
Key points
Vitamin D, contrary to popular thought, is not a vitamin. It is an inflammation-regulating steroid hormone involved in many of the body’s essential processes.1 Leaked NHS internal guidance, issued in June 2020, states that “evidence supports a causal role in Vitamin D status and COVID-19 outcomes”, and urges clinicians to “monitor, report and treat”.2
Meanwhile, a NICE rapid evidence review also published in June, states “there is no evidence to support taking vitamin D supplements to specifically prevent or treat COVID‑19.” However, it does re-enforce its September 2018 advice that at-risk groups should take a 10µg supplement all year round.3
Rewind to March 2018: the ‘world’s biggest quango’ NHS England, released new guidance not to issue Vitamin D and many other commonly available over-the-counter (OTC) medicines on prescription, which was intended to save NHS costs by promoting patient self-care.4
Vulnerable elderly care home residents, many of whom lack mental capacity, are unable to obtain Vitamin D without a prescription, as Care and Quality Commission (CQC) regulations prevent tablets being given by care staff without GP Guidance.5
This logistical deadlock has not been resolved, and Vitamin D deficiency has long been known to be widespread in care homes.6 Over 19,000 care home residents in England have died with COVID-19, representing at least 36% of all COVID-19 fatalities in England and Wales.7 8
Defining evidence: why the different guidelines?
Evidence is increasing that Vitamin D deficiency is causally linked to both likelihood of contracting COVID-19, and severity of infection.9
The NICE rapid evidence review,3 which states there is “no specific evidence” for Vitamin D in COVID-19, is heavily focused on the outcomes of the eight included studies, without corroborating this with the known physiological mechanism for how Vitamin D attenuates the inflammatory cascade in the lungs with coronaviruses.10 The physiology surely somewhat dispels the caution that NICE have that the correlation between low Vitamin D and severe COVID-19 may be incidental, or weakened by potential ‘confounders’. Confounders are factors which account for, or mask, an association. However, the confounders that the NICE review3 claim weaken three of the included studies could may actually strengthen when causal inference is considered. These confounders mentioned by NICE for Covid-19 severity included obesity, high blood pressure and socio-economic status: these are all independently linked to low vitamin D status.11 12 13 Could Vitamin D status, therefore, be the common link? The physiological mechanism would support this. The NICE rapid evidence has excluded relevant data on countries affected by COVID-19 and their latitude, showing countries such as the UK, who are above the 30 ̊north latitude line, meaning there is not enough light for the skin to make Vitamin D all year round. Interestingly, in the UK, there is not enough sunlight between October and March, 6 meaning deficiency would be at its peak in the population at the end of March.
In short, the leaked report, now a published study,2 is more comprehensive and credible than the NICE rapid evidence review, as it includes all the circumstantial as well as the forensic evidence.
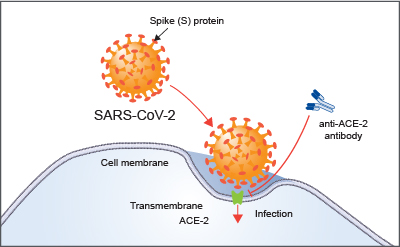
Figure 1: SARS-CoV-2 enters the cell via the ACE-2 receptors within the renin-angiotensin system (RAS). Image courtesy of R&D systems.10
How vitamin D protects against COVID-19
Vitamin D acts to re-balance the renin angiotensin system (RAS). This is a hormone system that regulates blood pressure, fluid balance and vascular resistance. It is the dysregulation of the RAS that creates the pro-inflammatory cytokine storm in COVID-19, triggering the potentially fatal severe acute respiratory infection. Vitamin D moderates the RAS by binding to the ACE 2 receptor cells, attenuating the inflammatory response and lung injury. 9 10
Known risk factors and vitamin D status
Well-known risk factors for COVID-19 have been well publicised to be age, obesity, ethnicity and socio-economic status. While there are social factors at play that increase risk for some groups, could Vitamin D also provide a physiological reason these groups are also at risk of severe COVID-19 infection? A very interesting study conducted in Israel showed that COVID-19 outcomes were worse in communities where traditional dress was worn, and where individuals had poor vitamin D status. This took into account and adjusted for baseline characteristics such as age.14
Table 1: Some better known risk factors for Covid-19 and their known link to Vitamin D deficiency
| Risk Factor | Linked to low Vitamin D? | Linked to Covid-19? | ||
| Ethnicity | | Darker skin less able to absorb. If cultural clothing covers skin, UV light cannot be absorbed 14 | | BAME communities identified in UK as more susceptible |
| Obesity | | Vitamin D is fat soluble, and dilutes into fat cells, making it less available13 | | Obese identified as more likely to require ICU admission for COVID-19 |
| Socio-economic status | | An independent risk factor for Vitamin D deficiency11 | | Thought to be due to social factors such as working in hospitality and living in densely populated areas. |
| Type II Diabetes | | VD protects against T2 diabetes by reducing parathyroid levels1 6 | | NHS trusts reported in spring that type II diabetics were more likely to require ICU treatment |
| Older age | | Skin is less able to absorb with age3 6 | | The majority (estimated 74%) of COVID-19 deaths have occurred in over 70s. |
Death stats for nerds
The evidence is increasingly undeniable that Vitamin D is linked to COVID-19. We also know that Vitamin D is not routinely given to residents in care homes,5 and in general, the guidance to take supplements is not widely promoted. Could this be partly to blame of the shockingly large number of deaths this year in England’s care homes?
The following data have been compiled by this author from the published ONS Excel spreadsheets on deaths in care homes,7 and total deaths attributed to COVID-19 in England and Wales8 with some totals and percentages worked out, so they can be viewed in a context that wouldn’t be seen on the BBC news.
Table 2: Covid-19 Death statistics for care homes in England
| Percentage of all COVID-19 deaths (England and Wales) who are care home residents in England* | 36% (19,726 of 54,678) |
| Percentage of deaths of all causes (England and Wales) who were care home residents in England | 17% (84,740 of 494,975) |
| Percentage of care home COVID-19 deaths that occurred in the care home and not in hospital (indicating only palliative treatment offered) | 75% (14,722 of 19,726) |
| Percentage of all England and Wales COVID-19 fatalities over 80 years of age | 61% (33,352 of 54,678) |
| Percentage of all England and Wales COVID-19 fatalities over 70 years of age | 74% (40,696 of 54,678) |
*This is likely to be an underestimate, as ONS state that deaths recorded early in the pandemic were not attributed to COVID-19. 8
A shocking 36% of all deaths in England and Wales attributed to COVID-19 have been of care home residents under NHS England. These are the most vulnerable in our society, and have already been failed in many respects through the pandemic, as limited resources and PPE were prioritised for the NHS.
Ambiguity and conflicting guidelines preventing treatment
Before Vitamin D was linked to COVID-19, there was already an inequality with Vitamin D provision, detailed in this study. A Catch-22 between the NHS England prescribing ban, the CQC strict policing of supplement administration, and a failure of Local Authority Public Health promotion of existing guidelines (10µg per day), meant that giving much-needed Vitamin D supplementation to care home residents fell through a large but unnoticed gap between different agencies’ responsibilities, rules and regulations.4 5
Given that most of the deaths from COVID-19 occurred in care homes and not in hospital, we may never know how many of these were vitamin D deficient, as recent blood tests are less likely to be available. However, the circumstantial evidence is stacking up well that this failure may have contributed to the care home death toll.
The million dollar question is, was NHS England’s do not prescribe guidance ever intended for care home residents in the first place? The document describes items not to be routinely prescribed in primary care. Primary care by definition, is ‘first’ point of contact care, e.g. an independent person rocking up to their GP and requesting a prescription. Quite rightly, if this prescription request is for something cheaply and easily available at the pharmacist, that person should go straight there. However, it could be argued that care home residents are not directly linking in with primary care, but their main source of care is in the tertiary/social care sector. Therefore, the NHS England prescribing guidance is arguably not applicable to them. Were local Clinical Commissioning Groups (CCG’s) ever intended to issue guidance that a care home resident with limited capacity should be responsible for their own Vitamin D as ‘self-care’, when all their other medications would be controlled on their prescription? Or was this a tragic error of interpretation by CCG’s of what is actually shockingly ambiguous guidance?
We don’t have the answer to that now, but this author has submitted a Freedom of Information request to obtain it. So within 20 days, we may have.
If the answer is no, then vulnerable care and nursing home residents have been left without a simple and cheap treatment that could have protected them from COVID-19 because of a misinterpretation of an ambiguous guideline, and because no-one along the chain of events sought to clarify it. If the answer is yes, it was intended for care home residents, then the next question is – why?
That answer is in the guidance – it’s to reduce NHS prescribing costs. But by now much? The recommended dose required to maintain good blood vitamin D levels and to prevent deficiency is 10µg, equivalent to 400 International Units (IU’s).6 Two months’ supply of a 100IU tablet (taken every other day, giving 12.5µg/500IU’s per day) can be obtained for as little as 59p by the NHS. That’s a cost of 30p per patient per month.15
Conclusion
The combination of loneliness, lockdown, and denial of a cheap and evidence-based treatment amounts to an abysmal failure of the most vulnerable members of our society. As we are locked down again, and the economy left to likely ruin, why is this safe, well-evidenced and ridiculously cheap treatment being ignored? This has to stop now. NHS England must review their position, and allow for and actively promote prescribing to those who cannot buy Vitamin D. If this Government really cared, instead of ‘stay home, protect the NHS, save lives’, they would stay ‘stay sane, take vitamin D, you could survive’.
References
1 Bilke, D.et al.: Vitamin D, an ancient hormone. Available at https://onlinelibrary.wiley.com/doi/abs/10.1562/2005-02-02-IR-430. Accessed 5th November 2020.
2 Davies, G. et al.: Covid-19 and Vitamin D information. Available at https://docs.google.com/document/d/1jffdZOSuIA64L_Eur8qyCQ12T7NXrHSKPxtMe134C0Y/mobilebasic?fbclid=IwAR0lYaw5dKPFd-vUmvTm5GD8uZYZ_E6Hl9SSj32FjuuCkJBy-YB6heKy30w. Accessed 4th November 2020.
3 National Institute of Clinical Excellence: COVID-19 rapid evidence summary: Vitamin D for COVID-19. Available at https://www.nice.org.uk/advice/es28/evidence. Accessed 4th November 2020.
4 NHS England: Conditions for which over the counter items should not be routinely prescribed in primary care. March 2018. Available at: https://www.england.nhs.uk/wp-content/uploads/2018/03/otc-guidance-for-ccgs.pdf. Accessed 4th November 2020.
5 Williams, J et al.: Responsibility for vitamin D supplementation of elderly care home residents in England: falling through the gap between medicine and food. Available at https://www.medrxiv.org/content/10.1101/2020.06.21.20136697v1. Accessed 5th November 2020.
6 SACN (Scientific Advisory Committee on Nutrition). Vitamin D and health. London, 2016 https://www.gov.uk/government/publications/sacn-vitamin-d-and-health-report
7 Office for National Statistics: Number of deaths in care homes reported to the Care Quality Commission. Available at https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/numberofdeathsincarehomesnotifiedtothecarequalitycommissionengland. Accessed 4th November 2020.
8 Office for National Statistics: Deaths registered weekly in England and Wales, provisional. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/weeklyprovisionalfiguresondeathsregisteredinenglandandwales. Accessed 4th November 2020.
9 Davies, G. et al: Evidence supports a causal role for Vitamin D status and Covid-19 outcomes. Available at https://www.medrxiv.org/content/10.1101/2020.05.01.20087965v3. Accessed 4th November 2020.
10 R&D systems: ACE-2: The Receptor for SARS-Cov-2.AVilale at https://www.rndsystems.com/resources/articles/ace-2-sars-receptor-identified. Accessed 4th November 2020.
11 J Léger-Guist’hau et al. Low socio-economic status is a newly identified independent risk factor for poor vitamin D status in severely obese adults. Available at: https://pubmed.ncbi.nlm.nih.gov/27524803/. Accessed 4th November 2020.
12 Pils, S. et al.: Vitamin D status and arterial hypertension: a systematic review. Available at: https://www.nature.com/articles/nrcardio.2009.135. (Abstract). Accessed 4th November 2020
13 Walsh, J. et al.: Vitamin D in obesity. Available at https://pubmed.ncbi.nlm.nih.gov/28915134/. Accessed 4th November 2020.
14 Israel, A. et al.: The link between vitamin D deficiency and Covid-19 in a large population. September 2020. Available at https://www.medrxiv.org/content/10.1101/2020.09.04.20188268v1.full.pdf. Accessed 4th November 2020
15 drugtarriff.co.uk: https://www.drugtariff.co.uk/DrugInfo/drugdetails.aspx?doseid=580784. Accessed4th November 2020.











Donate
We depend on your donations to keep this site going. Please give what you can.
Donate TodayComment on this Article
You’ll need to set up an account to comment if you don’t already have one. We ask for a minimum donation of £5 if you'd like to make a comment or post in our Forums.
Sign UpLatest News
Next PostLatest News