As an Englishman living in France who worked in the NHS some long time ago, it is of great sadness to me that both political dogma and the refusal to accept criticism of what has become a national icon manages to blank out any consideration that methods and experience from elsewhere could ever be applicable in the U.K.
This is particularly so in the NHS, where the dogma that the Government has to be directly responsible from taxation for the administration and supply of health care has been inbuilt for so long. It seems that from its earliest days the NHS that was set up as if patients were incapable of having any responsibility for their own health and therefore the Government had to take on that administrative responsibility. This may be one of the reasons why the NHS has been continually overburdened with self-perpetuating and ever-growing bureaucracy.
This combined with ‘free at the point of use’ was particularly damaging. ‘Free at the point of use’ in the U.K. encourages people to regard the access to such services as being free and as of right, encouraging time wasters and thus unnecessary use of medical services.
‘Free at the point of use’ is also a fallacy as so little in the NHS is actually free at the point of use – there are prescription charges, dental costs and the endemic rationing, which itself translates into huge costs for the individual patient.
So why are things so different here in France, where national expenditure on health is on a par with the U.K., yet we get far more bang for our buck?
First, the system is run on an insurance basis based on income, supervised by the state but not directly administered by the state. The system has 100% state protection for the low paid, the chronically ill, pensioners, children etc.
Normally, the state pays the larger part but not all the medical costs. Individuals have the option to buy supplementary top-up insurance (mutuelle) to cover the balance. This ensures that people do have an understanding of the value of their healthcare.
In France, health provision is supported by a very effective IT system. It was originated as early as 1982 with the Minitel online system, although it has now been superseded by the Carte Vitale.
The Carte Vitale is a type of credit card with a chip issued to all insured patients. It provides the data required for the insurer to pay the sums necessary to whichever health provider has been used. It retains minimal health information, such as the chronic illnesses for which the patient is due full reimbursement. Most health professionals, such as the GP, have card readers and are reimbursed directly through the system. The Carte Vitale can be updated on a terminal at any pharmacy. There is a parallel manual system which can be used by any small-scale provider, for example the visiting chiropodist.
The insurance organisations provide regular reports to the patient noting all the payments that have been made on their behalf, thus ensuring that the patient knows the value of the health care he or she has received.
Importantly, GPs are not paid by a capitation fee based on registered patient numbers but on their actual patient appointments. This means that there can be a modicum of competition between them as health providers. Well-liked health providers are successful and as busy as they want to be. And the patient retains his or her ability to choose.
Only recently, a system of affiliating patients to particular GPs has been introduced; before that it was totally open to the choice of the patient on any particular occasion.
All the providers in the system – the GPs, consultants, diagnostic labs, district nurses, etc. – are either private company groups or self-employed private contractors within the system. But they normally work at the nationally prescribed fee scales.
The contractors in the system choose their mode of working from the point of view of their own businesses and personal circumstances within those fee scales. This results in health service outcomes most of which would be remarkable in the U.K., other than in the costly private sector:
- My GP has no secretary and no appointment system. Turn up when you need and wait perhaps 20 minutes on a busy day.
- The GP will also be happy to make home visits; the reimbursed charge is rather more.
- The patient also has the choice of which consultant to see and can contact the consultant’s office directly without GP referral, but the GP will always recommend the one he or she considers suitable.
- The district nurse will turn up on the doorstep to take a blood sample at 7am in the morning for a fee of €6.35 (reimbursed).
- The pharmacist will provide over-the-counter advice and drugs for almost any common aliment. He or she will also provide prescription drugs (un-reimbursed) if needed at his discretion. Thus the load on the GP is much reduced.
- The dentist has no dental nurse and runs the practice single handed. A large proportion of his fees are reimbursed to the patient.
- The busy cardiology practice with three consultants has just one administrative assistant.
- The consultant dermatologist answers his own phone and makes his own appointments without any need for administrative help.
- As well as doing major surgery, the consultant orthopaedic surgeon does not hesitate to do his own minor splint work on the spot.
- There is a rigorous system of reminders about medical appointments by text and email so the waste from missed appointments is unusual.
- Etcetera etcetera.
Thus, the administrative load created by centralised control and rationing of access to consultants, treatments and hospital appointments does not seem to exist.
As separate private contractors, all health professionals work as if their time was their money. Most U.K. hospital consultants are already private contractors as well as being well-paid part-time Government employees. A piece-work remuneration system has been working for dentists in the NHS for many years. In France this also applies to GPs and their remuneration does not seem to be excessive as it often is in the U.K.
Prior to any hospital intervention, all the necessary preparatory checks take place as outpatients including blood tests, anaesthetic checks, cardiac checks etc. This means that inpatient hospital time is not used for these preparatory activities.
In France there is a real emphasis on preventative medicine and prompt treatment is considered to be economically worthwhile. Thus, certainly in my experience, long waiting lists just do not exist. In addition, speaking as a pensioner, the health service does not seem to think that age is an impediment to treatment.
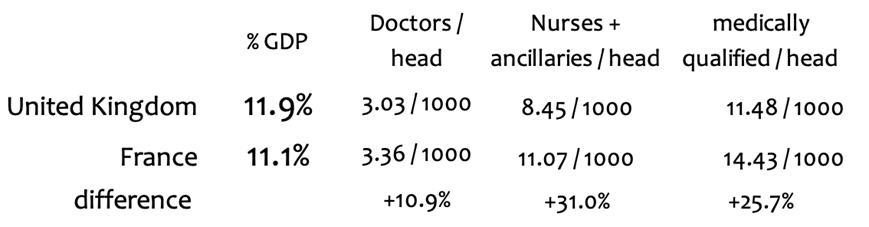
There is certainly an abundance of medically qualified people in the system and indeed there is a degree of real competition between them. According to OECD figures, there are around 25% more medically qualified professionals per head of population than in the U.K. health service. They are not rewarded with the high salaries received in the U.K.
The medics seem to control the running of the hospitals and other facilities, not the Government. They see the benefit of having an absolute minimum of administrative overheads. Those that exist are mainly involved with ensuring that the various state mandated insurance organisations are charged correctly.
This also means that there are no artificial limits placed on maximising the use of expensive capital equipment and the hospital installations.
Also, crucially, as the Government is not supplying the service, the state does not own the product of the service, nor, most importantly, the patients’ medical records.
Patients have bought the service via their insurance: they are therefore the owners of the results. The responsibility for the ownership of such records is reasonably unloaded on to the patient. As the patient owns the records, he or she is freely able to read them and understand them to the best of his or her ability.
This eliminates another whole swathe of administrative costs. As there is no Government duty of care with regard to patient records, there is no demand to create an expensive nationwide database of everyone’s medical records, as was tried and failed in the U.K.
The ambulance service is merged with the fire service as a single emergency service. Voluntary membership is prestigious in the community. If you have a regular treatment appointment, say for radiotherapy, a taxi will come and fetch you and bring you home – all part of the service.
In other words, the French health service is pretty well ‘privatised’, and that’s why it works rather well.
The nation’s health, not the National Health Service, should be the priority of Government.
The NHS is certainly not the only way to organise a Health Service and the clear alternative evidence is just across the channel. But dogma means that the Brits will never want to learn from foreigners.
Find Ed Hoskins’s blog here.











To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
And what about the Police taking the knee for BLM
The UK police officers are considered servants of the Crown and holders of the Office of Constable, not employees. This means they are not employed by the police force, but rather appointed by the Crown. The uniform, while standardized, can vary slightly by force and is subject to local policies. Crown-related symbolism, like the Tudor Crown, is also incorporated into police crests and insignia. The Police wear the Crown and they submitted the Crown to a Marxist mob that rioted and also desecrated the Cenotaph.
What about Starmer and Rayner taking the knee for a known criminal, our politicians are detestable.
Yes. That was treason.
An individual belonging to a protected category victim-group complaining about police impartiality surrounding a different protected category victim-group. The system will uphold the complaint. It has successfully dismantled the old normal and now works towards dismantling the new normal. The introduction of a new society requires complete destruction of the old society, which requires division – the more division the quicker the new society will be installed.
METROPOLITAN POLICE FOR THE NEXT CASE PLEASE
This is undoubtedly excellent news, not just for Linzi personally, but for all of the decent LGB community who wish to rightly distance themselves from the toxic, degenerate mental illness ideology that the TQ+ lot represent, for women standing up for their sex-based rights and for free speech in general. Only the biggest cynics wouldn’t see this for the win that it is. Now this needs to be implemented across ALL police forces in the country because none of them should be participating or showing support for this dangerous and perverse child mutilation cult which provably harbours sex pests and paedos;
”High Court Rules Northumbria Police BANNED from Pride Festivals!
Huge congratulations to We Are Fair Cop and @RightNUFC for their tireless efforts in pushing for this change!
In a landmark decision, the High Court has ruled that Northumbria Police can no longer participate in Pride festivals, citing concerns over the politicisation of law enforcement.
This is a MAJOR win for police neutrality!
For too long, police involvement in Pride events has sparked debate. While some see it as a gesture of inclusivity, others argue Pride’s political undertones compromise police impartiality. The court agrees: law enforcement must stay neutral, avoiding alignment with any social or political cause.
This ruling prohibits Northumbria Police from marching in Pride parades, displaying Pride symbols on uniforms/vehicles, or officially endorsing these events. It’s a clear message: police should focus on public safety, not activism.
Their campaign highlights the importance of keeping our police force impartial and accountable.
What’s next? This could set a precedent for other UK police forces, prompting a rethink of how they engage with community events. The decision may spark broader discussions about the role of Pride and the balance between celebration and politics.”
https://x.com/GerryKeogh_/status/1945498589368873359
I’m surprised so many gay and lesbian people still seem to associate with pride now it’s almost exclusively focused on transgender rights which are often anti gay/lesbian. One example is the fact that quite a few gay/lesbian young people go through a phase of thinking they might be trans as they realise and come to accept that they’re same sex attracted. The trans activists rush to confirm these youngsters temporary trans beliefs and push them onto a path to puberty blockers, surgical mutilation, loss of pleasure in sex etc. rather than letting then grow out of their trans beliefs and become happy same sex attracted adults.
All reasonable gays/lesbians should abandon pride and join the LGB Alliance.
Do you know what the best thing would be? And it’d be a test to see who’s really bothered about attending this crapfest because they’re bound to whinge the loudest, and I can take a confident stab at who that’d be…
Do a Viktor Orban and ban the entire thing. I’d gladly see the back of it.
But I think we can safely say that’ll never happen in this part of Europe, and we all know why. This lot ( much like the Muslims ) wield too much power now and must be appeased and pandered to, no matter what. This toxic ideology has got it’s feet firmly under the table and isn’t going anywhere. I doubt even Farage would have the balls to do a Trump or Orban and risk upsetting the transmafia.
Just a bit of supporting evidence to my above post;
“Keir Starmer has hosted a ‘Pride Reception’ in Downing Street.
Speakers included men in dresses identifying as women.
He committed to hosting a ‘LGBTQIA+ Roundtable’.
One attendee said that Starmer has “real understanding of the challenges queer people face”.
Worrying.”
https://x.com/JamesEsses/status/1945391679957012826
I’m sure the Muslim Party will sort it out when they hold the reins of power.
A great win. And now let us have who made the decision to take part either fired or demoted to a PC.
It was the chief constable who ordered her force to take part. She writes articles about how proud she is to be a lez. Thank goodness there are sensible homosexusls to rein in the exhibitionists.