Since the start of the pandemic, one of the main justifications for lockdowns – at least in democratic Western countries – has been the “externality argument”. This is the argument that government is justified in restricting our freedom in order to prevent us from harming others – which we might do by transmitting a deadly virus.
As the scientist Richard Dawkins stated back in September:
You can argue over whether masks, handwashing, banning groups etc are effective. What you can NOT argue is that you are personally entitled to take the risk as a matter of individual liberty. You risk other lives as well as your own. It’s just elementary epidemiology.
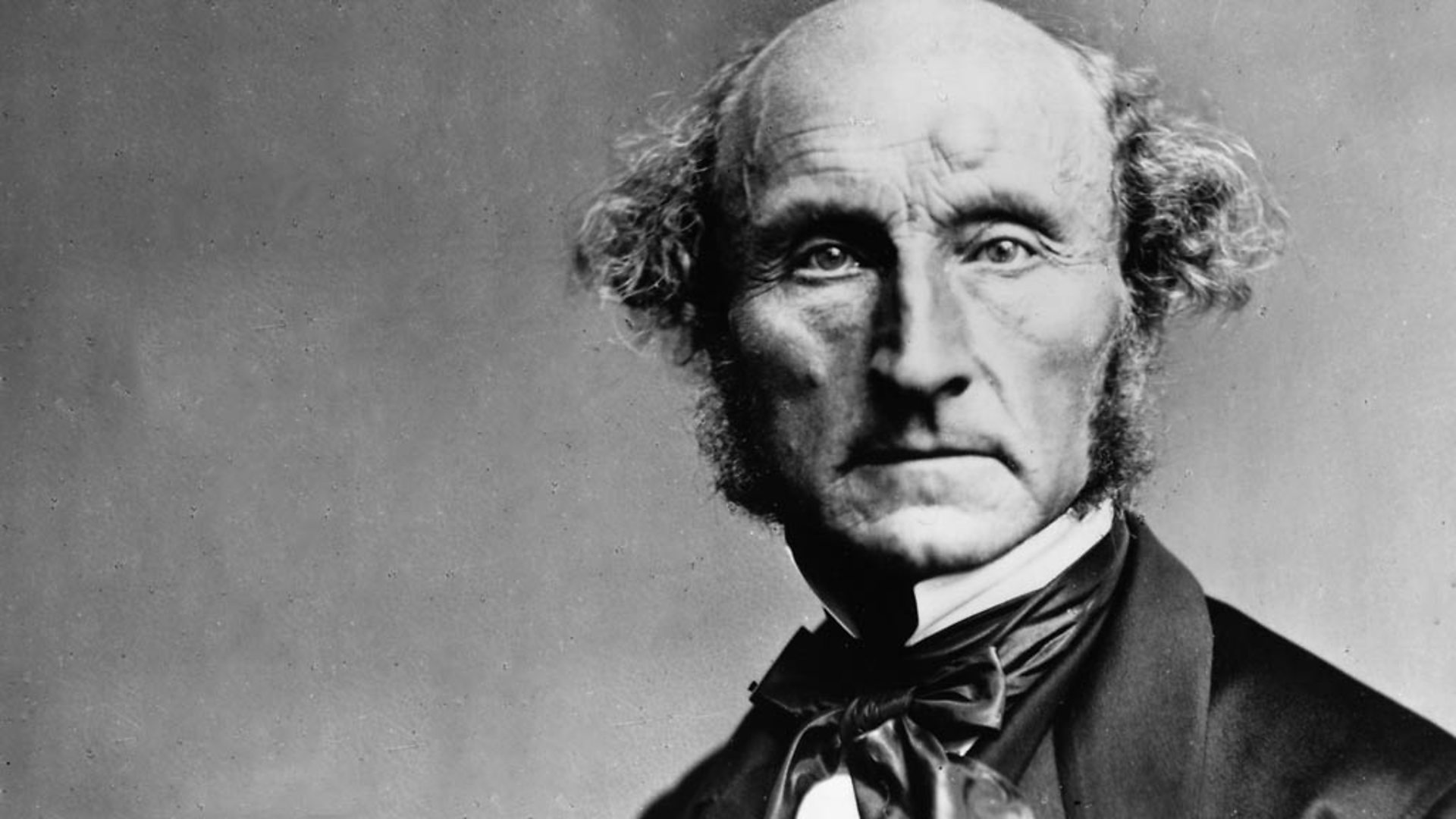
Proponents of this argument sometimes appeal to John Stuart Mill’s harm principle, which states, “the only purpose for which power can be rightfully exercised over any member of a civilised community, against his will, is to prevent harm to others”.
While the “externality argument” does have merit, the situation is more complicated than its proponents would have us believe. In a recent article for the Southern Economic Journal, the economists Peter Leeson and Louis Rouanet explain why.
Before getting to their arguments, it’s worth explaining what an “externality” actually is. In short, it’s a cost imposed on someone who did not agree to bear that cost. The classic example is pollution. When a factory releases toxic waste into a lake, this may poison the water, leading to illnesses or deaths among users of the lake. Since the lake users did not agree to be poisoned, the release of toxic waste is an externality. And most people would say it justifies government intervention.
However, the externalities associated with COVID-19 aren’t quite like this, as Leeson and Rouanet point out. First, when one individual transmits the virus to another, this has both negative and positive effects. It has a negative effect on the person who catches the virus. But it has a positive effect on vulnerable people who are self-isolating, since each infection reduces the time until herd immunity. And the sooner herd immunity is reached, the sooner those people can return to the community.
Second, COVID-19 externalities are often self-limiting. Since most people would prefer not to catch the disease, they have an incentive to avoid behaviours that increase the risk of transmission (such as attending large gatherings). This is in contrast to the factory example, where the owners have an incentive to release as much waste into the lake as possible. And indeed, evidence suggests that voluntary social distancing has much more impact on the epidemic’s trajectory than mandatory lockdowns.
Third, many interactions that result in transmission occur on privately owned sites that individuals enter voluntarily (e.g., shops, restaurants, cinemas). Absent force or fraud, there is therefore no on-site externality. What’s more, since businesses compete for customers, they have an incentive to take measures that reduce customers’ risk of infection (e.g., increasing ventilation or imposing capacity limits).
Fourth, the main externalities associated with COVID-19 are actions taken by individuals at one site that affect the infection risk of others at different sites. For example, if someone attends a party that results in a super-spreader event, he and all the other party-goers impose costs on society by increasing the general level of infection. This requires individuals and businesses to take measures to reduce the risk of infection they and their customers will face.
While there is a case for government intervention to reduce “cross-site externalities”, the total costs of such externalities are limited by the cheapest measure that can be taken to avoid them. As the authors note, if “an individual can avoid infection with certainty by wearing a hazmat suit, then under no circumstance can the external cost imposed on him exceed his cost of wearing a hazmat suit.”
However, there does seem to be a weakness in the authors’ argument. While it may be true that healthy adults enter privately owned sites voluntarily, and are capable of taking measures to reduce their risk of infection, the same cannot be said of frail elderly people living in care homes and hospitals. And of course, a large percentage of fatal infections have occurred in precisely these settings.
A frail elderly person living in a care home does not voluntarily accept the risk she faces in the same way that a healthy adult entering a restaurant voluntarily accepts the risk he faces. The interactions associated with care homes and hospitals therefore require further analysis.
One issue the authors don’t touch on is the externalities of lockdowns themselves. While lockdowns may correct for costs that some people impose on others in terms of higher infection risk, they impose new costs on everyone – regardless of whether you contribute to the externalities of viral transmission. (And of course, the evidence suggests they don’t have much impact on viral transmission anyway.)
Even if you’re not convinced by their arguments, Leeson and Rouanet’s article is worth reading in full.










To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.