The Daily Sceptic’s purpose is to question the conventional wisdom – something that’s more important than ever in the era of NPC-slogans like ‘Follow the Science’. But in this article, I’d like to uphold one piece of conventional wisdom: that vaccinating the elderly saved lives.
Now, this is far from a full-throated endorsement of the conventional wisdom on Covid vaccines. For instance, the conventional wisdom has it (or at least had it) that everyone needs to get vaccinated – regardless of age, physical health or prior Covid status. Yet there’s a decent case to be made against vaccination for young healthy people and/or those who’ve already had the virus.
Likewise, the conventional wisdom insists not only that everyone should get vaccinated, but that everyone must get vaccinated. Which is why until quite recently, you couldn’t get on an airplane without being vaccinated. I was strongly against the vaccine mandates, and my stance certainly hasn’t changed.
For those keeping score, I’ve always said the vaccines were a way of achieving focussed protection against Covid. And I continue to believe that vaccination was the right choice for most elderly people and others in high-risk groups.
At this point, a purveyor of the conventional wisdom might claim: there’s already overwhelming evidence of vaccine effectiveness against death, so what more needs to be said?
Yet as sceptics are well aware, there are problems with the evidence for vaccine effectiveness against death. Simply comparing Covid death rates among vaccinated and unvaccinated people, as purveyor of the conventional wisdom are fond of doing, isn’t satisfactory. (Note that the original RCTs were “not designed or powered to assess whether the vaccines prevented deaths”.)
First, there’s immortal time bias: because vaccinated people are often classified as ‘unvaccinated’ until two weeks after vaccination, deaths that occur during this window are not counted or wrongly assigned to the unvaccinated group, artificially inflating vaccine effectiveness.
Relatedly, there’s the ‘healthy vaccinee’ effect. Unvaccinated people are more likely to die of causes other than Covid, implying that they tend to be less healthy and/or less risk-averse than vaccinated people. Failing to account for this again leads to overestimation of vaccine effectiveness.
There’s also the phenomenon of waning. Some studies suggest that vaccine effectiveness against death wanes over time, just like vaccine effectiveness against infection. So even if the vaccines do protect against death, such protection may be relatively short-lived.
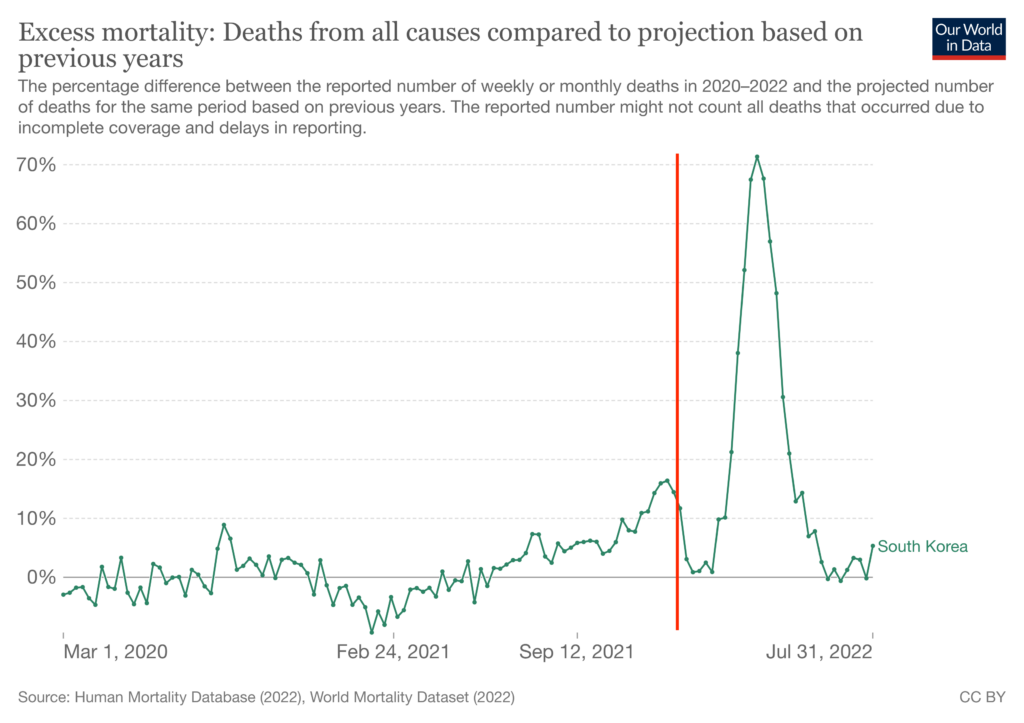
Finally, there’s the fact that some ‘Zero Covid’ countries like South Korea saw large spikes in excess mortality even after the vast majority of elderly people had been vaccinated. These data are hard to reconcile with commonly heard claims of 90% vaccine effectiveness against death.
One way to get round these problems is by using aggregate-level data: compare places where more elderly people got vaccinated to those where fewer did, and see whether excess mortality was lower. Any resulting correlation can’t be explained by immortal time bias or the ‘healthy vaccinee’ effect since those don’t apply at the aggregate-level.
And the use of excess mortality, rather than the official Covid death rate, obviates the problem of correctly classifying Covid deaths.
To see whether excess mortality was indeed lower in places where more elderly people got vaccinated, I obtained data on countries in the European Economic Area – the 27 EU member states, plus Norway, Iceland and Liechtenstein. These countries are culturally and economically similar, so the sample is appropriate for testing claims about vaccine effectiveness.
Data on the percentage of over 60s double-vaccinated by July of 2021 (the halfway point of that year) were taken from the European CDC. Data on life expectancy were taken from Our World in Data.
To calculate change in life expectancy, I subtracted average life expectancy in 2020 and 2021 from the average in 2015-2019. This indicates how much lower life expectancy was in the first two years of the pandemic than in the previous five.
You might say that 2020 should be excluded from the analysis as the vaccines only became available at the end of that year. However, the level of mortality in 2021 will be lower, all else being equal, for countries that had greater mortality in 2020. So it makes sense to take both years’ data into account. In any case, results are basically the same if 2020 is excluded.
The chart below plots change in life expectancy against elderly vaccination. The relationship is very strong and positive: in the most-vaccinated countries life expectancy stayed the same or even increased, whereas in the least-vaccinated countries (notably Bulgaria) it fell by 1–2 years.
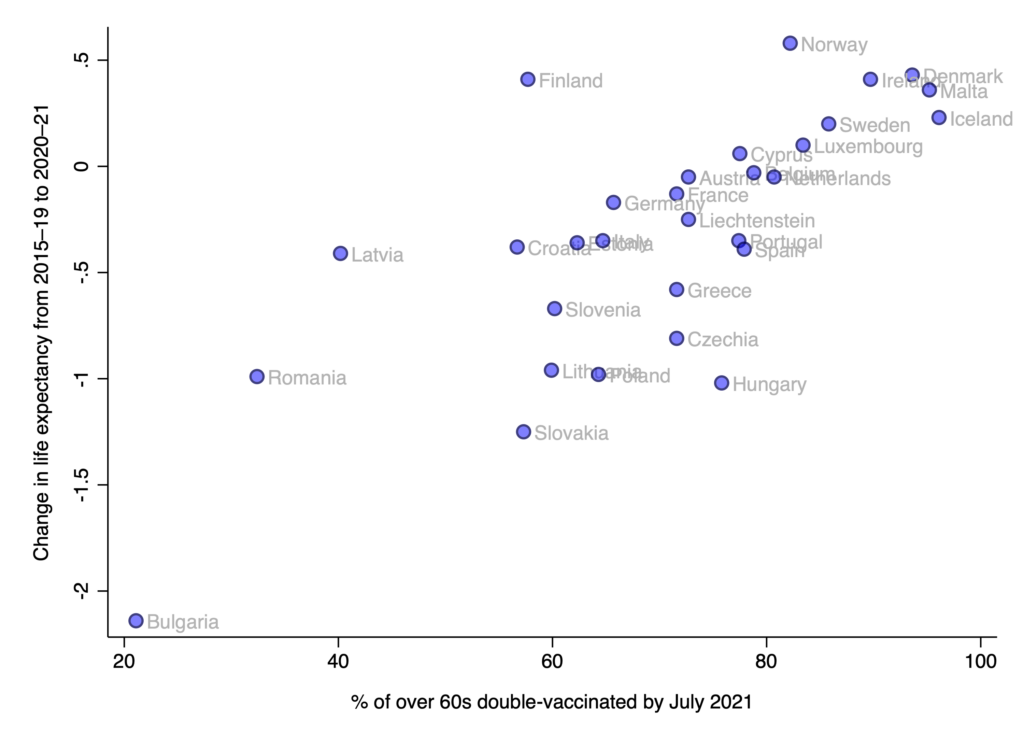
Of course, correlation doesn’t equal causation. Just because elderly vaccination is correlated with change in life expectancy, doesn’t mean the former caused the latter. So what other factors might explain the association?
Two obvious possibilities are: obesity and healthcare spending. Maybe it proved more deadly in places where more people were obese? Or maybe Covid proved more deadly in places where the healthcare system was worse at treating people?
When I tried controlling for these factors in a simple multivariate model, healthcare spending was more strongly associated with change in life expectancy than was elderly vaccination. On the other hand, obesity was not associated with change in life expectancy.
One could interpret these findings as showing that healthcare spending is the true causal variable, and elderly vaccination barely matters. However, I suspect that because the sample comprises only 30 countries, it is not possible to disentangle the effects of elderly vaccination and healthcare spending. (Perhaps some third factor causes both low elderly vaccination and less healthcare spending.)
To get a slightly larger sample, I turned to U.S. states – which provide another useful setting for testing claims about vaccine effectiveness.
Data on % of over 65s double-vaccinated by July 2021 were taken from the CDC, as were data on all-cause deaths among over 65s. To calculate excess mortality, I subtracted average deaths in 2020–21 from the average in 2015–2019, and then divided the answer by the average in 2015–2019 (and multiplied by 100).
The chart below plots excess mortality against elderly vaccination. As before, the relationship is very strong: in the most-vaccinated states excess mortality was less than 15%, whereas in the least-vaccinated states it was more than 20%.
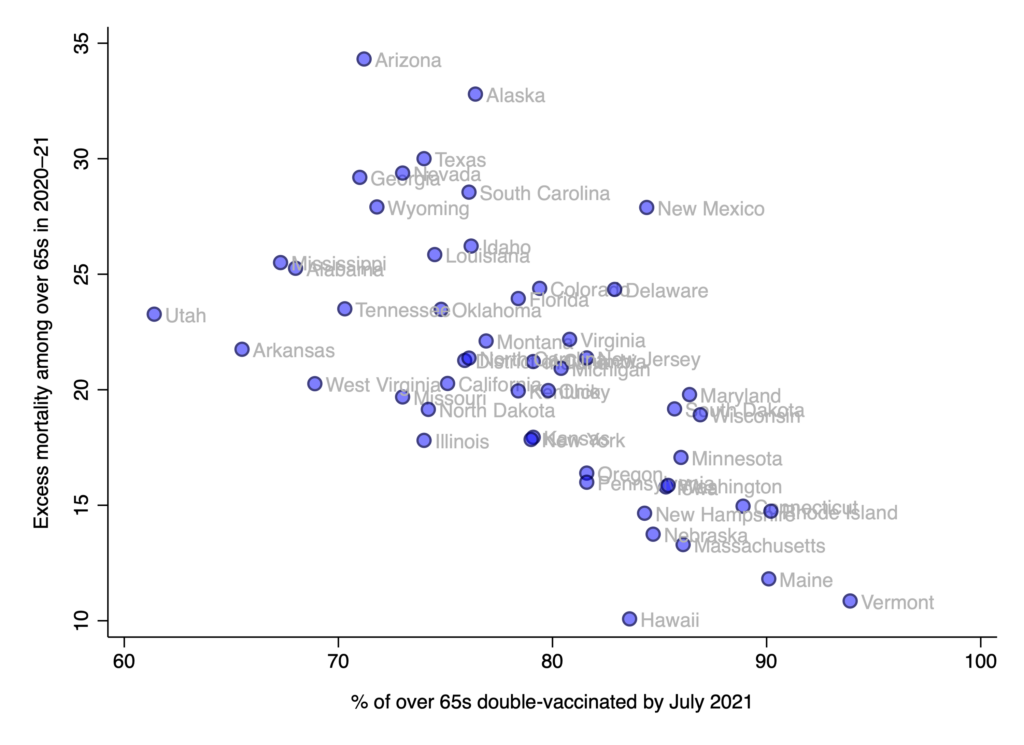
When I tried controlling for healthcare spending and obesity in a multivariate model, neither factor was strongly associated with excess mortality. By contrast, elderly vaccination was a consistently strong predictor.
In other words: in the larger US sample, the correlation between elderly vaccination and excess mortality can’t be explained by either obesity or healthcare spending. Perhaps there’s another variable that can explain the association, but it’s hard to imagine what it might be. (Neither age or racial demographics is going to work.)
As mentioned above, none of the results change substantially when excluding the 2020 mortality data. In fact, elderly vaccination is a more robust predictor in the European sample.
To sum up, elderly vaccination is strongly correlated with excess mortality in both Europe and America. The association is robust to controlling for obesity and healthcare spending in the American sample, though it diminishes substantially in the European sample. The latter result may be due to the small sample size, making it hard to disentangle the effects of correlated predictors.
One issue my analysis doesn’t really address is waning. Perhaps the vaccines don’t protect against death after the first year, so if I’d included the 2022 mortality data, I would have found no correlation or a much-reduced one? While life expectancy data isn’t yet available, there’s little evidence that the most-vaccinated European countries saw outsize excess mortality last year.
Iceland is the only one that saw a major spike in excess mortality (though in recent weeks excess mortality has been negative). So while comparisons based on only 2020–21 data may somewhat overstate the association between elderly vaccination and excess mortality, it’s unlikely to be dramatically different when including the 2022 data.
As another check, I obtained the ONS’s latest estimates of age-adjusted excess mortality, which encompass the period from January 2020 to July 2022. The chart below plots these estimates against elderly vaccination for 27 European countries. (They were not available for Germany, Ireland or Liechtenstein.)
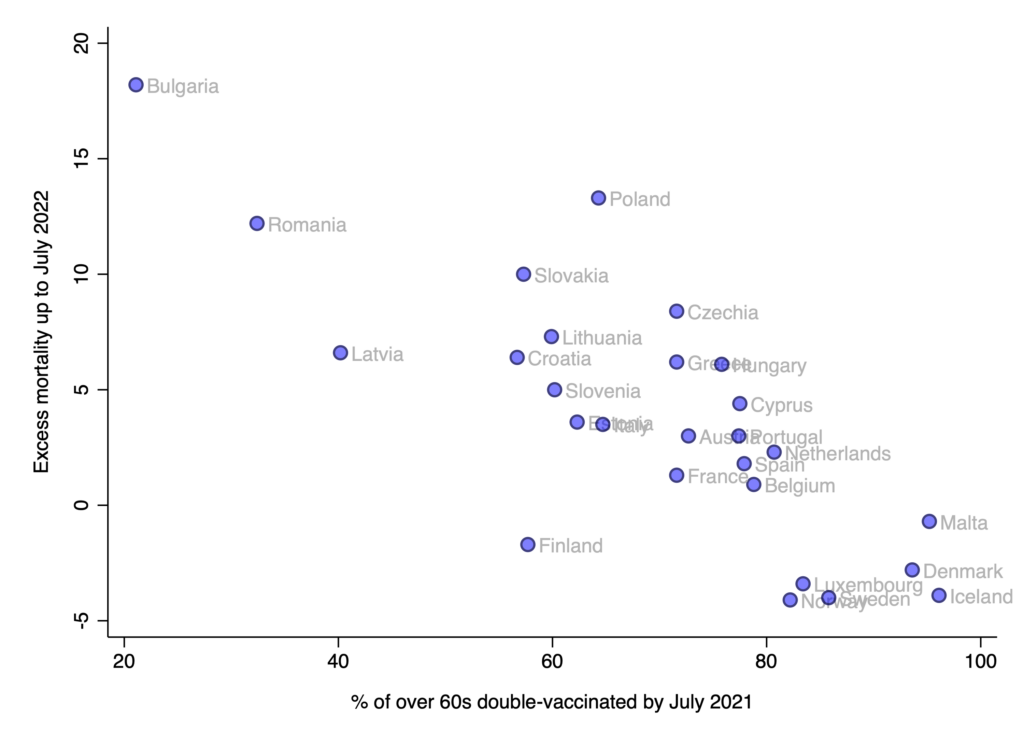
The relationship is just as strong as before, indicating that any effect of waning during the first half of 2022 was minimal.
In any case, even if vaccine effectiveness against death wanes all the way to zero after several years, getting vaccinated would still have been the right choice for most elderly people, since two or more years represents a non-trivial increase in one’s lifespan.
The evidence suggests that vaccinating the elderly saved lives. Unlike lockdowns and mask mandates – which had little discernible impact while imposing huge costs on society – elderly vaccination appears to have made a tangible difference. (There is no correlation between lockdowns and excess mortality across European countries or U.S. states.)
Focussed protection culminating in voluntary vaccination of high-risk groups was the right strategy all along – just as the Great Barrington authors argued.














To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
The next estate agent who meets Whitty in a London park, not a cuddle ok !!
Does Toby Young now regret not telling the world how evil Boris Johnson was while he had the chance?
Mother: I Put My Child’s School On Notice
https://www.youtube.com/watch?v=atBNDVwU32k
A mother at a freedom rally in Woking talks about how she warned her child’s school that they will face legal challenges should they coerce her child….
4th September, Woking, Surrey, England, UK
(The police were not wearing masks at the start before the filming started)
****
Upcoming events anti lockdown roadside events with the Big Yellow Boards to a Grand Stand in the Park
Wednesday 15th September 5.30pm Rebels on Roundabouts
Downshire Way, Bracknell RG12 7AA
near Premier Inn/Bracknell Fire Station
From our friends in Buckinghamshire:
Wednesday 15th September 6pm Marlow Hill, High Wycombe
Park up at Waitrose car-park
https://maps.app.goo.gl/VBLP9XXEFS3E9SK57
Saturday 18th September 12pm at Chequers meet up point as below
Coombe Hill Car Park
Lodge Hill, Aylesbury HP17 0UR
yellow boards with other banners and maybe a little protest outside BJ mansion
Monday 20th September 5pm Big Yellow Boards roadside event
Pavement outside (Morrisons The Peel Centre), Skimped Hill Ln, Bracknell RG12 1EN
Saturday 2nd October 2pm GRAND STAND IN THE PARK BERKSHIRE
– with a couple of guest speakers and a stroll thought the town centre at the end
Reading River Promenade
Reading RG4 8BX
Stand in the Park Reading River Promenade Reading
Sundays from 10am
Telegram https://t.me/standindparkreading
Stand in the Park Bracknell South Hill Park
Sundays from 10am
Wednesdays from 2pm
Make friends – keep sane
Telegram http://t.me/astandintheparkbracknell
isn’t there anything going on in Warwickshire or Oxfordshire
Check https://t.me/RebelsOnRoundabouts
I wonder!
What say, you Lockdown Sceptic?
T.me groups unite. Let’s Beat This Better Together.
Blake Park Bandstand Bridgwater Somerset –
Sundays from 10 am
Meet friends – keep sane – we are awake.
Telegram Connecting Warriors
Their hold based on an almost comatose compliance is slipping away and they know it .In discussions with colleagues i ask them, did you go to the football,the pub ,the cinema,the nihtclub,??? Yes they replied and
Are you ok i asked ,yes they replied ,Will you keep on doing it now you can ,yes they replied .Will you stop in an instant because the government have tried to tell you covid is many many many many more time serious than it actually is ,Not a fucking chance they replied .This will be the change .last year it was believable and served what we thought was the common good .A year later with almost everyone we ever knew still alive ,the risk is evident to all but a few bed wetters who were always afraid of sore throats anyway .Check your experience of Covid not the one you are being told to believe .Only the peple can end this .There are a million levels of compliance needed for this shit show to work .All most of have to do is shake your ow little part of the tree to make soemthing fall out of it.Soon it will become a barren trunk and forgitten about or at best ignored
We have to do our bit. But this could take years, if not decades, unless some LEADERS pop up and direct our wrath towards change. Too many people in power positions will cover up their mess or deny it altogether. There has to be a popular revolt or this is permanent.
Not sure leaders are going to help. It’s just projecting everything onto someone we hope will look after us but they invariably end up being corrupt and either useless or dangerous… And it all starts all over again… We need to start leading our own lives – somehow…
It will help. Some form of leadership is needed or we’re just a talking shop going round in circles, which is what they want. Why would our own lives on their own be any more effective? We have to trust in our ability to do more than moan.
In other words, the Govt applied the ‘precautionary principle’, but we’ve now seen through it, and it’s the evil it was predicted to be.
I really wish I could share your optimism – however much I might agree with every sentiment of it – but the brainwashing over a period of almost 19 months now, and which shows no sign of letting up, has just been FAR too effective and successful precisely because the sceptic angle never got a chance to be put to people in the early stages. Everyone I speak to around me is TERRIFIED of covid and believe that it shows no signs of letting up and are worrying about the death figures and the hospitals full of unvaccinated people with covid etc etc I do try, even very weakly (gently does it after all), to put the counterpoint, but if they knew what I really thought of it all (a massive scam on the whole UK population and I could present them with the evidence for that) they would recoil and never speak to me again. We cannot do it on our own in the face of a daily media bombardment of propaganda, and sadly, despite its best efforts, and I applaud them for it, GB news on its own isn’t going to achieve that either. We need a mainstream media outlet to start telling it like it is and we need a regular political presence to also do likewise – possibly Reform UK?
Better a huge wrestler to squeeze the life from the slimy, sniveling, wimpy, evil, excuse for a human being!
They lied.
What a surprise.
Protect the NHS. Never mind the people.
Always remember, lies may take care of the present but they have no future.
If i may… Protect the *massive money making/laundering scheme that keeps us and our friends significantly richer than you*
a Health operation with a country tied to it. Why don’t we just get rid if the farscilce name the United Kingdom and just rechristen it to the NHS .
I live in the NHS I am a citizen of the NHS.
The NHS is a killing machine and at some point soon it will undoubtedly need protection.
That good ! because we have load of practice at protecting it
Not just lies. This is demonic. This is the biggie.
Unfair to demons, sez I.
and what will the people get for protecting the NHS.They are sensing a distinct lack or reward for their efforts
they’ll get no access to medical treatment, unless of course they have severe covid, and will be left desperately googling their symptoms and perhaps needlessly dying due to lack of access to testing and treatment….
And lied and lied ..and lied; and then they caused their “Precioussssss” NHS to be slaughtered by not mandating early treatments to prevent NHS overload whilst sending legions back to Care Homes w/out any treatment – Hancock guilty as charged – inadequate PPP; Result – people ill with virus had no prophylactic treatments – as in US and elsewhere – affected people get sicker and last resort treatment is in the very setting these truly evil politicians say they want to protect.
More clear than ever that Whitty/Vallance etc are as guilty as Johnson & Co – the are not intellectually thick but they are the personification of the worst kind of appeasers last seen in the 1930’s – and how many millions of people died in WWII as a result?
QUOTE:- I live in the NHS I am a citizen of the NHS.
This reminds me of a conversation I had with a late friend about 7 Years ago. He was then in his 80’s and having felt it advisable to have a check up at his GP practice where he was subjected to a process that implied that the NHS actually owned his body! His words to me were “They’re coming to get us, watch out! ” How true those words turned out to be.
My feeling is that the NHS has past its day and is THE PROBLEM. The NHS should be reformulated as a free National Emergency Service. The other functions like elective surgery and non critical interventions should be “Pay as you Can” – OK, Means Tested. Before you jump on me for mentioning Means Testing may I make the point that at present we are expected to pay up to out total estate to reside in a care facility for our final years, so why not pay some of our wealth to improve our well being while we can still enjoy some freedoms? After all what’s more important – your wellbeing or a 30K SUV parked in the driveway?
An advantage of such a personally funded system may be the decoupling of Big Pharma from a State Behemoth, having to sell on a more individual basis may force them to reconsider there price structures? Bureaucrats just pay up whereas I / We think / research it.
Considering they are directly manipulating the numbers through policies, and the fact that there doesn’t seem to be any discernible difference between covid and the flu, sounds to me like they will try and to all they can to convince the public that we need vaccine passports.
Correct – the latest ZOE symptom checker suggests the current “variant of covid” is all but indistinguishable from the Virus Previously Known as The Common Cold.
It’s an absolute travesty that MPs just roll over and accept this nonsense trotted out by ministers and their supposed experts.
No doubt they have some incredibly accurate modelling to back up their policies though.
You are the first person who has not shied away for saying that Covid is similar to flu .In th begining there was absolute outrage for suggesting such a thing even though there was no such thing as a covidometer to measure the difference .As it turned out it was very much like the flu and very much like the flu i have just shaken off .I was tested for covid twice ,i ll say they tried damn hard to pin it on me but no, it was flu .Apparently this bug has been around forever and didnt simply just disapper from the earth last year .My own thoughst were that this viscious fucker of a flu bug is in fact worse that covid and given that, they could suddenly give it the attention it has sorely yearned for these last 50,000 years aand make us all stay in now that this isnt just flu (said in M&S sexy food ad voice)this is multi variant triple fatal inter stellar flu so you all better stay in again .For fucks sake in the words of that awful Grange Hill song JUST SAY NO
It ain’t quite the flu, because it is man made, or man adapted, at the expense of US tax payers, to have some especially vicious qualities. Dr Kendrick says deaths he has seen form Covid are unlike any he has seen before. I’m sure he is right.
But for most it’s flu or much less of course.
One person I do trust, Malcolm Kendrick.
Me too. He doesn’t go way beyond the data.
It is true that blood disorders appear much more common with “covid19” than with influenza. That’s thought to be wholly down to the superficial spike protein.
in terms of infection fatality ratio, I think it’s fair to say that the original SARS-CoV-2 WAS worse than a typical seasonal flu.
But as we’ve seen before, the slow mutational drift in SARS-CoV-2 favours its survival, which implies greater transmissibility yet REDUCED lethality.
The most recent estimates of IFR of the delta variant is pretty much superimposed in the flu IFR at around 0.1%.
As with flu, the VAST majority of those unfortunate enough to die as a result of infection by flu are elderly & already chronically ill.
The MAJOR positive which can be laid against SARS-CoV-2 is that it does NOT harm let alone kill children.
People seem to have forgotten (if they ever knew it) that flu, while also heavily biased to lethality in those close to the ends of their lives, does injure & kill a small but tragically distinct number of previously healthy YOUNG people.
i recall last year looking at causes of death by age band & being shocked at how many school aged children perish weekly in the winter of “ILI” (influenza-like illness).
I can’t believe how many people still seem to have complete confidence in Govt & their advisors.
Could that be because the chimerically made “virus” has been GoF modified to include a spike protein – that induces the inflammation that ultimately kills – never seen before – isn’t that what Dr K is driving at – a genetically modified SARS variant – deliberately so made and made possible by US tax dollar funded “research” contracted out to China.The crime of any century.
Beautifully expressed!
The NHS is under threat and overburdened every previous winter before Covid due to years of underfunding.
It’s nothing to do with under funding. It is inefficiency and bad management.
It has everything to do with underfunding AND inefficiency and bad management.
Underfunding my arse; out is too big, run by inadequate and incapable people, top heavy with administration empires. Any career military person would sort it out in under two years if the politicos were brave enough to pull the trigger. TOH works in the NHS and I have heard daily tales of ridiculous so called management for many many many years.
In October 2019 before the last general election a political commentator asked voters to speak to someone who works in the NHS and ask them these following questions which all have links proving the facts ……
Ask them how they think the £20 billion in NHS cuts between 2010 and 2015 affected the quality of care the NHS could offer, and how another £22 billion in NHS cuts is affecting the quality of care the NHS can offer now.
Ask them how they feel about the way the Tories introduced new rules to make it much easier for them to force the closure of NHS services without taking the views of local people or staff into consideration.
Ask them whether waiting list times and record waiting times at A&E departments have been rising, and whether they agree with the Tory policy of simply scrapping any waiting list targets that are being missed and scrapping the four hour A&E target instead of actually doing anything to address the dreadful problems they’ve created.
Ask them whether they think Theresa May’s decision to scrap NHS bursaries had anything to do with the 31% decline in applications for nursing courses, and the shortfall of an astounding 70,000 nurses in the NHS, and whether they think the NHS recruitment crisis will get even worse as the supply of new nurses slumps dramatically as fewer and fewer new nurses enter the system.
Ask them about NHS privatisation and how ever more NHS services being carved up and given away to profiteering private sector health companies like Serco, Virgin Health and (the major Tory party donors) Circle, reaching an all-time record of £9.2 billion worth of NHS privatisation in 2018.
Ask them how they feel about the years of below inflation pay rises for NHS staff whilst MPs bagged a whopping great 10% pay rise for themselves.
Ask them how they feel about the Tories’ £4.6 billion cut in the social care budget, and what kind of effect that is having on the already overstretched hospitals that are having to pick up the pieces.
Ask them whether the junior doctors were treated fairly and with respect during their confrontation with then-Health Secretary Jeremy Hunt.
Ask them whether Jeremy Hunt’s comments that people should just Google their health symptoms instead of seeking medical advice was a risk to public health.
Ask them whether they share Theresa May’s view that Jeremy Hunt was “an excellent health secretary”.
Ask them if they actually know anyone working in the NHS who has confidence in the pompous liar that Boris Johnson has put in charge now (Matt Hancock).
Ask them about the £3 billion wasted on the massive 2012 top down reorganisation of the NHS that the Tories repeatedly promised not to do before they sneaked back into power in 2010.
Ask them how they feel about the scores of A&E units, maternity wards, mental health facilities and NHS walk in centres that have been shut down by the Tories since 2010, and whether these closures have markedly increased demand elsewhere in the NHS.
Ask them about the secret plans the Tories drew up to close even more A&E units, maternity wards and walk in centres.
Ask them if their own primary care trust is in deficit.
Ask them how they feel about the Tories going on about how much they care about mental health issues as they simultaneously slash the mental health budget and instruct their outsourcing contractors to specifically discriminate against people with mental health conditions.
Ask them if they know any EU citizens who work in the NHS and whether they have left, or are thinking of leaving because of the threat of a ruinous Tory hard Brexit.
Ask them whether the 92% decline in the number of NHS nurses arriving from EU countries is likely to exacerbate the NHS recruitment crisis.
Ask them how they feel about the Chairman of Conservative Health saying that the only way the Tories could bring in charging for NHS services is if there was a feeling in the country that the NHS is “falling apart”. and whether the ongoing crisis in the NHS might actually be part of a deliberate Tory strategy to bring the days of universal health care to an end.
Ask them whether they feel that their colleagues are ever more stressed and overworked as they try to cope with increasing demand for services while funding and staffing levels are slashed year after year.
Ask them whether they think the NHS can actually survive if the Tories carry on like this.
https://anotherangryvoice.blogspot.com/2019/10/why-you-need-to-speak-to-someone-who.html
Impressive list, and before covid of course.
You could run for politics.
Unfortunately, it no longer matters. Such is the distortion of priorities “because COVID” that it would take a lot more than money ever to restore its reputation as a caring & competent institution.
its my ambition never again to see the inside of an NHS hospital. I don’t bother with my GP either.
Well Googled. I do not disagree but I don’t see any reference to the Blair governments privatisation of the NHS; I do not see any reference to the wholesale scam of PFI – sure started by the Tories – but ramped into interstellar overdrive by….Blair and Brown. If you are “happy” to fund the PFI contracts too expensive to be bought out and requiring annual debt finding even of they no longer provide “services”, please confirm.
I don’t see any shade of political opinion having a good handle on this – I am no Tory supporter either – they have both been a disaster for not dismantling it and starting again. Throwing more money at this money-pit is never going to work as I suspect you know.
The NHS has been falling apart at the seams for decades; too many services, too few competent managers, management refusing to demand – as they are legally obliged to do – payment by health tourists for their services. In case you are not aware, in times gone by, certain Labour Councils in the UK have backed some NHS Trusts not assiduously chasing this cash. In case you are not aware, some NHS trusts in certain parts of this country are inundated with people from abroad brazenly lying to get treatment here…for free. If you support that please confirm. And just in case you try to use EU Health systems where UK citizens routinely got treated whilst abroad as some kind of example how to run a health service – I had to pay towards my care in incident 1 and on another occasion, different country, the only care provider refused to treat under EHIC convention – why? because UK NHS/DWP admin took a very long time to pay up – get the drift?
Who opened the door to clinician immigration?
I can add other “eg’s” – how about nurse training – now you need a degree and are so well qualified that as soon as you get on the ward to do “Nursing” it is not unknown for Regs/SR/Cons level clinicians to have to do what was done formerly by …nurses because they did little actual nursing training. Midwives similar.
Not all Tory or Labour cockups, but they have ducked this for far far too long – well the time is coming very fast when it cannot be ducked any longer. No one will dissuade me me that Johnson and Co have screwed up so badly with SARS COV 2 that they have massacred the NHS – my experience is not yours nor RickH. Bur I think we can agree it is not fit for purpose anymore.
Medics and clinicians who do the hard yards are not – generally – included in the above description by my experience to date.
I am no fan of Blair and he did bring in the dreaded PFI’s.
However, New Labour (which I am also not a fan of) to their credit actually increased the funding of the NHS until the Tories came in again to dismantle it.
Health tourism is always going to be a problem until measures are taken for full reimbursement.
Nurses requiring a degree was a Labour decision implemented by the Tories.
Medical professionals and health staff in general are normally overworked and underpaid which is in part due to underfunding.
My wife of 38 years has been nursing for 45 years and is still a nurse and has seen the devastation caused by governments and the overblown hype around Covid which is nowhere near as bad as the powers that be are telling us. We also both have doubts about vaccinations.
I am disappointed that medics within the NHS have not been more vocal in their scepticism and of the treatment given to Covid patients. Most are brainwashed and those that aren’t are scared of being sacked.
Extra funding, less managers and patients paying for some treatments to weed out the hypochondriacs and time wasters would be a start.
outThe National Hurt Service is doing everything the publicly funded, Rothschild Medical Complex wants to extremely well.
bad management and swathes of it
Brother worked at a dental hospital 20 yrs ago and left because he couldn’t stand seeing the layers and layers of pigs at the trough
The Uk spends as much on health, private and NHS as Germany and France. If we spent more on private and less on the NHS our health care would be immeasurably better.
“Funding for healthcare is lower in the UK compared to many other high-income countries, at 10.3 per cent of GDP compared to 11.2 per cent in France, and 11.7 per cent in Germany.
In the UK we have three doctors for every 1,000 people, compared to three in France and four in Germany. We have seven nurses for every 1,000 people, in comparison to Germany’s 13 and Frances’s 10. In terms of hospital beds, we have two per 1,000 people compared to five in France and eight in Germany. We also have fewer diagnostic tools such as MRI and CT scanners.
As a result, in combination with poor welfare spending generally, the health of the UK lags behind that of many other wealthy nations and inequalities persist in key areas including life expectancy, cancer survival, and cardiovascular disease.”
https://www.independent.co.uk/voices/nhs-reform-covid-funding-b1843785.html
You are only talking about the NHS. The total health spend in the UK private and NHS is the same per capita as France and Germany. And there is literally no point in referencing the Independent, I wouldn’t use it to clear up my dogs’ sick.
i would
Show a link to prove your suggestion.
The article I linked to is from Dr Michael Anderson who is co-research lead for the LSE-Lancet Commission and Elias Mossialos who is professor of Health Policy at LSE and the co-chair of the Lancet Commission.
Who cares that you don’t like the Independent.
HAHAHAHAHAHA – the Lancet – is that the same organ that published the letter from a group of scientists who were lined up by Daszak/Farrar/Fauci & co and attempted to trash the theory that SARS COV 2 leaked form the WIV? Is that the same group of scientists 27 of whom have been skewered for their links to ….the WIV? What is the thrust of the US Intelligence Services now ( and they DO know because they are implicated in the GoF “Research”)
Saying the NHS is “underfunded” is straight out of the “Meaningless Mantras For Dummies” playbook and the exact same kind of rubbish as Johnson et al saying they are protecting the NHS ( after damn near destroying it in 2021/21 and, in all but name, broken the will and spirit hordes of NHS clinicians such that they are retiring/leaving in very significant numbers thus putting even more strain on a broken system ).
Try again.
Give it some more money to waste so they finally privatise the bastard child of post war socialism and we can stop praying to it like some some fucking shaky sun god
Poor welfare spending? Is this a wind up? Show me anyone other than the homeless who doesn’t have a smart phone or flat screen TV.
Underfunding? It’s a black hole that just sucks more and more resources out of us all- it needs running efficiently if that’s even possible any more. The more money it gets, the more it will demand and use, just like anything.
Stop being an apologist for the Tory party who have underfunded the NHS and the Old Age Pension so that the UK is behind most other developed nations.
It’s the Tories fault that the NHS is inefficient, they’re the one’s who control it.
Another belly laugh, thanks; the State Pension is, never has been and never ever will be “funded”.
Politicians of all disaster parties have created a crutch for people instead of encouraging “self reliance” – ergo, it becomes a “drug” and the people are addicts. Weaning them onto taking personal responsibility for their health through diet/exercise etc might leave the “NHS” to treat the unforeseen illnesses life throws up. The ever expanding suite of treatments was never envisaged in 1946, and C. Northcote Parkinson was right about the inevitability of an entity ever expanding, this time to create a demand that can never be paid for – long overdue massive reorganisation needed along European public/private ( “mutuel” if you like ) lines.
Yes that’s right – European health care systems are public private partnerships serving 500m people and are – in my twice times personal experience – better equipped, better staffed but still I had to pay for elements of my treatment only partially recouped. If it works over the channel it will work here – and it will be less of a political football than it is now to no one’s interest.
Anyone seen the one way roadmap?
It got “accidentally” chucked out with the recycling…
Deaths (Covid) are 10 times higher this August than last August. Ergo, this winter is going to be horrendous. The double vaccinated will be monstered by Antibody Dependent Enhancement (they already are, hence 10 times the death rate) and many other vaccinated people will be hit by blood clot problems – up to and including death. On top of these horrors we have an NHS operating well below capacity due to staff suffering from adverse vaccine side effects coupled with the resignations of thousands who refuse the vaccine.
We are therefore guaranteed an absolute tsunami sized overwhelming of the NHS, which effectively means a guaranteed lockdown, guaranteed V-passports and guaranteed war against the untermenschen unvaxxed as we will be held responsible for the government manufactured catastrophes. Just as the New World Order planned…..
I can’t ‘like’ your very accurate post of the dystopia in which we live.
Thank you for so eloquently describing it.
“Deaths (Covid) are 10 times higher this August than last August.”
There will, undoubtedly, be fictions like this perpetrated … which would replace other causes of mortality to an absurd extent in a year when the actual August all-cause variance is +1 to +2% – i.e quite normal (but giving no confidence in vaccine efficacy).
The current excess death for those aged 45-65 years is about 5 standard deviations above normal for August. Most ages see a similar level of excess death, other than those under 16.
However, deaths from covid account for about 1 standard deviation of these. There is something else increasing the death rate in the country at the moment.
Yes, I think we all know what two things are doing that…
Quite.
And, with the above factored in, what is the appropriate countermeasure?
Wait until the elite dies from vaccines, then start over.
They ain’t taking ’em!
Ha! Never saw meself as an “eelit”!
but they’ve all had photos of them with their sleeves rolled up or shirts off completely having the jab shoved into their arm with brave look on face and then tweeting afterwards that they didn’t feel a thing….oh, you mean the saline/placebo jab
Don’t forget the booster deaths.
they’re hiding the stats on vaccinated being hospitalized
From Mercola’s daily bulletin
If CDC are doing it – uk prob doing the same
Even a CT rate of 25 is too high according to Dr Fleming if I recall – “efficacy” of the PCR flatlines at 25 according to a video he posted…?
The boosters which they are about to shove into the arms of everyone over 50 will guarantee it – I don’t expect my mother to be alive by this Christmas based on the effect the first 2 jabs have had on her.
The vaccines are working well aren’t they? (Sarc).
Precisely the main point. They told us vaccinating the most at risk was the way out of the pandemic, not into a new or worse version of it which this winter will be. But then Zahawi knew vaccinating would cause variants to emerge and they would rake it in creating new vaccines. So much for The Science.
Except the “booster” ain’t created against the new variant. It’s just more of the same pharma ejaculate.
It’s absolutely inevitable vaccine freedom licences will be brought in.
The “pandemic” will never be allowed to go away (just as flu hasn’t) so the freedom licences will be with us permanently to stave off a threat which everyone has long since forgotten is most deadly to very old and already at risk people just as most respiratory viruses always have been.
True. But we’ve all foreseen and accepted this. We will fight until we win or are destroyed.
Complete pantomime. We are governed by these clowns? It is becoming almost embarrassing.
As to the NHS being underfunded, if there are around 1.4 million employees, that means something like 1 in 46 of the population work for it. So 20 for every thousand, roughly speaking. Underfunding is not the problem. If anything it is vastly over resourced, and still the organisation makes a f@%king pigs ear of everything it touches. It is a vehicle for management careers, not for treating sick people.
And to add insult to injury can’t any of these charlatans see the graphs going skywards following the jabfests?
The NHS is under-funded by any relevant comparison. Whether it could improve efficiency is another matter, but a major reason for the shit-show and the ‘Protect the NHS’ nonsense is a political drive to divert attention from a trail of political mistakes in the resourcing of the NHS leading to a shortage of provision.
But if anyone thinks private provision provides any model of efficiency and economy, they really need to get out more.
Sorry – but a downvote with no argument is just proof of having no argument.
I’ve just had an example a prime example of private sector inefficiency – a 20 minute consultation costing £300 for someone desperately needing a diagnosis, and thus forced into the private sector (a hidden government policy, in effect), where the consultant hadn’t even got his head round the notes. I’ve never had that degree of sloppiness in several years of frequent NHS treatment.
I could write a book on how badly the NHS has treated me on multiple occasions, nothing life threatening yet, but a life of misery and pain going on 3 decades worth now. Absolute shit show, little to no interest in prevention or lifestyle cures, ‘just take this pill and go away’.
… and I could document 8 years of the precise opposite, dealing with life threatening issues. That’s the problem with individual stories.
What I do know is that the Covid shit-show has little to do with the NHS per se, and all to do with political control. The US with a very different system has had similar problems.
Same in Germany, again with a different system. Same Health system could be overwhelmed! We must urgently buy Chinese face masks! method.
Yeah, perhaps if the health minister had not spent 7 billions on Chinese facemasks, but rather used the money to hire new ICU staff, the health system would have been a bit less “overwhelmed”. But as he told in an interview, the only regret is that he did not waste more money.
Von denen kriegt er keine Prozente :->.
just think what the £37billion on track and trace could have done for NHS and ending the pandemic since pandemic is only over when bedwetting NHS says it can cope – so, never then
The NHS issuing held up as all important but it is the excuse for extremely bad decision making by politicians who have surrounded themselves with agenda driven apparatchiks – SAGE/NERVTAG/modellers and pysop mechanics – whilst refusing to seek truly independent scientific advice based on experience in dealing with epidemic management/vaccines etc – as evidently happened in Sweden and elsewhere.
For reasons I cannot disclose I could fill these pages with incidents of “NHS” malpractice going back decades – it is crippling parts of the NHS unseen by TGBP because “no fault” compensation does not exist.
FWIT, my life has been saved more than once – UK and elsewhere – so my comments are not a moan for moaning’s sake.
I don’t particularly agree re the NHS- it’s been appalling in so many cases within my family but brilliant with my wife’s cancer- BUT I do feel we all get side-tracked, probably deliberately, into this debate when the real issue is the relentless assault on our liberties. Nothing justifies this. Absolutely nothing.
All that is about to change with introduction of Whole Genomic Sequencing – if you think things are bad now they are about to get a whole lot more dystopian. Government has already done a 2 month consultation on it and is determined to introduce it because it will make massive cost NHS cost savings.
I worked in the NHS for over 22 years and I can tell you that it is not underfunded but extremely badly managed.
I concur. Too many managers, insufficient clinical support admins to allow clinicians to do clinical work & layer upon layer of hoops to jump through. I’ve worked in the NHS for 33 years. When I first started a dozen paediatric patients were seen each day in clinic & all notes & admin completed in what was then for me a 33hour week. Six adult outpatients seen in clinic again with admin done & six home visits done per day. Now patients only want to be seen at certain times, don’t like early appointments & with the associated admin hoops to jump through with no clinical admin support, guess what? Number of patients able to be seen in a day for adults is four! Now full time work a 37 hour week yet regularly do 9 hour days just to deal with all the admin!
My bag is rehab, with the take a pill & get better approach over the years, the concept of having to work hard to get better doesn’t go down very well…
TOH’s experience over the same time period, to a “T”
1 in 20 of the working population.
I wouldn’t want to put myself through watching the whole of that press conference, but a quick fast forward and you can see Whitty is his usual doom-y self, and the questions from the people seated who claim to be journalists were all, as ever, Why can’t we have harsher restrictions? / Why aren’t masks compulsory? / When can we have another Lockdown?
As Julia HB puts it “So, to summarise the Winter Plan:
Plan A: vaccines & learning to live with this endemic virus.
Plan B: go back and repeat the exact same policies based on no scientific evidence that didn’t work last time and which won’t work next time either.”
Plan A: stream of embezzled money and bribes might dry up.
Plan B: we just continue to milk everyone as usual while they keep clapping in appreciation.
Guess which plan is going to win.
The real Winter Plan!
we will be locked down by end November at very latest
Not me.
Javed says – that at 81% – the jabbing programme has been highly successful. Then announces a programme of interventions that they will use – ‘if necessary’ – without stating what criteria would constitute ’necessary’.
Why can’t they be precise? Why leave everyone in limbo? What does such uncertainty do for business – big and small – for education and for peoples’ state of mind.
Weren’t we promised that getting jabbed would lead to a return to normal?
If harsh regulation may be necessary, what was the point of getting jabbed?
Why sow fear into the minds of people?
Incompetence or wickedness?
Jabbing program , you’ll note. Nothing about their efficacy.
threats, threats , threats. “if you don’t do this we will mask you, if you don’t get your children injected we will lock you up, if the god we all serve the NHS starts to struggle again we will shut your business down”
What a country! ruled by despots, by thugs dressed up as scientists as politicians who are so drunk on power they will sacrifice us all and anything to keep hold. Haven’t we all had enough?
I somehow don’t think Bozo wants another lockdown. Not because he doesn’t enjoy kicking peop,e in the face, but because he thinks that this time, they,
or some of them, are likely to fight back.
Yes, that’s a possibility. Him not wanting one because he thinks they will be unpopular is how he feels, he doesn’t think.
Tory constituents complaining.
We had enough months ago. We’re currently waiting for leaders and some fireworks.
So unless we impose lockdown/vaxxing on ourselves Boris will throw the kitchen sink at us.
He’ll do it anyways, whatever we do, so at least let’s not CHOOSE to do it.
A lot of rage against the corrupt politicians and members of SAGE – yet they will just continue to receive their salaries and live happily ever after on very comfortable pensions. Much huffing and puffing but the house of cards still stands.
Professor Whitty gave a more downbeat assessment saying that infections were “high” relative to last year, and the NHS was under “extreme pressure” because the vaccines were helping to boost hospitalisations
Fixed it!
Same lies regurgitated. God how I loathe these bastards.
This country is well and truly fuc*ed. Johnson has allowed the ridiculous deification of the NHS to reach its apotheosis. We have become a poorly run health service with a state attached to it.
You would think that the last 18 months might have made the scales fall from people’s eyes. But no. Even the tax grab (none of the money will ever see social care) doesn’t prompt calls for reform of the antediluvian relic.
Psychiatrist’s talk about ‘learned helplessness’ where no matter what you do, the end resulti s deleterious.
I’m there. I give up.
Are they deliberately ignoring the blatant correlation?
The emperor has no clothes!
Not my Emperor!
We need a true Bonaparte to do some spring cleaning
It would be fascinating to see a journalist put the underlying question :
“So, Prime Minister, this would suggest that the ‘vaccines’ are an utter failure, doesn’t it? Why are you still pursing a failed policy?”
Any bets?
They spout the “Saved over 100,000 lives” sound bite. A figure completely bereft of any evidence, but easily swallowed by the gullible.
One question wouldn’t be enough. You’d need an extended period with him on his own, following up every bullshit answer of his with logical rebuttals. I think it would be an utter trainwreck for him, done by the right journalist who remained calm but firm.
But all journos are in on IT, so editors would absolve the creep. The only extended questioning he needs is in a court room. With swift and final resolution to the questions preferred.
Ha- I wish the stock market was as easy to predict.
I can safely say without fear of contradiction that stock markets fall as well as plummet
But there are no contradictions, so Johnson needs to check his premises- assuming he knows what they are.
There is going to be a surge in “infections” when they jab the children because the Pfizer jab depresses the immune system. The booster will wipe any natural immunity the double jabbed have developed, since their immune systems were wiped by the first two jabs. There will need to be a second jab for teenagers and another booster in the spring for the sheeple. And thereafter for everyone for evermore to try and stop the ADE.
Nice doublespeak. The vaccines are working but the NHS is still under “extreme pressure.” Would that be because of your total mismanagement of this whole pandemic? Your sole focus on all things covid has led to major backlogs in other areas hence your “extreme pressure” you witless idiot.
Once again one wonders why Labour continue to pass up the opportunity to defeat the government by opposing all this. The opposition plus Tory rebels = government defeated.
Because, unfortunately, in the US (due to the timing of the election and the fact that Biden had to say the opposite to Trump) lockdown policy and its bastard siblings have become very much a left-wing bandwagon.The left in other English-speaking countries have all jumped aboard, so Labour is only ever going to demand even tougher restrictions.
Because they support it.
The NHS could potentially be overloaded with all the vaccine injuries and not necessarily just Covid.
In August 2021 a pro-vaccine pathologist in Germany who has been vaccinated against Covid himself did 40 autopsies on people who had died within 14 days of the vaccine and found that 30% to 40% died from the vaccine.
Google translate into English. https://www.augsburger-allgemeine.de/panorama/Corona-Chef-Pathologe-der-Uni-Heidelberg-draengt-auf-mehr-Obduktionen-von-Geimpften-id60235361.html
Come on guys, we’d better get vaccinated now. We have to keep our communities safe, and it’s a moral duty to obey the government, which is doing really well to stop this vicious virus in so many, many, ways. The vaccines are EFFECTIVE, SAFE, QUICK, and FUN. It’s not true they’re not working: they’re doing what they’ve been created for. It’s working!!! Everything going great!!!
yes the bit about yesterday that worried me the most was the determination to double down on their efforts to get the remaining 80% who are still unvaccinated double jabbed – how do they intend to do that? will they be sending the police to homes? rounding them up and interning them in camps? if you’d wanted it you’d have had it by now and there isn’t much more left in the psychological coercion arsenal
Boosters are an admission that the vaccines don’t prevent anything. And if the boosters don’t work what would be the point of vaccine passports?
True. It’s all f*cked up. We have to get some leaders and put on some fireworks.
The point of Nazipapiere is that Nazis love them.
20th March 2020: the clown announced the first lockdown to “protect the NHS“.
We are 6 days off 18 months from then: the clown suggests we may need further lockdowns to “protect the NHS“.
With apologies to the Blackadder team:
Pathetic!
The asthmatic ant needs his booster
Thank you – you made me laugh!
Witty is grasping for straws. How about some real news? Schools reopened. Once again, the predicted COVID tsunami didn’t materialize. Massively ramping up testing didn’t kickstart the pandemic again, just a short flare-up of hitherto undetected asymptomatic infections.
Infections have been declining fairly sharply for six days in a row now.The government’s chief Corona whisperer tries to paint this as bleakly as possible while all the usual experts update the date of the predicted apocalypse once again.
Instead of consulting a broad range of views, the gov are allowing a turtlish man to project his psyche onto the “virus situation”. What a wise man.
… but we know that this has nothing to do with reality.
Just love the cartoon.
Now a real leader would have long since got rid of those two jokers along with putting Ferguson out to grass and cutting all research funding to Imperial College. Unfortunately, we have Bunter
None of this is surprising, it is entirely consistent of Kim Jong Johnson to say and do exactly opposite things in a very short space of time.
Despite there being no justification for lockdown, even without the vaccines, he is proposing them anyway after they’ve been administered.
He’s also going to bring back the same old pish that previously had no scientific justification anyway because he can.
The UK this winter following its miopic belief in the failed vaccines:
“Seriously ill COVID-19 patients double in vaccine pace-setter Singapore”
https://www.reuters.com/world/asia-pacific/seriously-ill-covid-19-patients-double-vaccine-pace-setter-singapore-2021-09-13/
‘Infections’ ie faulty and inaccurate PCR and LFT results? This is War. Updated information, resources and links – PS RogeredBorg – this is a link – (Love, love, love Bob Moran – many thanks for the permission to use the artwork! ‘Stand Firm’): https://www.LCAHub.org/
That’s what you get when the sunk cost fallacy meets a God complex, as always with cults.
Which is why they can never change their opinion, to the contrary even in particular in light of any contradictory evidence, and why they can and will only end in and through a catastrophe.
As the NHS is always overwhelmed for +/- 9 months of the year, as they openly manipulate all Covid data and criteria and as they have a completely different real agenda, we here all understand what that means and will result in.
Many people seem to be upset and willing to balk at the boosters, but as they mostly also didn’t bat an eyelid when their children were poisoned, I wouldn’t hold my breath that they won’t cave in.
Regardless, and especially if they don’t and opposition increases, the only proper way forward and to deal with any new restrictions is mass civil disobedience.
The German singer Nena nailed it:
“It’s not about what we are allowed to do. It’s about what we let them do with us.”
Perhaps instead of ‘Clap the NHS’ every night, we need ‘Boo the government’ every night?
Despite the depressing news, I am pleased that this article, and the article in the Telegraph, saw straight through it.
Boris and his band of lying bastards thought we would fall for it. But we’re too used to their slimy tricks.
Imagine being healthy, keeping your own immune system in good nic, self-employed and law abiding… Doesn’t pay does it.
It does pay, but you will not be able to buy anything anyways. The new normal.
It does pay; it’s just that some of the benefit is going into your mental and self esteem “bank accounts”.
What frustrates me the most is that many of the sheeple desperately want this. What on earth can we do?
I’ll resist being vaccinated for now but soon I won’t be allowed anywhere or maybe even to be employed. There’s only so much resisting one can do.
Here’s an idea. Befriend a genuine believer who desperately wants the booster and wants it now, but doesn’t qualify. Give him/her your details and get them to present at a jabbattoir as you. Befriend another a few weeks later. Repeat. Congratulations, you are now double-jabbed! Maybe we could set up a dating service to match every sceptic to a bedwetting pincushion.
Stay strong. Don’t become a zombie to avoid zombiehood. It’s all or nothing. Contact your local resistance.
Declare yourself exempt, and take them to the cleaners for all the offences being committed – Discrimination, Equalities Act and so on. Alright, your solicitors would make a cut out of it, and keep the county courts busy, but that’s how it might work out.
Reality check here. Courts are organs of state and controlled by establishment figures – they are not going to help ANYONE in this morass.
It saddens me that Jonathan Sumption is a lone voice from the legal profession – how this country needs people with his skill and judgement; equally sad is I don’t see his ilk ever wanting to go into politics until after the civil war..
Of course “infections” won’t stay low this winter. The government controls how many “infections” there are, by means of the false positive rate of the PCR test (more tests = more “cases”), the tuneable nature of this test (more cycles = more “cases”), the lockdown policies (more masks and lockdowns = depressed immune systems = more “cases”) and the vaccine rollout (more vaccinations = more “cases”).
AKA ‘Red Facts’
Could not agree more or put it better – I just hope Reiner Fuellmich and his team succeed in a way that scares the shit out of Johnson and The Disaster Team so much they give in…
Have just worked out why these goons have been deified by the media and most of the public.
They are:
God Awful
God Damned and
God Forsaken
Off topic, but this one example shows that the majority know they’re being spun a yarn!
They didn’t get the response they expected!
https://www.facebook.com/80221381134/posts/10158207967261135/?d=n
Damn. I’m proud of these people.
(Apropos of nothing)
https://21stcenturywire.com/2021/09/14/220000-military-members-say-no-to-bidens-forced-covid-injection-lawsuits-filed/
Today I read in German MSM an advice to the school teachers to “not engage” with anti-corona “troublemakers” (i.e. parents) and instead “to call the police if house rules are broken”. The teachers were also warned that if they engage their responses might be uploaded to the Internet (*gasp*). So basically, the new role of a teacher is to shut up and call the cops on people who disagree. Well done, Germany!
The Original, and Best!
They had plenty of practice decades past.
Doesn’t take much for a people to revert to type.
They have just time-travelled back to the 1930’s
The “cheap” comment might be “well they are good at this sort of thing” but the Germans we have met – loads – are as far removed from this Dystopia as it is possible to be – lovely people, generally small ‘c” conservative, educated, literate, hard working, very polite and very animated when you (try to) speak German with them. Cleary that doesn’t describe them all, sadly.
I wonder if these GITS on the Sage committee will ever give up?
https://www.theguardian.com/world/2021/sep/14/bring-in-measures-soon-or-risk-7000-daily-covid-cases-sage-warns
They’ll be there until they’re pushed, or thrown under a bus.
At least, their last success was pushing back so-called freedom day by four weeks. This means their predictions of imminent doom have been tested for the first time since they starting making them (for the second, actually, as they already predicted a COVID tsunami which failed to materialize when schools were originally reopened this spring) and so far, and each and every of them turned out to be wrong.
The more often they predict something which fails to happen, the less influential they will become.
So much for “irreversible”. Rather like “three weeks”.
I have 2 kids just sent home with a consent form for the Fluenz Nasal flu vaccine containing 4 live attenuated virus strains, it even says on the back of the form that they are wild viruses. Is this not a good idea based on ADE and covid vaccinated people. It even says if they live with immunocompromised people they can’t have it as they will shed live virus for up to 2 weeks. The 4th wave??? Utter madness
Interestingly my vets warned that dogs aren’t to have the “live” kennel cough vaccine if there is a human in the house who is immuno compromised. Hasn’t happened before…
Check the ingredients. Oxford Univ may have a website to do this for the approved ones (not those with EUA).
Vaccines have got worse and worse as time goes on, maybe because they have to add proprietary ingredients to maintain their patent protection.
As Mike Yeadon said, the idea that healthy people need a vaccine against respiratory diseases with a low IFR is absurd.
You might want to also check out gut issues related to nasal ‘flu vaccines.
So tell me about Israel again LOL ???? Are we really pretending we are going to have a different outcome?
It’s funny how deaths and cases for the same time of year last year were significantly lower. Is that the ‘vaccine’ working it’s magic???
The Vaccine looks like a complete dud from the data i’m looking at. Unless a 4.5% ARR in over 50’s and 0% in under 50’s is considered a major success these days?
Thanks to the high uptake they are going to struggle to hide this. Of course the double jabbed who pass on the booster will no doubt be classed as unvaccinated to make the unter mensch numbers look worse than they really are.
We all know what’s coming sadly.
It’s worse than that, being double jabbed with waning immunity and new variants, this leaves your immune system wide open.
Yes I think you might be right which is why I think only triple jabbed data will be released, Those on double or single will be reclassed as unvaccinated to hide ADE if it becomes a reality.
see my post above. CDC already doing it. Massive fraud and people do not see through it, plus it reinforces public fear and doubles down on all the original lies. If it wasn’t so deceitful and sinister it would be clever.
What a bunch of knobs. No other words
So they are going to repeat all the mistakes they made in the past and introduce all the measures that failed to work in the first place – I think it was Einstein who said that insanity was repeating the same mistakes over and over again and expecting a different result.
This government is either completely insane or highly manipulative using psychological abuse to impose its authoritarian agenda. The sooner it is removed from power the better.
‘insanity was repeating the same mistakes over and over again and expecting a different result.’
It isn’t a mistake – they are achieving their aims.
I think they are both. Evil is both scheming and mindless.
Yes, but what do you put in its place? They are all putrid. Smarmer and his gang would be worse worse – hard to imagine, I know, but true.
Who believes a single word from these evil liars?
Its all about propaganda and how they can try and justify ludicrous laws and lockdowns. Look at Australia, that is what is coming.
It’s worse that Australia in a way: the gradual insidiousness means 95% still think nothing is wrong.
Agreed – if you are Australian and can’t see it in Oz then there is no help for you – at least here the sleight of hand and clever propaganda manipulation make it more difficult to see the abuse
I said it when the pot banging started and I’ll say it again now. FUCK THE NHS.
I clapped once or twice. Now they’ll section me and forcibly inject, no doubt.
Yeah it’s becoming nauseating
I concur
Im sure the tax hike will pay for this nonsense….or not
Destruction slow of small and medium businesses.
But infections will stay low because we have all been vaccinated surely .The minute this is not the golden apple then the vaccine will be rendered useless and their uptake will vanish.The govt have promoted a double narrative throughout this virus period .Protect the healthy ,send the elderly home from hospital .Get your vaccines ,vaccines dont offer full protection.Please get your second jab ,you now a need a booster .Constant ly shifting their plan as the bullshit behind each one becoms exposed .Its over .tell yourself ,tell your friend and tell your employer and then get then to tell everyone they meet .Its over (if you want it)
Even if millions die of the vaccines, the gov will not admit it’s happening. They can get away with it because too many souls are too scared to confront the harsh reality. This is what the Commies did very effectively for DECADES.
Hoisted by his own Petard?!
Sorry I don’t get it
Correlation between the vaccine rollout and the upsurge in cases, hospitalisations and deaths. The numbers to date are greater post vaccine, yet the answer is more vaccines! You’ll find this correlation in all highly vaccinated countries. For example, Israel, where nearly the entire adult population is vaccinated and proof of vaccination is required to access restaurants and indoor events, now rolling out a 4th round of shots as spread soars to record highs.
Reading this, I have the words ‘disgusting’ and ‘turds’ in my mind. I have nothing but contempt for these people.
https://twitter.com/SteveBakerHW/status/1437769574615764992
https://questions-statements.parliament.uk/written-questions/detail/2021-07-12/31381
Whitty and Vallance know this.
They all fucking know this!
Vallance is in this scandal up to his neck; he knows all about the development of SARS COV2 – see the Highwire and it is all laid out there as with other blogs – I could no more stand up and pontificate as he does than fly to Pluto on a brick.
Evening. I am perplexed as I listened to Whitless say you were 9 X more likely to die if you were unjabbed? .. yet in today’s daily sceptic it said those poor souls dying were 70% double jabbed . Anyone know the truth ? Please thx x
He is using this shambles of an analysis. It’s as bad as some of the scary graphs they presented in the past.
https://news.sky.com/story/covid-19-fully-vaccinated-people-made-up-just-1-of-coronavirus-deaths-in-england-in-first-half-of-2021-figures-show-12407019
And of course it doesn’t stack up.
https://dailysceptic.org/2021/09/14/why-is-the-ons-claiming-just-1-of-covid-deaths-are-in-the-vaccinated-when-phe-data-shows-the-true-figure-for-august-was-70/
So lockdown, social distancing, masks, and the added delicacy of vax passports are on the way, as it is obviously inevitable that numbers of infections and hospitalisations will rise as we go into autumn/winter. Beyond farce into dark, dark waters …
“Whatever action is necessary to protect the NHS”.
Like no more lockdowns or fear porn for example?
This must be the most authoritarian government in the history of British politics – this is a government that is hooked on control through fear – its a government that took away our freedoms under false pretenses and promised that the measures were temporary – now that promise to return those freedoms come with caveats and underlying threats that they will be confiscated once again whenever they feel the need to do so – this is what the start of tyranny looks like – this is the road to totalitarianism – this is a government that rules by fear this is an evil government.
Absolutely, evil personified!
Only if we let it.
What the fuck. Three jabs for over 70s in 10 months and that’s not good enough to stop veiled threats of lockdowns, useless bloody masks and anti-educational school closures?
Jesus, it doesn’t take any acumen in science to realise that something is deeply wrong with this strategy.
But hey, keep your heads in your sand pits … or up the arses of your conformant mates.
For God’s sake, just say “no” to more shit.
Hold the line, people, this is gonna get fucking ugly!
Exactly – we were told back in February/March that vaccines were the way out of this – vaccines were the road back to normal – well three jabs later including children and this government is still making threats to withold our freedoms – rights and privileges that were not simply handed over willingly but were swindled from us and stolen under false pretenses because they promised that it was temporary and would save lives – both were lies – this does not end until we all say it does – the more we comply the longer this nonsense goes on – and here’s another thing – this government must fall if there is any hope of returning back to normal – this is a government that can no longer be trusted – it is a government that addicted to the manipulative methods of psychological abuse to control and coerce people into doing their bidding – this is a tyrannical government.
Vaccinate the vulnerable and you’ll all be free and happy, they said as they loaded the sheep on to the lorry bound for the abattoir.
Hooray, we’re so happy, bleated the sheep as they leapt joyfully on board.
Re the cartoon at the top – maybe an alternative could be Commservative Gov
Johnson looks decidedly shifty in the middle of his 2 handlers.
The end game is the passport. It always has been!
Of course it is, then comes the credit score app as in China.Why people can’t see this is beyond me.
It’s quite apparent now that injecting yourself with one of the Government’s approved covid ‘vaccines’ is tantamount to giving yourself a form of lupus.
or worse!
Sunday javid says no passports no masks
johnson says no lockdowns
Tuesday all reversed again. Cruelty a sadistic game being played on the British public.
why lie and mislead on Sunday if they knew they would change on Tuesday. How can any business or indeed anyone plan with this bunch of sick people in charge
I genuinely think they are criminally insane and sadistic.
What happened to ‘Cry freedom!’ once the elderly and vulnerable were vaccinated? What happened to making sure we took our time unlocking to ensure it was irreversible? I don’t think Johnson knows or cares how many lies he tells anymore- just says whatever he thinks will make him look at any given point in time. I honestly think he exists on soundbites and forgets what he said immediately afterwards. No one can lie this consistently otherwise.
Whatever they say, it’s usually the opposite which is true. So they say they’re scrapping the vaccine passports…truth is they are preparing to introduce them. They say there will not be another lockdown…truth is another lockdown – or firebreak as they are now calling them – will be introduced at some point over the winter. SAGE are calling for even harder lockdowns. We should all know what the plan is by now – to introduce Digital IDs. On a global scale, this is extremely worrying, we are walking into a digital prison and I thought that 1984 was just a book, it seems it was a warning.
Well seeing as the NHS whine every year about being overwhelmed but never is then what does this even mean?
It’s a threat, fear again to get people to comply.
If the NHS cannot cope, scrap the NHS.
Yes, it’s a threat that plays well in the media and they’ll have a field day creating a whole host of fear porn headlines, lapped up by the masses and spat back in your face when having a chat about masks/vaccines etc with one of the converted. If the NHS can’t cope, maybe use some of that £38 billion from the magic money tree they wasted on Track n’ Trace, to build more hospitals and hire more doctors and nurses. And instead of clapping like a bunch of overexcited seals, actually do something that supports the NHS. I don’t agree with scrapping it – I think that’s the subplot playing out here anyway.
Please have some sympathy for the door soldiers who have to turn up, do the hard yards, bow and scrape to their utterly inadequate “higher administrative authorities”, go home , look after their families and themselves, get some rest and repeat the next day – and we are 21 months into this madness. Not great , is it?
Disgusting and still the British public remain compliant…
If passports can be brought in at a week’s notice, we all know they are printed up and ready to roll. Gaslighting the population is now becoming the way to govern. No debating, no voting and no democracy. How so many people can be under this globalist spell is proving to me that the Ascension is very close. The harvesting of souls. https://energeticsynthesis.com/index.php/79-energetic-synthesis/1791-what-is-ascension-2
Think Bob sums it up. Trouble is only a few of us can see it. On a brighter note I have been talking to one or two in my street who are getting pretty fed up. I’ve given Laura Dodsworth’s book to the lady at no.71. She had no idea about Ivermectin, the average age of death from/with Covid, the IFR or any of the basic stuff she had just been listening to all the guff from MSM etc. Hopefully her eyes are about to be opened. She seemed up for it after her mini education! Fingers crossed.
The scum know it is coming, just a case of waiting. As in after 1945, those brave Jewish camp survivors had a mission, a beautiful vengeful mission.
https://www.dailymail.co.uk/news/article-9990935/Former-Dragons-Den-star-Rachel-Elnaugh-slammed-vile-tweet-saying-Chris-Whitty-hang.html#comments
It’s inevitable! Colds and flu (COVID) season is imminent, and, as has been shown, the number of ‘cases‘ will undoubtedly be manipulated to show whatever Witless, Unbalanced and the Savage Jabber want them to be. The Manic Stream Media will gleefully promote it all to the quivering moronic masses.
T.me groups from around the country unite. Let’s Beat This Better Together.
Blake Park Bandstand Bridgwater Somerset –
Sundays from 10 am
Meet friends – keep sane – we are awake.
Telegram Connecting Warriors
In my working career as a surgeon most years in the winter months I had operation theatre lists cancelled because of pressure on beds : it will be no different this year for surgeons still working.
As we entered the post Christian era the UK population substituted the NHS God and the religion of NHS worship has failed to see the horrors that it is creating. It is when Governments are able to pronounce to public acclaim that it is the duty of society to suffer to “Protect the NHS” that the absurdity of this fanatical religious cult should be questioned. The cry emerging from some ITU consultants is that they are working to breaking point, when the units are not full but clearly there is a major problem with staffing as any hospital doctor can observe.It is a supply side issue.
It is not silly attempts to do something by pretending that several days old pieces of cloth extracted from a pocket have any part to play in altering transmission, or potentially damaging decisions to vaccinate children that will save the health of this country but stopping discredited guessing machine called epidemiologist such as Ferguson frightening people and removing Public Health doctors from a position of power.
To reduce demand stop creating morbidity by permitting patients with disease to go to a GP and get examined. Make it mandatory that all GPs work from their surgery and ban home working. You cannot exam one a breast lump of determine a referred pain on the phone. If GP’s don’t go to work pay them pro rata.
We should not be clapping the NHS but clapping individuals such as Carl Hennigan,Sunetra Gupta Julia Hartley Brewer etc who have kept alive the hope that there is a hope.
Bravo Sir, very well said and may I vote for you?
Please, please at least use the correct terminology and stop referring to covid infections. Covid is not an infectious agent it is a disease, which means you have to have symptoms. The infectious pathogen is SARS-CoV-2 which may or may not result in disease.
This conflation of terms is exactly what is being used to continue with the restrictions. If you have a positive test for the virus then you are a covid case, which is absolute nonsense.
And how many healthy teenagers who miraculously got tested positive overburdened the NHS exactly?
Go earlier and harder, before the numbers naturally go down. I think they should wait until the sheep have their third clot-shot – which, hopefully will take us ’til after Christmas. The un-vaxxed should then also have herd immunity.
Short and to the point https://tinyurl.com/duwjyx2r Mike Yeadon
Evil gits!
No doubt flu will be zero this winter again and COVID high. I hate these people with their Big Lie to impose totalitarianism. No evidence, no debate just assertions from nameless “experts” who don’t allow challenge.
And of course rates won’t ‘stay low’ this winter. It was declared openly last September that henceforth flu and ‘covid’ would be counted together. How fiendishly clever – ensuring that ‘rates’ will be inflated by flu anyway. The behavioural psychopaths certainly got their act together, didn’t they?
GB News on Twitter: “‘[Boris Johnson] straddles not just the centre, but the centre-right and centre-left. This is a major problem for Keir Starmer.’ Andrew Neil says the Labour Party are ‘running out of a place in the political spectrum.’ https://t.co/rE4MCUA8C7” / Twitter
The b*****d child of tony blair now rules. Not a genuine conversative party.
Big government = big trouble (as per history of the uk). No interest in addressing the huge public debt and a slave to the monolith nhs.
Time will tell….
Today my husband, who has cancer was told he could not have a blood test because there are no blood vials. Does anyone else think we have a problem? However, if you would like a dozen or more lateral flow test kits, just walk up to one of the thousand nhs mobile Covid units dotted around the entire country. Plenty of money to waste on that nonsense, and yet not a blood vial to be seen. We are in serious trouble folks, when the flipping nhs cannot provide blood tests as needed. Oh and if you want a flu jab, come straight in. Even though there will be no flu this winter. And once you have had your flu jab and your next Covid booster, things will be so confusing, no one will be able to separate fact from fiction. That should be fun
Sorry to hear your difficult situation.