NHS England guidance promoting universal masking in healthcare settings was quietly dropped on June 1st as part of the government’s ‘Living with Covid’ plans. So how is it that some hospitals and clinics seem to be making their own policies, with some mask-free and others aggressively insisting on masking both staff and public?
The reason is that the new guidance made masking policies a matter for local discretion. As a result, national COVID-19 guidance can be trumped by so-called ‘local COVID-19 prevalence’. But how consistent are local responses? By what set of rules are decisions to reintroduce masks made? And, most importantly, who is responsible for determining the rules and making decisions?
A return to masking?
Early in October, mainstream news outlets were reporting on the ‘return of the mask’. Between the Mail and the Sun’s accounts, eight different NHS Trusts were reintroducing a range of Non Pharmaceutical Interventions (NPIs), prominent among which were mask mandates for patients and visitors.
In all cases, these measures were apparently being introduced as a result of ‘Covid’s resurgence’ with “surveillance data suggesting Covid is on the rise in England”.
Just a month on from these heavily publicised reintroductions of mask ‘requirements’, the picture had changed somewhat. Table 1 shows the current status of mask requirements for the public. In some cases, the trusts who saw the need for restrictions have relaxed them, but they remain in full force for others.
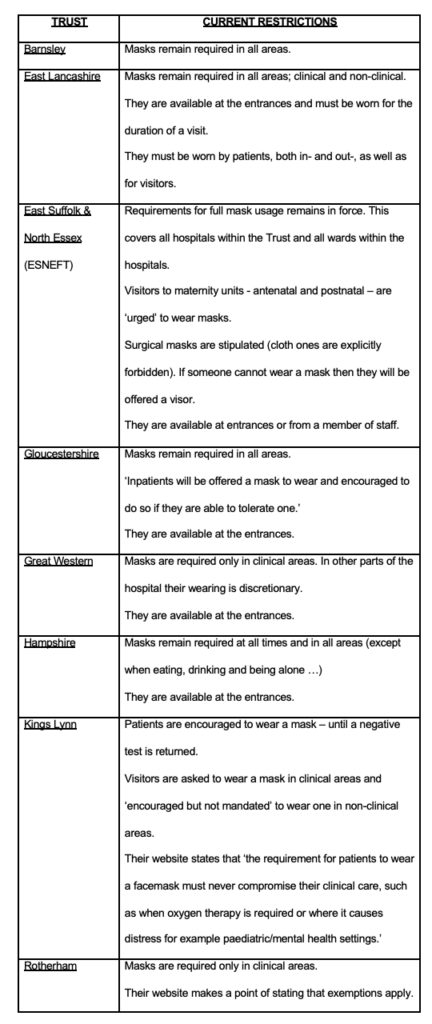
It is clear from the hotchpotch above that not all NHS Trusts are acting the same. Perhaps ‘local prevalence’ of COVID-19 can explain why we are seeing these differences? To test this hypothesis we can look at the infection ‘case’ rates in each of the domains covered by the Trusts, as documented in Table 2.
We should expect those Trusts imposing mask mandates to be in areas of above-average Covid prevalence. But, certainly at a high level, this appears not to be the case. Instead, there is no discernible pattern and, in fact, some discrepancies. For example, Barnsley, with continuing significant restrictions, has a catchment area with the lowest daily new cases per 100,000 people; while Swindon and its surrounding areas in Wiltshire, served by the Great Western Trust that has reduced its mask restrictions, has the highest rate!
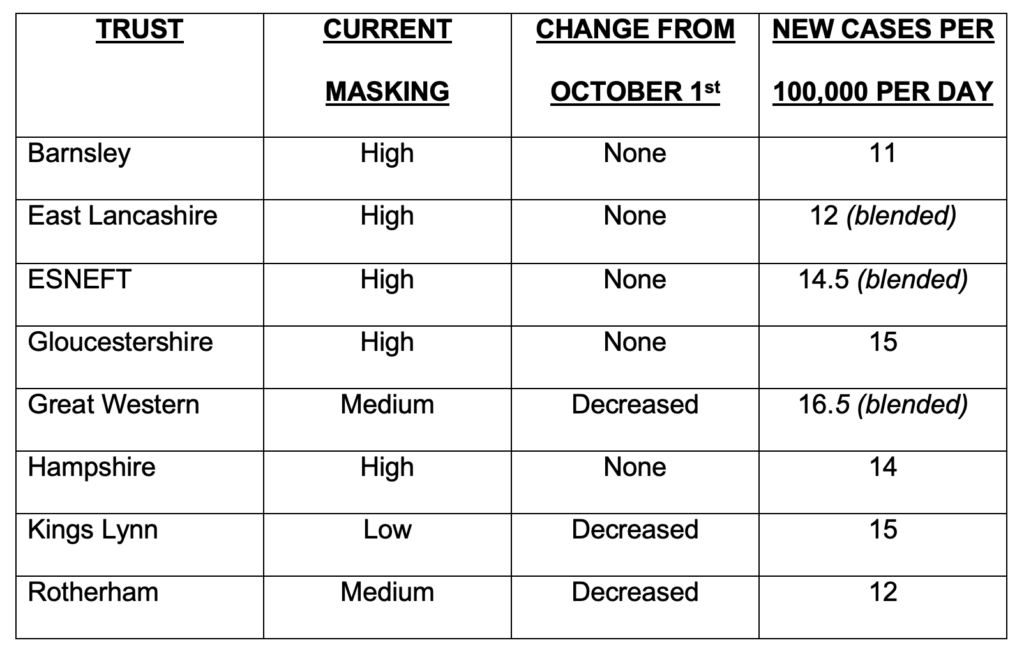
Source for ‘Cases’: GOV.UK Coronavirus (Covid-19) in the UK https://www.covidlive.co.uk
If local mask ‘requirements’ aren’t stipulated in national guidance, and ‘local prevalence’ of COVID-19 doesn’t explain it either, what’s going on?
Essex: a case study
Draconian masking – and other NPI measures – remain in place within the East Suffolk & North Essex Foundation NHS Trust (ESNEFT). This body runs the major hospitals of Colchester and Ipswich as well as several smaller community hospitals in the surrounding areas. It is worth noting that within ESNEFT’s bailiwick lie some of the most deprived areas of the entire country which also have some of the highest suicide rates.
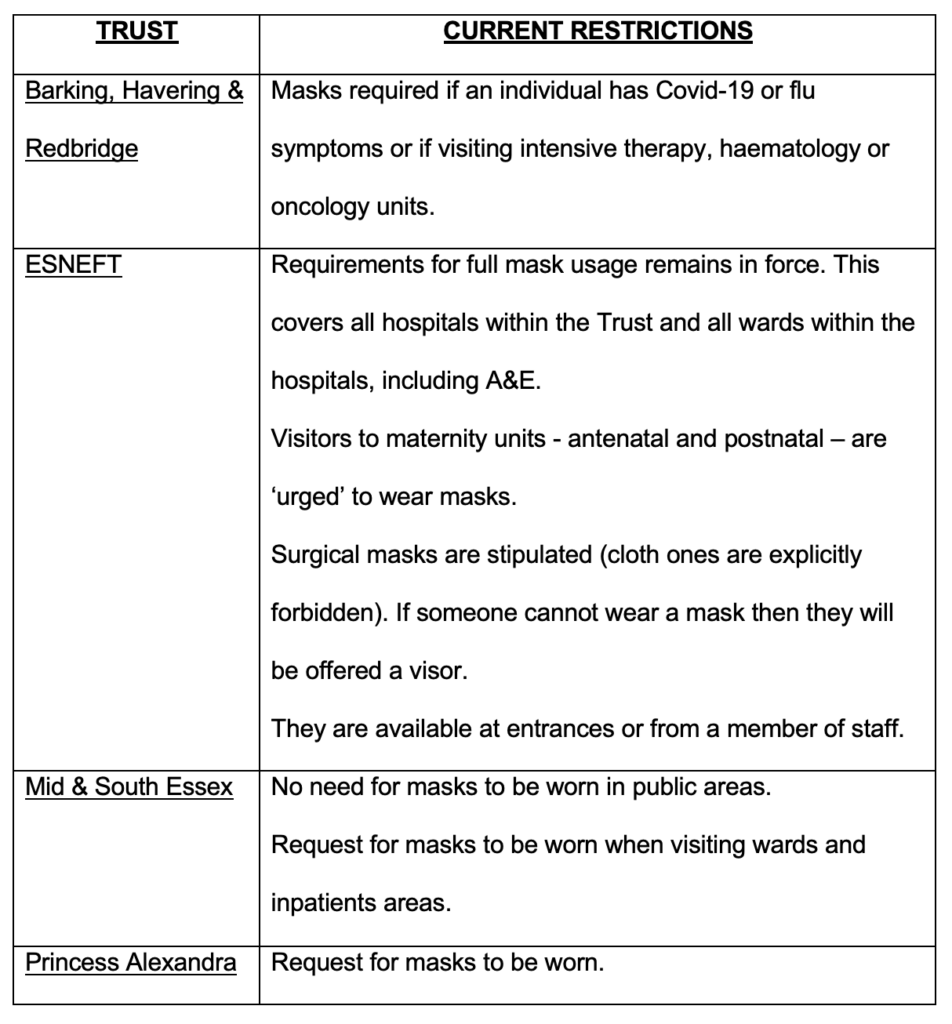
In addition to ESNEFT, three Trusts provide healthcare services in Essex. Each Trust runs multiple hospitals and covers specific geographic areas. How, in terms of mask mandates, does the ESNEFT Trust compare to the others? Table 3 documents the face covering requirements at the health establishments run by the other three Trusts operating in the county and reproduces the rules at ESNEFT.
The profile of a masking decision-maker
The man responsible for ESNEFT ratcheting the restrictions upwards is Giles Thorpe, Chief Nurse and Director of Infection Prevention & Control (IPC).
Doctor Thorpe is not a medical doctor, rather he is a “senior nurse leader” and an “honorary professor”, with a professional doctorate in health service management awarded by the University of Essex in September of this year. If you were uncharitable you might say he was an NHS bureaucrat. “Once you accept that some part of you might be racist, you may then need to accept your white privilege,” Thorpe is quoted as saying in an NHS website article entitled “From bystanders to activists”. Indeed, sensitivity to racism appears high on the agenda at ESNEFT. In 2019 Thorpe’s boss, Trust Chief Executive Nick Hulme, went on record to declare that the region his Trust provides health services to was “probably the most homophobic, racist, awful place in some senses to live in the country”; his track record as an actual administrator of health services meanwhile appears somewhat chequered.
When it comes to countering COVID-19, Dr. Thorpe is an earnest observer of infection rates within the Trust’s catchment and a firm proponent of NPIs in general, and masking in particular. For example:
● June 2021: In his first IPC annual report, without supplying any evidence to back up his assertion, Thorpe noted that “causes of COVID-19 outbreaks in the hospital wards” were, in part, due to “lack of offering patients to wear masks (sic), and lack of uptake by patients to wear a mask”;
● December 2021: just in time for New Year, ESNEFT suspended visiting rights for their health venues. Dr. Thorpe was quoted in the press as saying that “by keeping a close eye on community COVID-19 infection rates and the number of people in our hospitals with the virus, this is action we really need to take now”;
● January 2022: Due, according to Thorpe, to “a rise in positive coronavirus tests among pregnant people (sic)”, new rules restricting visits to maternity units in east Suffolk and north Essex were put in place;
● March 2022: Faced with rising infection rates, visitors were banned completely from ESNEFT venues, with Dr. Thorpe commenting that the Trust was “committed” to reinstating some ward visiting “as quickly and as safely as possible”;
● April 2022: Notwithstanding falling COVID-19 community infection rates, the Trust kept visiting restrictions in place, although Dr. Thorpe said: “We did manage to open some visiting for patients who have been in hospital for more than seven days before the Easter weekend.”
Given the lack of robust evidence to support mask-wearing, and the known harms, particularly in healthcare settings, the Smile Free campaign recently wrote to Dr. Thorpe, posing the following questions:
● What robust, real-world evidence are you drawing on to support the re-imposition of mask requirements?
● Do you believe that the evidence for masks significantly reducing viral transmission is sufficiently strong to justify insisting all staff, patients and visitors wear them?
● Given the wide range of potential physical, social and psychological harms associated with habitual masking, have you conducted a comprehensive risk/benefit assessment addressing the likely consequences of this policy decision?
● Including both the wholesale cost of the surgical masks, together with the salary of the monitors at the hospital entrances, how much is your Trust spending each year on implementing your mask requirement? Given the huge financial pressure the NHS is under, do you believe that this is optimal use of tax-payers money?
● It is admirable that you recognise the importance of “patient experience”. But what’s the likely impact of mass masking on the experience of a confused, elderly, hard-of-hearing person in one of your medical wards or a frightened child, in acute pain, attending your Accident & Emergency Department?
● It is admirable that you seek to give a voice to the “lesser heard groups” and to ensure that the “stay silent” groups are heard. But in re-imposing your mask requirement have you listened to your autistic patients, or those with histories of physical and/or sexual abuse, or those with recurrent panic attacks, many of whom suffer extreme levels of distress as a direct consequence of face coverings?
Dr. Thorpe replied, without answering any of the substantive questions. Confusingly, he said “we support and respect anyone’s decision to wear a face mask, or not, while they are in our hospitals”, while in the same email confirming universal masking had never gone away in “A&E, our urgent treatment centres, and assessment areas (and) areas where we treat immunocompromised patients”, and saying “we reintroduced mask wearing for visitors to our wards in September”.
No doubt Dr. Thorpe believes he’s doing the right thing. It’s just a shame that the 10,000 patients reportedly seen every day at ESNEFT are still being subjected to safety theatre with no evidential backing, going into a third year of the Covid saga, seemingly driven by a very small and unaccountable infection control team, if not in reality the whims of one man. If your local healthcare setting is still insisting on masks, find your ‘Giles Thorpe’ and ask him or her or they the same set of questions.
Perhaps we should not be surprised, because the over-valuation of masks goes to the very top of the NHS. As recently as October 4th, Dame Ruth May, Chief Nursing Officer and national lead for infection control at NHS England, was justifying mask advice to hospitals with “highly uncertain” computer modelling linked to Professor Neil Ferguson’s Imperial College that is literally labelled “Should not be used to inform clinical practice” on page one.
As Smile Free wrote in June when the NHS guidance changed, “two years after the imposition of masking in English hospitals, it is most regrettable that NHS England and the authors of this latest guidance (Professor Stephen Powis and Duncan Barton) could not simply have signalled a clean break and consigned this unprecedented, poorly-evidenced, and ultimately failed policy to history. Since they have chosen not to, by far the most likely outcome is that masking in English hospitals will now become a ‘postcode lottery’ based on the whims of local staff.“
And so it has come to pass.
Stop Press: A new RCT has concluded that N95 masks are no more effective at stopping transmission of the virus than ‘regular’ medical masks. The Brownstone Institute has more.












To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
They could do a matched cohort study into the effects of masking in a healthcare environment on the spread of Covid and other respiratory tract infections (there are about twice as many people in ICU with influenza as with Covid in the UK at the moment).
Except that they won’t, because they’re not at all interested in finding out whether the measures work.
This new study just did it for surgical Vs N95 and found no difference.
https://brownstone.org/articles/not-even-n95-masks-work-to-stop-covid/
It is obvious why they did not create a cloth masked and/or unmasked cohort too.
Addenbrookes found FFP3 masks (equivalent to what would be called N99 in North America) quite effective for their staff… when replaced twice a day. https://elifesciences.org/articles/71131
This is the wrong discussion. It doesn’t matter if masks work, whatever that’s precisely supposed to mean and for as long this is being discussed, people who are convinced that they do work (and who will always remain convinced of this as people only extremely rarely change their opinions just because they’re demonstrably nonsense) will try to enforce their usage. The proper question to ask is: Are people people and thus, generally masters of their own actions, or are they just another sort of domestic animals experts can principally manage in whichever ways suits their whims? Including requiring them to put on any kind of fancy dress said experts deem necessary.
I was in Asda last night, customers and staff mask-free apart from a couple of loonies. However the staff in the pharmacy were all masked up – I think they like feeling as if they are “medical”. It’s like some kind of pathetic pantomime, an extra prop to go with a white coat.
I think you may be right. This morning I popped into Boots (in Wellington, appropriately enough) to buy a knee brace, and all the sales staff were wearing masks.
Same in my local big Tesco – and they still have massive screens up, which combined with their mask wearing makes it very difficult to hear what they are saying.
A small independent chemist in a nearby town no longer has these measures.
A couple of months back, I was in a branch of ASDA that has an optician’s department that I used. The Optician wanted me to wear one, which I refused, but he did his job. Later on, the other staff – including the one that did the real close up work to fit a new set of specs – were quite content.
The other places I used earlier in the year were the Great Western A&E department, and a dentist’s surgery, At the A&E, I was dealt with in a couple of hours, for a minor, albeit nasty looking graze. Normal for the doctor doing close up work on things like that; I did not. At the dentists, one of the receptionists wore one, and the other did not. My dentist was not doing specific work that normally need one either – just a routine check up, and he appeared quite normal and did not wear one. None of the other patients in the waiting room did not.
The whole thing was a bureaucratic lottery, including the idea that anyone believes in their efficacy re the transmission of such tiny compounds!
I walked past Specsavers this morning and there was a staff member sort of guarding the shop just inside the door at some kind of security checkpoint station, wearing a face nappy. In the mad world of the covidian, masking up in “medical” settings like a doctor’s waiting room or even a pharmacy where you are likelier to encounter sick people makes some kind of sense, as does masking up if you’re working at close quarters like a dentist or an opthalmologist. But specsavers reception is not a bloody medical setting. Clown world.
East Yorkshire Family longtime GP who I thought I knew really well through family births and deaths. Haven’t been for years. Had an eye problem. Was only seen outside at 6 pm because I wasn’t allowed in the surgery (the receptionist genuinely didn’t know how I was going to be seen) due to my inability/refusal to wear a mask. GP (older and I thought very sensible till now) came out wearing something like WW1 – I assume one of the N95 ones and had a quick look outside in the dark with me standing on the doorstep. It’s fine and ‘stay out of the cold wind’ wasn’t terribly helpful as I spent alot of time outdoors – but what would I have done if I’d needed to take some clothes off?
“By what set of rules are decisions to reintroduce masks made? And, most importantly, who is responsible for determining the rules and making decisions?”. With the risk of sounding a little pedantic, actually the most important thing is do we have to comply? No, regardless of the rules and whoever is making the decisions, no matter what the setting, we must never comply.
Are they allowed to refuse treatment if you do not wear a mask? In June I was refused a breastscan because I did not wear a mask… I kicked up a fuss and they sent me to another scanning location. I’m now pursuing this as a formal complaint, pointing out that the survival rate of Covid is 99.9%, and the 5 year survival rate of breastcancer is 85%. So much for “heroes of the NHS”.
If anyone is being forced to wear a mask in the working environment, clinical or other, you can get support from the Workers of England Union. They are fighting hard for nurses, midwives, theatre staff, doctors, care workers etc, taking the fight to their employers.
Employers are breaking the law imposing blanket policies without exemptions. PPE is very tightly regulated (the government knows this) and very specific risk assessments and fit testing needs to be undertaken. Employers are ignoring their duty of care to their employees, rendering them negligent and culpable for any injuries or damage suffered.
Head over to workersofengland.co.uk
As someone in East Lancashire I can comment on this. I am accompanying someone to hospital regarding cancer.
Blackburn hospital – most staff wearing masks though some under their chin and most amusingly I watched one take her mask down to talk to a patient. Signs about masks about but not consistently. Happily there are no bouncers on the door now to check compliance. No one asked either of us to wear a mask, and most consultants aren’t bothering. Patients are mostly not bothering either.
Cancer centre – not a mask in sight among staff and patients apart from a couple of nervous patients. No signs requiring them.
So the east lancs rules are not applied consistently.
One other titbit from this part of the world – a nurse recently asked if there was much covid in hospitals said no, it’s all strokes. When asked if that was vaccine related, she said “I’ll tell you what we’ve been told to say: I can neither confirm nor deny that.”
As in Australia, the health bureaucracy is composed largely of non-doctors or ex-doctors (who may have practiced for a couple of years 30 years ago), then get given wonderful titles like “Professor of Public Health”, and then have politicians and the media fawning over every word, and giving them unlimited power. These roles appeal to the Machiavellians and narcissists, whose whimsical pronouncements become “The Science”.
Also, as we now hit summer, I’ve noticed an increase in mask wearing. Usually frightened old sheeple types (though some younger), often alone and outside.
Excellent article and well researched. I fear that since mask wearing is not based in science or on logic that we will never be able to counter it with reasoned discussion, although we have to keep trying.
I find it appaling that someone with the ‘rona or flu are being to to wear a face nappy.
For goodness sake they need to be able to breathe freely and not have their breathing further impeded by a non-functional bit of paper.
In a nutshell the problem with the NHS is that the Giles Thorpes of this world not only gain employment in the organisation but are also elevated to positions where they make decisions which impact on the people paying their (usually excessive) salaries.
As for his comment that “part of you is racist”, does that part have to be a complete organ system, a whole limb, part of a limb or a specific appendage?
Truly, evidence based decision making has been replaced by moronic, hysteria based decision making.
It seems that Infection Control breeds such idiots. When I was an inpatient a while ago Infection Control had decided that all sinks would have their plugs removed. Perhaps they got a bonus from the local water company?
I was in a hospital A&E recently waiting hours to be seen. As people were called, the doctor/nurse was telling them to use the hand sanitizer. One person was told to wear a mask because he wanted to go in with his ill companion. I heard the reason given was that “if we get covid we have to be off for such and such a length of time.” So the staff are all scared of getting covid.
You can’t get covid if you don’t take a covid test. When will they go back to treating a cold as a cold and stop all this covid theatre nonsense?
I have recently been to my GP and was asked to wear a mask. I refused and they said nothing. I also went to the hospital and the appointment letter said masks must be worn. There were signs everywhere and I ignored them all. Everybody was masked up, patients and staff, and nobody said a word to me. Stand up against this medical tyranny.