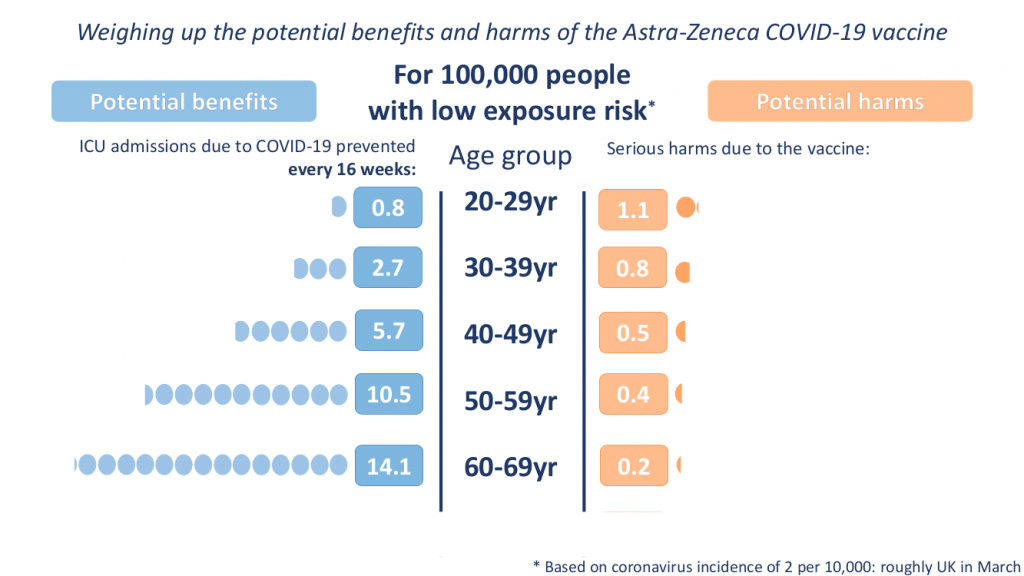
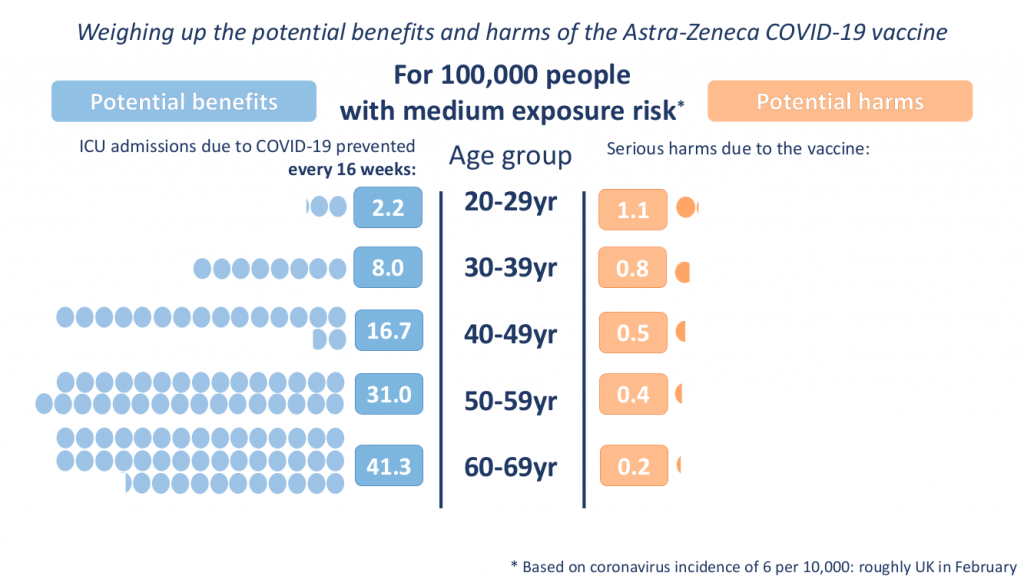
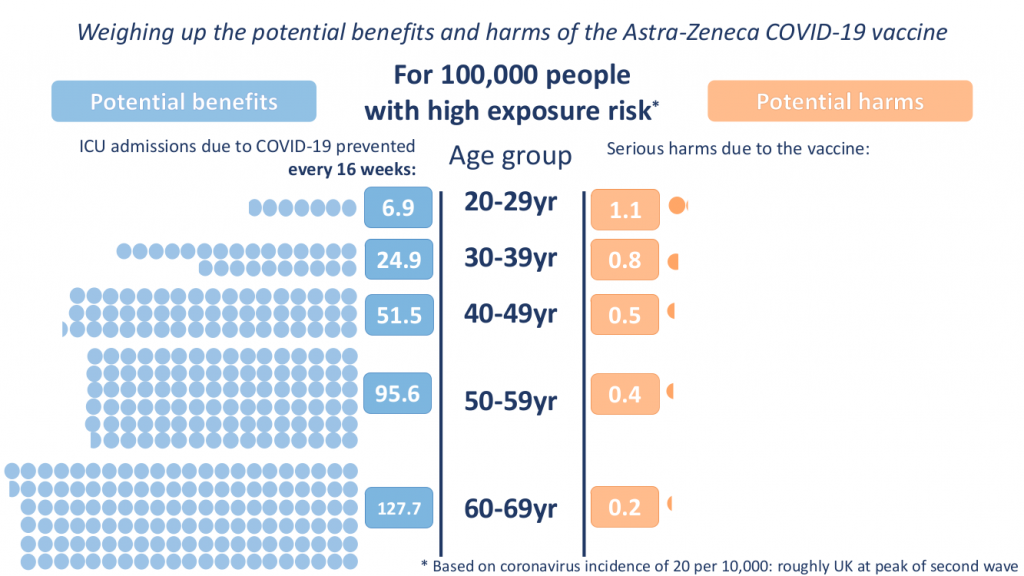
The press conference on April 7th chaired by Deputy CMO Jonathan Van-Tam with representatives from the MHRA and the JCVI about clotting side effects of the Oxford Astra-Zeneca vaccine was a case in point. During the press conference charts showing potential benefits in preventing ICU admission compared to potential serious harms of the AZ vaccine were presented by age group and for three levels of population incidence of SARS-CoV-2 (2, 6 and 20 per 10,000):
The conclusions of the press conference were that these blood clots were extremely rare, that the benefits of the AZ vaccine outweigh the risks, and that an alternative vaccine should be used for those under 30 years without underlying health conditions. These conclusions would appear on first glance to be consistent with these two principles.
Undoubtedly these charts are helpful and a big improvement on the level and detail of information presented to the public during this pandemic, particularly since they present both positive, and unusually, negative effects of the intervention. However, it would have been helpful to know if the baseline risk of ICU admission for each age group included those with underlying medical conditions or not, to avoid over-estimating the benefits for most people.
Given current vaccination uptake, naturally acquired immunity from COVID-19 infections and cross-immunity from other coronaviruses we have almost certainly achieved herd immunity and so widespread transmission at 20 per 10,000 seems extremely unlikely (equivalent to peak of second wave). Therefore I will not consider chart 3 any further.
Clearly we have to accept some risks in life and so too when deciding on medical treatments, so that primum non nocere is really about assessing the risk/benefit ratio and ensuring patients are able to make fully informed decisions. When recommending interventions for healthy individuals, as with the Covid vaccines, a high bar is required, particularly when there is a high level of uncertainty about the incidence of serious side effects (see JCVI statement). So if we assume 10 times more health benefit than risk is required then the 40-49 year group in the low exposure chart could be recommended to have the vaccine, but not the younger groups. At a higher ‘medium’ incidence of COVID-19, perhaps during an autumn/winter 2021 seasonal rise, the 30-39 year group could be included, but still not the 20-29 year olds.
However, what about the potential harms not included in the charts? The AZ vaccine, like all COVID-19 vaccines, is still in the midst of a Phase 3 trial and this will not report on any long-term side effects until early 2023. If we apply the precautionary principle we would want some additional room to accommodate any adverse effects that emerge, so a 15-20 fold difference between benefit and risks would be more reasonable. This begins to point towards 50 years as the cut off; below that the potential benefits may not be justified by the potential risks.
How about switching to another vaccine for the younger age groups? A “course correction” as Prof. Van-Tam called it? Unfortunately, we do not know about long-term side effects of the other vaccines either. For the newer ones there may also be rare side effects yet to emerge, like the blood clots for the AZ vaccine, and for the Pfizer/BioNTech vaccine there are concerns about higher rates of infection and deaths in the weeks immediately after vaccination.
Applying the precautionary principle and primum non nocere, a recommendation to vaccinate only the original nine JCVI priority groups seems more reasonable than all adults over 20 years as currently recommended by the JCVI. That would include all those over 50 years and those who are younger but with underlying conditions putting them at high risk. Such an approach would protect the most vulnerable (through vaccination), stop any significant transmission in the population through existing herd immunity, and anyone below 50 who does contract COVID-19 is likely to have mild or no symptoms and develop lasting immunity, which will help to maintain herd immunity and further protect the most vulnerable.
Finally, there is certainly no case for vaccinating children, who have even lower rates of serious outcomes with COVID-19 than young adults and, given the increasing incidence of thrombosis with thrombocytopenia with decreasing age, may have an even higher risk of experiencing adverse effects as a result of being vaccinated.
Dr Alan Mordue is a retired consultant in public health medicine.










Donate
We depend on your donations to keep this site going. Please give what you can.
Donate TodayComment on this Article
You’ll need to set up an account to comment if you don’t already have one. We ask for a minimum donation of £5 if you'd like to make a comment or post in our Forums.
Sign UpPolice Unable to Deal With Crowds Due to Outdoor Hospitality Rules
Next Post‘First Do No Harm’ Means Not Giving the Covid Vaccine to Young People