In a study published earlier this year, Paul McKeigue and colleagues analysed data on all diagnosed cases of COVID-19 in Scotland, as well as a large number of matched controls. They found that a staggering 30% of severe cases (those that resulted in critical care admission or death) were linked to a recent hospital visit.
This suggests widespread nosocomial transmission of SARS-CoV-2. In other words, a lot of people caught their infections in hospital, and then became seriously ill.
The fact that such a large portion of severe cases were linked to a recent hospital visit is actually not so surprising. After all, people vulnerable to COVID-19 (the elderly and persons with underlying health conditions) are overrepresented among those who make frequent hospital visits.
Nonetheless, it’s rather concerning that hospitals – places where people are meant to come out healthier than they go in – were a major site of SARS-CoV-2 transmission.
Given that COVID-19 patients, as well as those vulnerable to COVID-19, tend to be concentrated in hospitals, making efforts to reduce nosocomial transmission would seem like a top priority. Indeed, one would expect interventions that did reduce such transmission to have a large benefit/cost ratio.
Which makes a new preprint so interesting. Andrew Conway-Morris and colleagues investigated whether airborne SARS-CoV-2 could be removed from hospital wards using portable devices that filter and sterilise the air.
Their experiment involved two units within an English hospital: an ordinary Covid ward, and an ICU containing Covid patients. The presence of airborne SARS-CoV-2 was measured during three consecutive weeks: one in which the devices were turned off; one in which they were turned on; and one in which they were turned off again.
In addition to measuring the presence of SARS-CoV-2, the researchers measured the presence of various other microbial bioaerosols, such as E. coli and staphylococcus. Their results for the Covid ward are shown in the figure below.
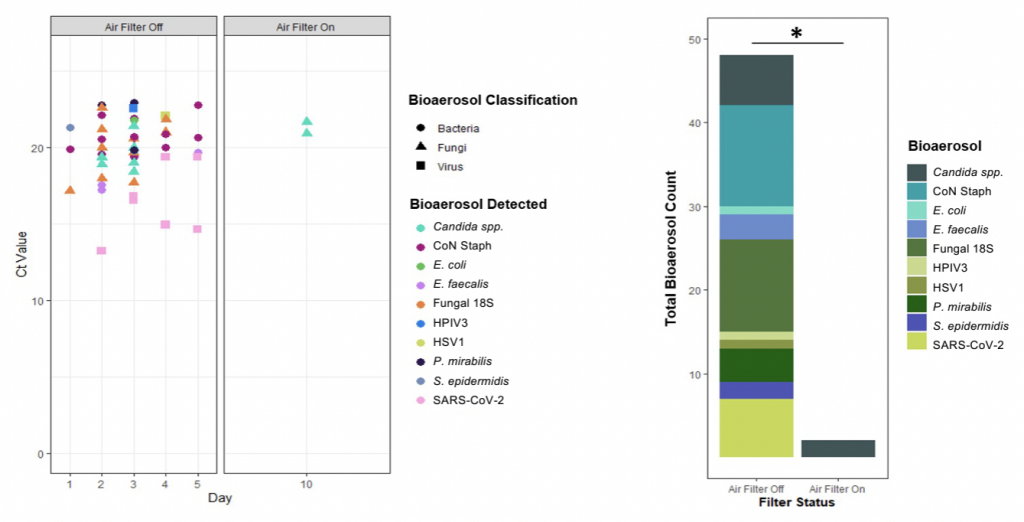
When the devices were turned off, many microbial bioaerosols (including SARS-CoV-2) were detected. Yet when they were turned on, all of these except candida were undetectable. This means the devices were successful in removing not only SARS-CoV-2, but also other potentially dangerous pathogens.
As the authors note, SARS-CoV-2 was detected on “all five days before activation of air/UV filtration, but on none of the five days when the air/UV filter was operational”. The virus was again detected on “four out of five days when the filter was off”.
Interestingly, SARS-CoV-2 was barely detected in the ICU (regardless of whether the devices were turned on). This may be because viral shedding is lower among critically ill patients, or because ICU staff were wearing proper N95 masks.
It’s important to note: the study didn’t show that the devices actually prevent transmission of SARS-CoV-2 in hospitals. However, the results constitute strong circumstantial evidence that they would reduce transmission.
While attempting to halt transmission of SARS-CoV-2 in the community at large is costly at best and futile at worst, attempting to do so in high-risk hospital environments makes a great deal of sense. Further investigation into the efficacy of these devices is clearly warranted.











To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.