by Dr Clare Craig FRCPath, Jonathan Engler MBChB LLB and Joel Smalley MBA
Viruses do not disappear. When a novel virus is introduced to a naive population there will be an epidemic. Spread will be exponential, some susceptible people will die but eventually we will reach a point where there is sufficient population immunity that spread is slowed and the virus stops spreading in an epidemic fashion. Thereafter, localised outbreaks can still occur and susceptible people can still die but there is no longer a risk of epidemic spread because every outbreak is contained by population immunity.
Coronaviruses are seasonal, so it is only now that we have had some winter weather that we can assess what endemic Covid will be like.
Figure 1 shows the sharp spike in excess deaths seen with epidemic Covid in spring. These deaths were in excess of the usual winter hump. Compared with previous years, this year’s winter excess deaths started earlier but the shape of the curve is consistent with previous years. However, we have now reached the bizarre situation where so many deaths are being labelled as caused by Covid that, for the first time ever, this winter there are fewer non-Covid deaths in winter weeks than there were in summer.

Figure 1 Total deaths by date of occurrence shown in green line. Summer minimum (dotted black line) used to calculate winter excess deaths shown beneath in blue. Covid labelled deaths are coloured red.
Doctors have noticed that unlike in previous years, their patients have low white blood cell and platelet counts, sudden hypoxias and bilateral atypical pneumonias. These features can be seen in other pneumonias but are characteristic of Covid and are being seen in large numbers currently.
However, the numbers of patients presenting through Accident and Emergency with an acute respiratory infection (which includes those categorised as Covid-like) is well below normal levels. Also, the total number of patients in hospital remains the same or even lower than in previous years despite a third of patients being diagnosed with Covid in some areas.
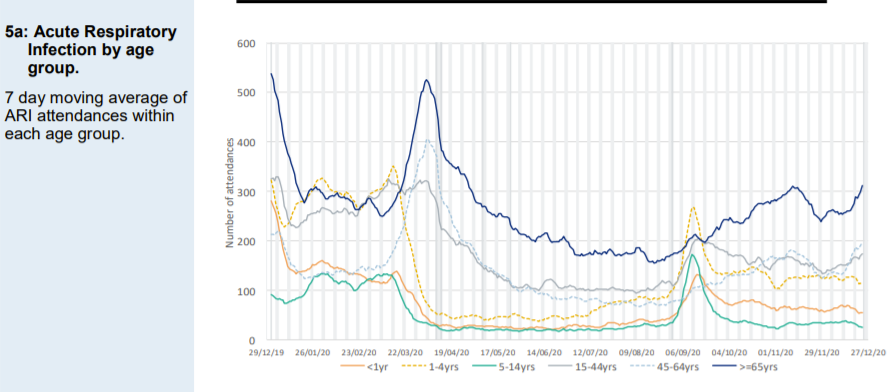
Figure 2: Attendances at Accident and Emergency for an acute respiratory infection (which includes those categorised as Covid-like). Attendance levels at the end of December 2020 are lower than for 2019 (left of graph) for every age group.
How can all of the above be true?
1. Changing biology
The nasopharynx can be home to a number of viruses and bacteria which are either innocent bystanders or the source of illness. However, in the same way as an ecosystem can only sustain a certain number of predators, there is competition between these microorganisms.
Much has been made of the lack of influenza diagnoses this year and the reasons for that remain a puzzle. One possibility is that SARS-CoV-2 has out-competed influenza.
What is little understood is how often respiratory infections can be identified in hospitalised patients. This study, from Spain, showed that testing of the recently deceased elderly identified a respiratory virus in 47% of them and 7% of them had a positive coronavirus test. However, only 7% of these patients had been diagnosed as having a respiratory infection before death.
There are three ways that this could be interpreted:
- Respiratory viruses precipitated other problems e.g. myocardial infarctions that then led to death (and has previously been a massively underdiagnosed contributor to death that we have managed to live with)
- Patients who are very ill and dying are highly susceptible to respiratory infection
- Respiratory viruses are innocent bystanders present at death i.e. not contributing to the underlying cause of death
Because we have never routinely tested for respiratory viral infections in such volumes previously, we do not know what we would have found previously had we done so.
The significance of finding a respiratory virus in the dying is therefore uncertain and given the lack of excess deaths we should conclude that one or more of the three scenarios above must also apply to Covid.
If Covid has become the dominant respiratory virus this year, then identifying it in a significant number of deaths from other causes should not be a surprise to us. If it has no impact on excess mortality, with people dying this year who would otherwise have died, then placing the finger of blame on Covid is of little importance in terms of NHS and broader societal impact.
2. Misdiagnosis
There are two ways in which Covid cases and deaths have come to dominate this winter. As described above, a number of cases and deaths, which previously may have been associated with other viruses that were undiagnosed, are now being correctly diagnosed as associated with Covid. The second way is that our diagnosis of Covid has become dependent on faulty testing, and misdiagnosis is taking place. Evidence for the latter is clearest in the deaths data.
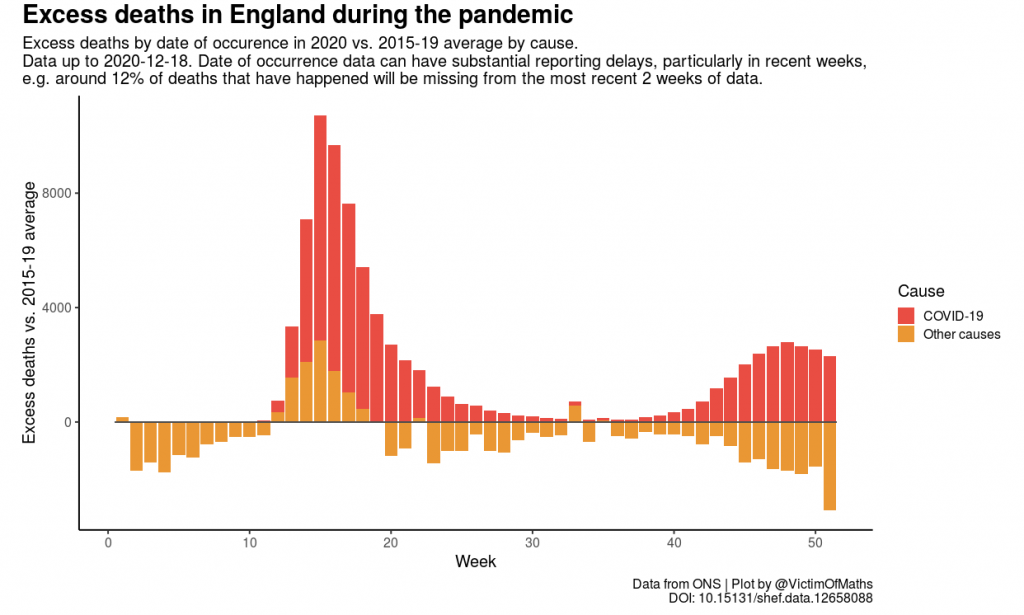
Figure 3 Spring excess Covid deaths were accompanied by excess non-Covid deaths as we restricted access to healthcare. However, every increase in autumn excess Covid deaths has been mirrored by a fall in non-Covid deaths.
The fact that the rise in Covid labelled deaths has been mirrored by a fall in non-Covid labelled deaths (figure 3) means that Covid appears to be behaving in a similar way to the viruses in the Spanish study, and if we were not testing for it, then deaths would have been attributed in the usual way.
3. Bed Management Crisis
Hospitals are in crisis at the moment. That is undeniable. However, the cause may not be what it seems. Total hospital occupancy is normal or even low for the time of year. However, the NHS undoubtedly faces crises every winter and the reduction in beds available for a growing and ageing population is the core underlying problem (figure 4) from 240,000 in 2000 to under 165,000 in 2019. The figure fell by a further 10,000 beds this year after a reduction in beds to allow for social distancing between patients in hospital.
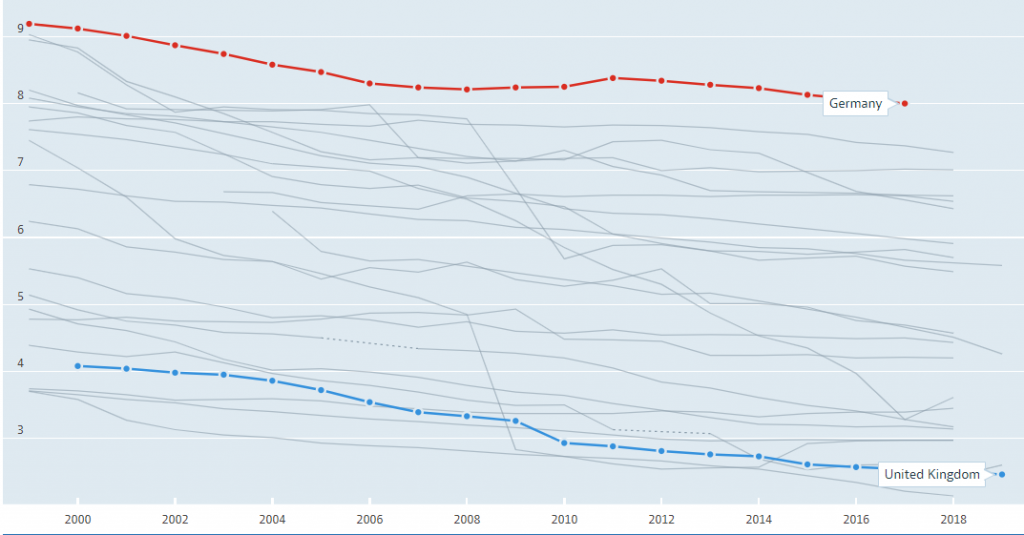
Figure 4 Hospital beds total per 1,000 inhabitants 1999-2019. Data from OECD.
The capacity has not been exceeded even in regions where 30% of patients have a Covid label. Where have all the non-Covid patients gone? There has either been misdiagnosis or mass hospital-acquired infection.
Normally, hospitals work very close to or at capacity in winter. The only way this can be sustained is by a carefully choreographed flow of patients from admission to the wards and then back out. This flow has broken:
- Bed managers, who organise the flow, used to only be concerned with whether a patient was male or female or needed a side room to avoid spread of other infectious diseases. They now have to try and keep patients with a Covid diagnosis separate from those with a suspicion of Covid and those without. This is no small feat in a full hospital.
- In some hospitals patients are not being discharged until their Covid test returns as negative. Clearly returning patients to care homes during the window of infectivity would be a bad idea. Beyond that this policy is not justifiable. Some patients continue to test PCR positive for 90 days after infection.
- PCR testing has led to a staffing crisis as even asymptomatic staff are made to self-isolate for two weeks, with 12% of staff absent when it would normally be 4%
- Staff are having to work in PPE and change it between patients, adding a significant additional burden to an already heavy workload.
If patients are no longer moving smoothly from the Emergency Department to the wards, then the former will quickly fill up giving the impression that the hospital has been overwhelmed. It is easy to see how this could cause a backlog of ambulances unable to drop off their patients.
Conclusion
The NHS is facing a winter crisis which has more to do with bed management and broader policy decisions than Covid itself, although the latter will be contributing as well, because it is winter and we must now regard Covid as an endemic disease (like flu), hopefully to be mitigated to an extent by vaccination.
We may find that the mix of the predominant winter respiratory viruses has changed to have a different character and whether this is permanent remains to be seen. However, the overall impact on healthcare and on the number of lives lost is not, and will not be, that different.
Why then are we reacting in the way we are?













Donate
We depend on your donations to keep this site going. Please give what you can.
Donate TodayComment on this Article
You’ll need to set up an account to comment if you don’t already have one. We ask for a minimum donation of £5 if you'd like to make a comment or post in our Forums.
Sign UpLatest News
Next PostToby’s Newsnight Appearance: A Review