NHS England guidance promoting universal masking in healthcare settings was quietly dropped on June 1st as part of the government’s ‘Living with Covid’ plans. So how is it that some hospitals and clinics seem to be making their own policies, with some mask-free and others aggressively insisting on masking both staff and public?
The reason is that the new guidance made masking policies a matter for local discretion. As a result, national COVID-19 guidance can be trumped by so-called ‘local COVID-19 prevalence’. But how consistent are local responses? By what set of rules are decisions to reintroduce masks made? And, most importantly, who is responsible for determining the rules and making decisions?
A return to masking?
Early in October, mainstream news outlets were reporting on the ‘return of the mask’. Between the Mail and the Sun’s accounts, eight different NHS Trusts were reintroducing a range of Non Pharmaceutical Interventions (NPIs), prominent among which were mask mandates for patients and visitors.
In all cases, these measures were apparently being introduced as a result of ‘Covid’s resurgence’ with “surveillance data suggesting Covid is on the rise in England”.
Just a month on from these heavily publicised reintroductions of mask ‘requirements’, the picture had changed somewhat. Table 1 shows the current status of mask requirements for the public. In some cases, the trusts who saw the need for restrictions have relaxed them, but they remain in full force for others.
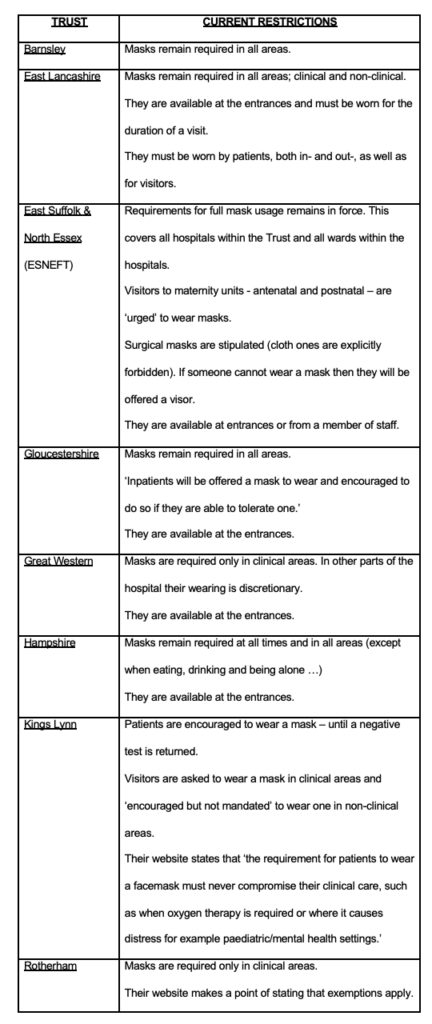
It is clear from the hotchpotch above that not all NHS Trusts are acting the same. Perhaps ‘local prevalence’ of COVID-19 can explain why we are seeing these differences? To test this hypothesis we can look at the infection ‘case’ rates in each of the domains covered by the Trusts, as documented in Table 2.
We should expect those Trusts imposing mask mandates to be in areas of above-average Covid prevalence. But, certainly at a high level, this appears not to be the case. Instead, there is no discernible pattern and, in fact, some discrepancies. For example, Barnsley, with continuing significant restrictions, has a catchment area with the lowest daily new cases per 100,000 people; while Swindon and its surrounding areas in Wiltshire, served by the Great Western Trust that has reduced its mask restrictions, has the highest rate!
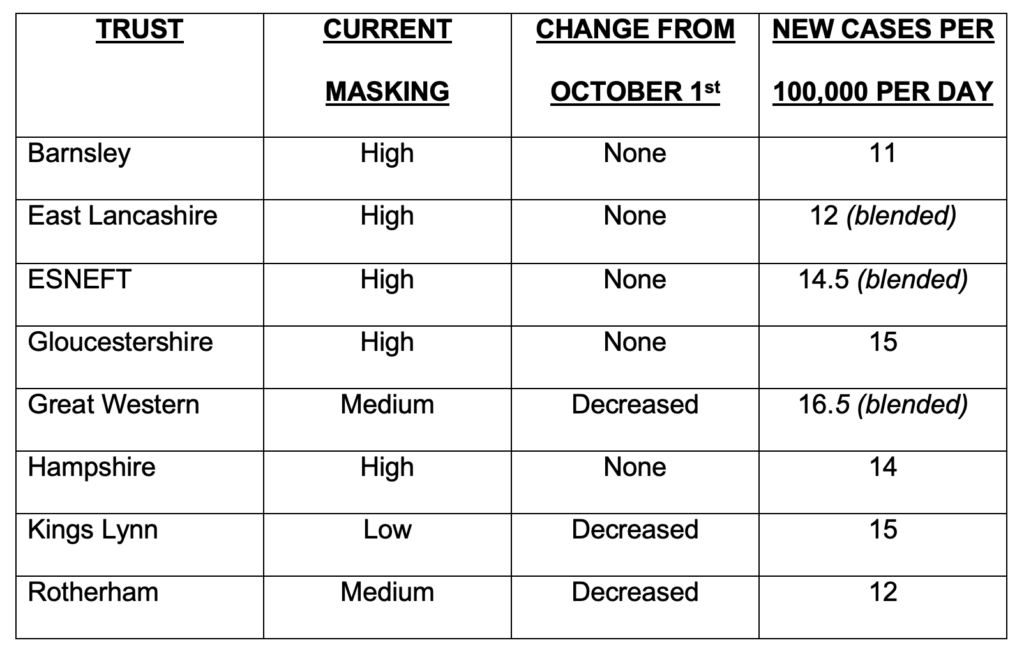
Source for ‘Cases’: GOV.UK Coronavirus (Covid-19) in the UK https://www.covidlive.co.uk
If local mask ‘requirements’ aren’t stipulated in national guidance, and ‘local prevalence’ of COVID-19 doesn’t explain it either, what’s going on?
Essex: a case study
Draconian masking – and other NPI measures – remain in place within the East Suffolk & North Essex Foundation NHS Trust (ESNEFT). This body runs the major hospitals of Colchester and Ipswich as well as several smaller community hospitals in the surrounding areas. It is worth noting that within ESNEFT’s bailiwick lie some of the most deprived areas of the entire country which also have some of the highest suicide rates.
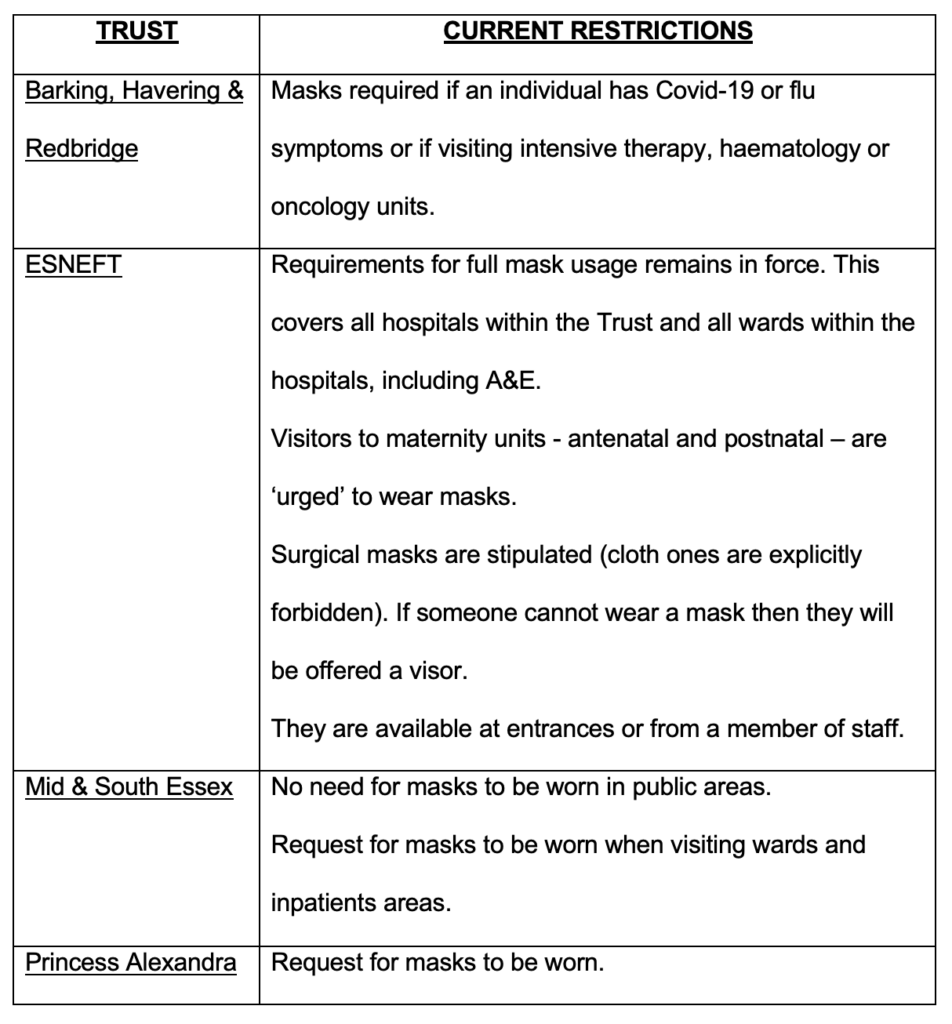
In addition to ESNEFT, three Trusts provide healthcare services in Essex. Each Trust runs multiple hospitals and covers specific geographic areas. How, in terms of mask mandates, does the ESNEFT Trust compare to the others? Table 3 documents the face covering requirements at the health establishments run by the other three Trusts operating in the county and reproduces the rules at ESNEFT.
The profile of a masking decision-maker
The man responsible for ESNEFT ratcheting the restrictions upwards is Giles Thorpe, Chief Nurse and Director of Infection Prevention & Control (IPC).
Doctor Thorpe is not a medical doctor, rather he is a “senior nurse leader” and an “honorary professor”, with a professional doctorate in health service management awarded by the University of Essex in September of this year. If you were uncharitable you might say he was an NHS bureaucrat. “Once you accept that some part of you might be racist, you may then need to accept your white privilege,” Thorpe is quoted as saying in an NHS website article entitled “From bystanders to activists”. Indeed, sensitivity to racism appears high on the agenda at ESNEFT. In 2019 Thorpe’s boss, Trust Chief Executive Nick Hulme, went on record to declare that the region his Trust provides health services to was “probably the most homophobic, racist, awful place in some senses to live in the country”; his track record as an actual administrator of health services meanwhile appears somewhat chequered.
When it comes to countering COVID-19, Dr. Thorpe is an earnest observer of infection rates within the Trust’s catchment and a firm proponent of NPIs in general, and masking in particular. For example:
● June 2021: In his first IPC annual report, without supplying any evidence to back up his assertion, Thorpe noted that “causes of COVID-19 outbreaks in the hospital wards” were, in part, due to “lack of offering patients to wear masks (sic), and lack of uptake by patients to wear a mask”;
● December 2021: just in time for New Year, ESNEFT suspended visiting rights for their health venues. Dr. Thorpe was quoted in the press as saying that “by keeping a close eye on community COVID-19 infection rates and the number of people in our hospitals with the virus, this is action we really need to take now”;
● January 2022: Due, according to Thorpe, to “a rise in positive coronavirus tests among pregnant people (sic)”, new rules restricting visits to maternity units in east Suffolk and north Essex were put in place;
● March 2022: Faced with rising infection rates, visitors were banned completely from ESNEFT venues, with Dr. Thorpe commenting that the Trust was “committed” to reinstating some ward visiting “as quickly and as safely as possible”;
● April 2022: Notwithstanding falling COVID-19 community infection rates, the Trust kept visiting restrictions in place, although Dr. Thorpe said: “We did manage to open some visiting for patients who have been in hospital for more than seven days before the Easter weekend.”
Given the lack of robust evidence to support mask-wearing, and the known harms, particularly in healthcare settings, the Smile Free campaign recently wrote to Dr. Thorpe, posing the following questions:
● What robust, real-world evidence are you drawing on to support the re-imposition of mask requirements?
● Do you believe that the evidence for masks significantly reducing viral transmission is sufficiently strong to justify insisting all staff, patients and visitors wear them?
● Given the wide range of potential physical, social and psychological harms associated with habitual masking, have you conducted a comprehensive risk/benefit assessment addressing the likely consequences of this policy decision?
● Including both the wholesale cost of the surgical masks, together with the salary of the monitors at the hospital entrances, how much is your Trust spending each year on implementing your mask requirement? Given the huge financial pressure the NHS is under, do you believe that this is optimal use of tax-payers money?
● It is admirable that you recognise the importance of “patient experience”. But what’s the likely impact of mass masking on the experience of a confused, elderly, hard-of-hearing person in one of your medical wards or a frightened child, in acute pain, attending your Accident & Emergency Department?
● It is admirable that you seek to give a voice to the “lesser heard groups” and to ensure that the “stay silent” groups are heard. But in re-imposing your mask requirement have you listened to your autistic patients, or those with histories of physical and/or sexual abuse, or those with recurrent panic attacks, many of whom suffer extreme levels of distress as a direct consequence of face coverings?
Dr. Thorpe replied, without answering any of the substantive questions. Confusingly, he said “we support and respect anyone’s decision to wear a face mask, or not, while they are in our hospitals”, while in the same email confirming universal masking had never gone away in “A&E, our urgent treatment centres, and assessment areas (and) areas where we treat immunocompromised patients”, and saying “we reintroduced mask wearing for visitors to our wards in September”.
No doubt Dr. Thorpe believes he’s doing the right thing. It’s just a shame that the 10,000 patients reportedly seen every day at ESNEFT are still being subjected to safety theatre with no evidential backing, going into a third year of the Covid saga, seemingly driven by a very small and unaccountable infection control team, if not in reality the whims of one man. If your local healthcare setting is still insisting on masks, find your ‘Giles Thorpe’ and ask him or her or they the same set of questions.
Perhaps we should not be surprised, because the over-valuation of masks goes to the very top of the NHS. As recently as October 4th, Dame Ruth May, Chief Nursing Officer and national lead for infection control at NHS England, was justifying mask advice to hospitals with “highly uncertain” computer modelling linked to Professor Neil Ferguson’s Imperial College that is literally labelled “Should not be used to inform clinical practice” on page one.
As Smile Free wrote in June when the NHS guidance changed, “two years after the imposition of masking in English hospitals, it is most regrettable that NHS England and the authors of this latest guidance (Professor Stephen Powis and Duncan Barton) could not simply have signalled a clean break and consigned this unprecedented, poorly-evidenced, and ultimately failed policy to history. Since they have chosen not to, by far the most likely outcome is that masking in English hospitals will now become a ‘postcode lottery’ based on the whims of local staff.“
And so it has come to pass.
Stop Press: A new RCT has concluded that N95 masks are no more effective at stopping transmission of the virus than ‘regular’ medical masks. The Brownstone Institute has more.












To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
He should be locked down, hermetically sealed in his own personal cocoon, then he would be quite safe and need not worry about the rest of us. We’ll manage.
This guy knows perfectly well that Sars-CoV2 was never a substantial danger for anyone. He’s just convinced that our way of life is too unhealthy on a planet notoriously ridden with pathogens and thus, needs to be abolished because he and he only is the guy who knows exactly how everything needs to be done to be done properly. A megalomaniac who’s really convinced that he’s a god. People like this should be locked away in padded cells to ensure that they’ll neither harm themselves nor anyone else.
A Padded Cell lined with sharp stuff !!..
I think he would welcome being put to sleep as he would no longer need to fear us or the numerous virus that share the earth with us, I am happy to chip in a couple of quid for him to have a seat on the plane to dignitas.
I will second that.
You could say that the more someone seems intent on “saving” others the more of a danger he is to others.
Someone who is fanatical about saving the entire global population is a egomanical lunatic and an absolute menace.
The worst tyranny always comes from those who terrorises you “for your own good”, because they never sleep.
C.S. Lewis said it best. It is better to be ruled by robber barons than by omnipotent moral busybodies.
He’s not scared. He is, in his own words, a Fascist and a power junkie.
I think he is mostly terrified of his impending demise.
The proper way to handle dangerous, stubborn idiots who are unwilling to learn from their mistakes is to go a bit all medieval on them.
It’s a shame he’s not British
Let these people expose themselves for what they are, and a few more people will wake up
If I met this man in the street I would be very tempted to biff him on the nose…and I’m not a violent man at all. To think of all the pain, loneliness and broken lives it caused for something with well over a 98% survival rate. If indeed there is a next time, let’s lock him up in a small trunk and he can enjoy his lockdown all by himself.
“It’s a map for what is very likely in store for us courtesy of the ‘pandemic planning’ industry. Read it and weep. Or read it and resist.”
I don’t care what their plan is.
I will NOT comply!
Well said, HP! I’m with you.
Thanks Aethelred
Seriously, NEVER AGAIN. Full stop, with NO asterisks!
An interesting ‘stack from Dr Malone, as he focuses on Davos, ‘Disease X’ and also highlights the important work of Brian Bantugan in exposing the corruption of the WEF and the WHO. ”We won’t get fooled again”. ( That’ll be the legit ‘Who’ )
”It is Davos (World Economic Forum) week and the MSM hysterical propaganda push from the globalists regarding “disease X” is in full swing.
Almost every major news outlet in the world has run black propaganda pieces about disease X. Why do I write black propaganda – because the “experts” aren’t actually named, the peer-reviewed papers supporting the thesis of “a deadly pathogen causing 20 times more deaths than COVID-19” or “killing 20 times more people than COVID-19” or “killing 50 million people” are non-existent. Yet these narratives are all headline news in main stream media.
Right now, Disease X and One Health are being propagandized in the main stream media as being the solution to save the world from a massive die off – this propaganda is being driven by the WEF in collaboration with the WHO. The Ecohealth Alliance is also at the forefront of the One Health initiative and has collected millions of dollars for their research projects into One Health. The Davos meeting is being used to prop up support for the WHO Pandemic treaty that removes national sovereignty over public health by promoting.
The WEF and the WHO envision solutions to the imaginary “Disease X” that involve more loss of freedoms. They want control over food systems, more money, more censorship, more surveillance, control over the climate change agenda – all in the name of public health. But even worse, they want all this codified in a document that the turns over national sovereignty to the WHO.”
https://rwmalonemd.substack.com/p/disease-x-and-the-corrupt-lancet
Massive die off?? Maybe the “Disease X” is actually going to be the consequences from the jibby jabbys, wrapped up as a new illness, an opportunistic leap following the failure of the vax pass licenses to live.
Indeed, the powers that be are literally saying the quiet part out loud now.
You can’t fix stupid
I assume Mc Neil speaks from inside a pressurised, clean oxygen safe room in which he lives for 24 hours a day and has no contact with any living life forms, if not then step up onto the plate another rank hypocrite with a hatred for humanity, the “virus” is still with us, but so are lots of other diseases, so Mc Neil must surely be terrified that he may contract or carry one of these little critters. But of course he doesn’t live that way, he just wants to play God with other people.
GFY
And the horse he rode in on.
Sometimes it does seem appropriate if a lone wolf just takes someone out – for the greater good, of course.
Imagine the benefit to humanity if a lone wolf had dealt with Hitler, before he achieved unfettered power.
There were a few attempts long before the bomb in the Wolf’s Lair. And early ‘conspiracy theorist’, saw Hitler as some kind of Antichrist and planted a bomb in a Clock, but Hitler often changed arrangements at the last minute and the plot was discovered.
He actually thinks Medieval medicine is the gold standard for fighting pandemics?
He must be all in with the Science Must Fall movement?
https://www.youtube.com/watch?v=C9SiRNibD14&t=101s
Science Must Fall?
Again, quiet part out loud.
‘……..the Western focus on personal liberty above all else can kill”
An exponent, then, of Socialist Fascism.
‘Anti-individualistic, the Fascist conception of life stresses the importance of the State and accepts the individual only in so far as his interests coincide with those of the State, which stands for the conscience and the universal, will of man as a historic entity. It is opposed to classical liberalism which arose as a reaction to absolutism and exhausted its historical function when the State became the expression of the conscience and will of the people. Liberalism denied the State in the name of the individual; Fascism reasserts.’
Benito Mussolini 1932
McNeil’s epitaph (and that of Pantsdown): ‘He thought he was an expert.’
Here is the other Socialist, Mr A. H. giving a speech where he talks about freedom of the individual (or not, in this case). ANd notice the use of socialist words.
“…For you must also understand this, my people’s comrades: No leader can use more strength than his followers give him! What am I without you? What you do not give me, I can never use for your own benefit! If you refuse me your unanimous unity, what should I do?! I am a single man, I can possess the best will. The will is not worth more to you than your will is worth to me! And that brings us to the problem of freedom! Freedom, yes! Insofar as the interest of the national community gives the individual freedom, it is given! Where the freedom affects or even impairs the interests of the national community, the freedom of the individual ceases! Then the freedom of the national community takes the place of the freedom of the individual!…”
(1937)
And that also goes for Jeremy Vine and regular guests like Yasmin Alibhai Brown. What is funny about her is that she is so fast to call other people fascist. Yet she is one of the most vocal advocates for this collective nightmare.
“Here is a man who very nearly tasted the power that comes with running the world”
Surely this should say “the power that comes with ruining the world”.
Is this a concern for the planet or is the ageing scribbler becoming aware of his mortality and impending demise and will ride roughshod over everyone’s rights, no matter the horrendous damage, to try and ensure a little longer on this world? Selfishness and the gibbering terror of a threatened organism garbed in the finery of philanthropy is my take.
He literally said the quiet part out loud, and his mask fell right off, pun intended. When someone shows you who they really are, believe them.
Tyrants & authoritarians using the fallacy that they are saving you from harm if you just obey them were some of the most evil people that emerged during this whole covid madness. I was shocked as I watched ordinary people turn into cold hearted vicious fascists willing to destroy and even kill to fulfill their need for power and control. McNeil is just another one of these but with an outlet through his writing. He tasted this power and wants more.
Indeed, next time someone says, “You can either give up some of your rights temporarily, or give up all of your rights permanently”, RUN, it’s a trap! Or better yet, FIGHT!
I don’t want to be hater, but this guy…