by Dr Clare Craig FRCPath and Jonathan Engler MBChB LLB
Abstract
Evidence of transmission of SARS-CoV-2 from patients who remain asymptomatic (as opposed to pre-symptomatic) is found in a body of numerous meta-analyses. Evidence of asymptomatic transmission has been based on only a handful of instances which themselves are questionable. The existence of transmission of SARS-CoV-2 from asymptomatic individuals has become an accepted truth but the evidence for this phenomenon being anything other than mistaken interpretation of false positive test results is weak. Examination of the underlying data from the most frequently-cited such meta-analyses reveals that the conclusions are based on a surprisingly small number of cases (six in total globally) and, moreover, the possibility that they are all coincidental contacts with false positive results cannot be ruled out. Transmission which is pre-symptomatic is rare and represents a negligible risk to the population. It is questionable therefore whether any of the extensive testing, tracing, isolation and lockdown policies have delivered any worthwhile benefit over and above strategies which seek to advise symptomatic individuals to self-isolate.
Introduction
Many of the world’s economies have been seriously damaged on the basis of alleged evidence that people with no symptoms can spread SARS-CoV-2. It is essential that all such claimed evidence is carefully scrutinised because of the immense and ongoing impact of that claim on public policy making. Much of the early evidence of asymptomatic transmission came from China. Chinese publications appear to be major outliers in the scientific discussion and their contributions are, it is suggested, seriously distorting the available evidence in this area.
Scientific papers from reputable institutions which attempt to summarise the evidence have taken certain Chinese papers at face value. This has arguably resulted in the establishment of a dangerous assumption. The assumption is that there is compelling evidence that people who never have symptoms are capable of spreading SARS-CoV-2 to others.
This paper reviews the evidence that people who are asymptomatic (defined in this paper as not only having no symptoms but also never developing symptoms) are capable of carrying SARS-CoV-2 and infecting others. This must be clearly distinguished from pre-symptomatic – there is evidence that some patients can be infectious for a brief period before developing symptoms.
To the extent that pre-symptomatic cases exist the evidence suggests that they must only account for a very small proportion of transmission and therefore they present a low overall risk. In fact, in one study of 243 cases in total, the maximum transmission from pre-symptomatic individuals was estimated to account for less than 7%1 of transmissions. The secondary attack rate from pre-symptomatic transmission was estimated to be only 0.7% to household contacts in a large meta-analysis of 77,758 traced participants.2 Transmission which is pre-symptomatic is rare and represents a negligible risk to the population. The evidence that asymptomatic transmission exists at all is tissue thin. It is questionable therefore whether any of the extensive testing, tracing, isolation and lockdown policies have delivered any worthwhile benefit over and above strategies which seek to advise symptomatic individuals to self-isolate.
The evidence of transmission of SARS-CoV-2 comes largely from case reports where specific groups of infected individuals have been traced in an outbreak and the transmission routes are then reported. Deducing transmission from outbreak data is not straightforward and assumptions need to be made about which of the contacts caused transmission. This is not an exact science.
Reports of instances of transmission are important and interesting enough to publish but on their own they are merely anecdotal. Anecdotal evidence alone is no basis on which to formulate public policy. To draw conclusions about transmission it is necessary to gather multiple instances, ideally all, of such anecdotes and weigh them all up as evidence reaching a conclusion based on all the anecdotes together, i.e. in a formal meta-analysis. However, meta-analyses suffer from the flaw that they can be hugely skewed by larger data sets.
There have been numerous meta-analyses attempting to answer the question of whether SARS-CoV-2 can be spread by people who are asymptomatic. These have been published by distinguished scientists from a range of respected institutions. To reach a conclusion, the evidence from all the papers included in a meta-analysis is summarised. However, only by going back to the underlying data can we understand what the real risk of asymptomatic transmission is. We identified the most frequently-cited such published papers and examined the data underlying their conclusions. The bulk of the Chinese literature on asymptomatic spread were excluded by these meta-analyses because they did not meet the quality criteria specified by the authors.
Results
Across the studies reviewed, a total of seven instances suggestive of asymptomatic transmission were identified, these being:
- In Italy, two asymptomatic cases allegedly passing the virus onto two others.
- In Brunei, two asymptomatic cases allegedly passing the virus onto three others.
- In China, two asymptomatic cases allegedly passing the virus onto two others
Notwithstanding the small numbers, these case reports, given undue prominence in papers written by respected authorities, appear to have played a major role in the evolution of lockdown and test and trace strategies adopted by most countries over the past nine months.
Findings from each of the four papers examined:
- Yanes-Lane et al, from McGill University in Quebec,3 found 6,137 studies examining the issue of asymptomatic SARS-CoV-2 transmission and rejected all but 28 of them (due to small size, or inadequate methodology). Only 5 included reports of asymptomatic transmission and were listed in table 5 (figure1). As it happened, these were all reports of pre-symptomatic transmission. The study by Park et al. included four asymptomatic cases and four pre-symptomatic cases (hence these were listed separately in the table reproduced below) and there was no evidence of transmission from any of them.
Despite the only evidence of asymptomatic transmission (all of which were pre-symptomatic) being from China, an average was taken, concluding:
Among five transmission studies, 18 of 96 (18.8%) close contacts exposed to asymptomatic index patients were COVID-19 positive.
That sounds high until you consider that the sample size is just 13 index cases, all of which were pre-symptomatic cases, transmitting to 18 people across five studies, none of which were outside of China.
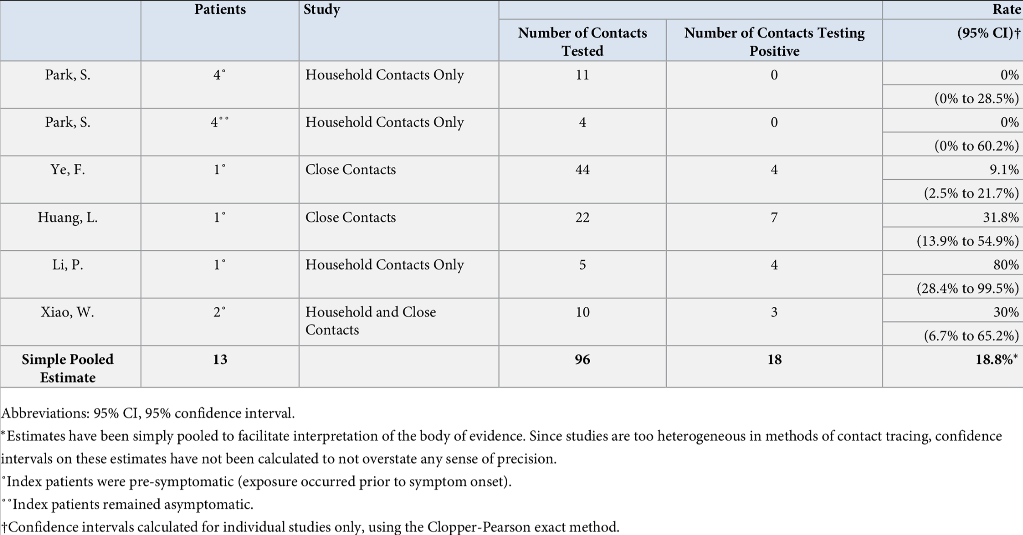
Figure 1: Table 5 of the Yanes-Lane et al paper. The two references to the study by Park et al. were from South Korea and the remainder from China
- Buitrago-Garcia et al., from the University of Bern,4 found 688 studies on asymptomatic and pre-symptomatic COVID-19 and 5 which commented on transmission. Rather than draw conclusions on the likelihood of asymptomatic transmission they compared the risk from asymptomatic with that from symptomatic transmission. Included were three studies showing asymptomatic transmission, one from Brunei and two from China and two showing no transmission from Taiwan and South Korea.
As regards the Brunei study, which will be discussed further below, it is not clear how the numbers in this table were derived from the paper which reported on 71 patients and 1755 total contacts. Of these there were four instances of pre-symptomatic transmission and two incidences of true asymptomatic transmission, accounting for 11 and 3 cases respectively.
The two Chinese papers each only claimed a single patient had contracted COVID-19 from an asymptomatic person. Luo et al. studied 4950 people up until March 6th 2020 who were quarantined in Guangzhou.5 They had up to 6 PCR tests each with a mean of 2.4. From all this testing they only claim to have found eight asymptomatic individuals. They report on a single asymptomatic individual spreading SARS-CoV-2 but do not make it clear whether they were pre-symptomatic nor what symptoms the secondary case had. Nevertheless this has been interpreted as evidence of asymptomatic spread.
Zhang et al.6 also reported from Guangzhou and two of the authors on this paper are the same as the Luo paper. Given the shared authorship, the possibility that this single case of probable pre-symptomatic transmission was the same individual reported in the Luo paper cannot be ruled out. This paper reported on the first 359 COVID-19 diagnoses and their 369 contacts up to 15th March 2020. Importantly, the single case of asymptomatic transmission was from a man to a male colleague who also remained asymptomatic (i.e. tested positive only, without symptoms). Given that the person said to have contracted COVID-19 had no symptoms this cannot be regarded as adequate evidence for transmission of disease.
Every test has a risk of producing an erroneous positive result, a false positive. A false positive rate of 1% would be very respectable for PCR testing and it is hard to find reports of false positives for PCR at lower rates than this. The UK Government’s own estimate for false positive results, based on other PCR tests for other viruses in non-pandemic situations is a median of 2.3% (range 0.8-4.0%),7 so a rate of 1% might be regarded as improbable given the speed of roll out of the test and other observations.
It is not clear how many of the people tested remained asymptomatic throughout, however, when testing 369 contacts a reasonable false positive rate of 1% would result in three to four false positive diagnoses. Given that all the contacts were tested because they had relationships with those that tested positive, any false positives found would by definition have been a contact with a case.
It is worth pointing out at this early stage that studies based on single figures such as this are no proper basis for policies affecting hundreds of millions of lives predicated on the questionable assumption that true asymptomatic transmission can regularly occur. It must be repeated that both studies so far contained a bare handful of alleged transmission without symptoms.
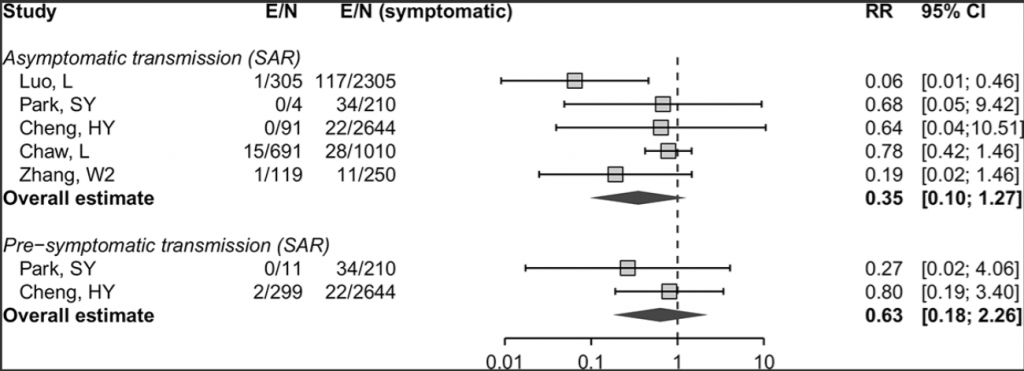
Figure 2: Figure 3 of the Buitrago-Garcia paper. The publications originated from: Luo and Zhang – China; Park – South Korea; Cheng – Taiwan; Chaw – Brunei. The first column shows the fraction of contacts contracting COVID-19 from an asymptomatic / pre-symptomatic individual and the second column shows the fraction contracting from symptomatic individuals in the same study.
- Wee Chian Koh et al.8 also put great weight on the Brunei study but use different numbers for the same work. It is not clear why. No other cases of asymptomatic transmission were included in this analysis.
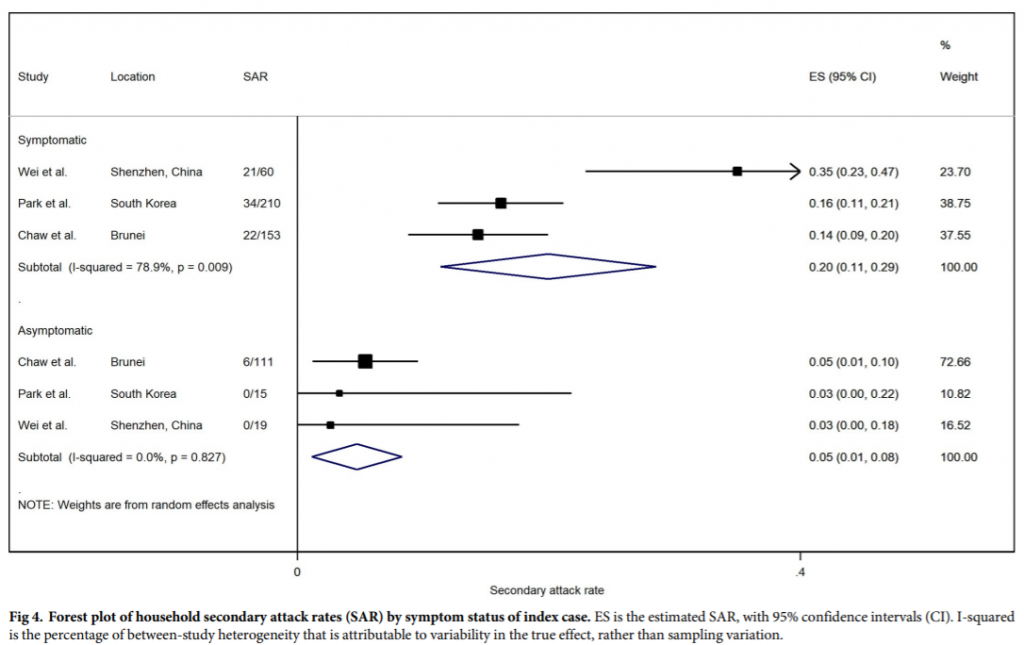
Figure 3: Figure 4 of the Wee Chian Koh paper. The columns labelled SAR shows the fraction of contacts that contracted COVID-19 in each study.
- The Lancet pre-published a meta-analysis by Byambasuren et al.9 who found five studies from 571 met their minimum methodological criteria, two of which reported asymptomatic transmission. The first was a study of 4,950 contacts in Guangzhou5 who were quarantined.
The second study quoted was a Nature paper10 on an Italian study that did not actually report on asymptomatic transmission. Instead they extrapolated from the results of PCR testing to deduce how much virus was present and assumed that high viral loads on testing equated to a higher risk of transmission.
The Italian study reports on numerous asymptomatic ‘cases’ and goes on to propose lines of ‘transmission’ concluding that two asymptomatic people were infected by two other asymptomatic people, out of 2,812 tested initially and then 2,343 tested again two weeks later. In the first round of testing, 29 of the 73 positives were asymptomatic. A respectable false positive rate for the testing performed would be 1%, therefore, it is reasonable to expect at least 28 false positive results when testing 2,812 people. It is therefore fair to conclude that all the 29 asymptomatic positives in the first round were most likely false positives.
In the second round of testing at the beginning of March, there were 18 asymptomatic people who tested positive out of 2,343 people tested. Likewise, these were most likely false positive results. Deducing chains of transmission based on a high risk of material numbers of false positive results is bad science.
Brunei study
Due to the prominence afforded to it by those justifying policy choices on the basis of asymptomatic transmission, it is worth focusing particularly on the study by Chaw et al.,11 from Brunei, which reported on a large outbreak which started with people who attended a religious festival and subsequently developed COVID-19. There were apparently six people who had no symptoms initially (of which, crucially for our purposes, two were asymptomatic throughout), but who allegedly spread SARS-CoV-2 from this outbreak to other people who did not attend.
There are two aspects of this paper that weaken this evidence:
- Weak definition of a case (it appears any symptom of any severity was adequate)
- High possibility of false positive test results
The same group published a further paper12 where they describe two of the incidences of asymptomatic spread in more detail. First there was a 13 year old who attended the festival who is said to have spread SARS-CoV-2 to their teacher. The basis for this conclusion was that the teacher “had a mild cough for one day” along with a positive test.
The second was a father who remained asymptomatic but whose wife briefly had a runny nose and whose baby had a mild cough on one day.
In both these papers no details are given as to the testing protocols. A final paper13 reports on the first 135 cases to be diagnosed in Brunei. Thirteen of these first cases were asymptomatic. Without knowing the false positive rate of the testing and the numbers tested it is not possible to establish the significance of these asymptomatic ‘cases’.
Dr Chaw, the lead author of the Brunei transmission paper, was initially very helpful in correspondence with the authors. Thorough testing (with whole genome sequencing) was carried out for the first few cases but otherwise, as in the rest of the world, a positive PCR was considered sufficient. She was unaware (as are almost all doctors diagnosing COVID-19) of the criteria used in their laboratory to declare a test positive and has not responded to a request for further clarifications.
It is therefore at least arguable that the asymptomatic diagnoses in spring were all due to false positive test results. No testing system is perfect. Failure to acknowledge this and misinterpretation of positive results in patients with no symptoms has been hugely damaging. What is undoubtedly true is that the policy-making of governments responsible for the lives of billions of people around the world may in part be influenced by the dangerous assumption that there is persuasive evidence of asymptomatic transmission of SARS-CoV-2. It is far too soon to make that assumption and the evidence underpinning it is, at best, circumstantial.
Chinese Publications
During the early stages of the pandemic, many papers were published from China suggesting the frequency of asymptomatic transmission and its importance in SARS-CoV-2 spread. Notwithstanding that most of these were excluded by authors of the meta-analyses examined herein, their frequency, and the prominence afforded to these studies laid the foundations for this phenomenon being given undue salience in the scientific literature. This is despite asymptomatic transmission never having been a feature of previous respiratory pandemics and despite large studies showing no evidence of asymptomatic transmission outside of China. The reader will no doubt readily understand the challenges of relying heavily on the output of a highly controlled regime with an active interest in destabilising the economies and political systems of other countries.
It is notable in fact, that in what would seem to represent an abrupt volte face by the CCP, a further (presumably Government-approved) study from China was recently published14 which entirely contradicts the earlier conclusions regarding the phenomenon of asymptomatic transmission, which had been driven by Chinese data in particular, early in the pandemic.
Some might conclude that that study lacks the credibility one might expect for a paper published in Nature; it is claimed, for example, that they PCR tested 92% of Wuhan’s population (~10m individuals) over a 19-day period at the end of May, and found just 300 positive PCR tests, implying a false positive rate of no greater than 0.003%. Further, it is claimed that while 100% of the 300 PCR positive cases were asymptomatic, there were zero symptomatic PCR positive cases out of ~10m tested during a period only a few weeks after the epidemic had peaked in Wuhan.
If this seems incredible, then surely that has serious implications for the way in which earlier studies from China – data from which formed a significant part of the worldwide evidence base for asymptomatic transmission – should be regarded.
We do not claim to have included every meta-analysis that has been written on this subject, however the studies quoted here do represent the ones most frequently cited in support of the phenomenon of asymptomatic transmission. It is clear that these meta-analyses consist of highly questionable studies taken at face value.
What is an asymptomatic ‘case’?
Attempts to understand the phenomenon of asymptomatic COVID-19 have resulted in reports of asymptomatic cases accounting for between 4%15 and 76%16 of COVID-19 cases. An implausibly wide range such as this is evidence of an attempt to measure a phenomenon that is not a characteristic of the disease, in contrast to features such as symptoms.17
For completeness, it should be acknowledged that SARS-CoV-2 can be detected in asymptomatic people. They can test positive for SARS-CoV-2 virus and viable virus can be cultured from these individuals. In the past, this scenario of having virus onboard in the absence of symptoms would have been referred to as ‘immunity’ or else been attributed to a testing error. Someone with immunity cannot prevent virus entering their respiratory tract, however, when that occurs, their immune system invariably deals with the attack and they remain oblivious and have no symptoms.
It is for the above reasons that whereas reports of high numbers of asymptomatic cases, for example in cruise ship outbreaks,18 are cited as evidence of asymptomatic transmission, we contend that a more plausible explanation for most of these observations is in fact prior immunity. Several prominent papers made unsupported claims of asymptomatic transmission simply because they had found asymptomatic individuals who had tested positive during an outbreak.19 Asymptomatic transmission can only be proven by clear evidence that a patient has been infected by SARS-CoV-2 from a person who was asymptomatic. Finding positive test results in asymptomatic individuals is not evidence of transmission.
Normally, someone who is immune would not be considered to have a disease or to be a ‘case’ in an epidemic. It is only in the current crisis that mass testing of asymptomatic individuals has resulted in the detection of virus in asymptomatic individuals. Considerable further work would be required before it could be confidently stated that asymptomatic positives could ever transmit infection.
There is certainly no evidence of immune individuals (as historically defined) transmitting other respiratory viruses. Viral replication and shedding20 is a prerequisite for viral spread and in immune individuals virus is prevented from growing exponentially so the viral numbers remain low. Attempts to deduce viral numbers present from the quality of the test results (viral load on PCR) is overinterpretation. However, no assumptions have been made here. The evidence as to whether immune individuals can transmit SARS-CoV-2 virus must come from actual studies that show, or do not show, real world transmission.
Aside from reported studies of transmission, those leading on the contact tracing response might have useful experience on the likelihood of transmission. Maria Van Kerkhove, head of the World Health Organization’s emerging diseases and zoonosis unit21 stated at the beginning of June:
Countries doing very detailed contact tracing …[are]…following asymptomatic cases and following contacts and they’re not finding secondary transmission onwards. It’s very rare. Much of that is not published in the literature.
It is worth noting that an early frequently-cited claim22 of pre-symptomatic transmission has been discredited23 after it was revealed that the authors did not interview the patient accused of spreading infection who was in fact symptomatic at the time of transmission. This has not been retracted.
Conclusion
Medical evidence can be difficult to summarise. The medical literature is huge and constantly growing and it is impossible to say with confidence that everything of relevance has been read. This in itself can cause problems: it is difficult to say confidently that there is zero evidence for something. That is why this paper has been careful only to claim that it is a dangerous assumption to believe that there is persuasive, scientific evidence of asymptomatic transmission.
It could be argued that adherence to ‘precautionary principle’ demands that public policy assumes the existence of significant asymptomatic transmission, in order to be ‘better safe than sorry’. However, given the increasing evidence of the harms caused by such policy, at some point the burden of proof must surely shift onto those advocating extreme measures. There is increasing evidence of harm from interventions, for example: there are over 100 excess deaths at home per day in England; accident and emergency attendances are well below normal levels; excess mortality in the under 60s is significant; prescriptions for heart medications are well below normal and there are excess deaths resulting from heart disease.
The Chinese Communist Party24 has mandated that all scientific literature on COVID-19 must first be approved by the Chinese Ministry of Science and Technology or Ministry of Education before publication. This political interference means that all Chinese scientific publications should be regarded as suspect.
Additionally, there is an unknown but real risk of publication bias because studies, such as the many early Chinese ones showing asymptomatic transmission may find a quicker route to publication, whereas an article reporting the opposite may risk not having commensurate perceived salience when the editors of a journal are choosing papers for publication. It is important to note that much of the evidence relating to modes of transmission was shared via pre-prints prior to publication, and decisions had to be taken based on evidence that had not been peer reviewed, as is inevitable in a pandemic situation.
A claim is not being made that every meta-analysis has been included here and this article may be updated in due course with more data as it becomes available.
However, after examination of the most frequently-cited papers in this area available to date, we are struck by the paucity of persuasive evidence of anything but the most minor of symptoms resulting from supposed asymptomatic spread; most or all of which could be misdiagnoses and in any event are at no more than anecdotal level. There is no evidence, outside of China, that anyone has developed even moderate COVID-19 based on true asymptomatic spread, as opposed to pre-symptomatic spread.
I/we have read and understood the BMJ Group policy on declaration of interests and declare the following interests: None
1 Wei WE, Li Z, Chiew CJ, et al. Presymptomatic Transmission of SARS-CoV-2 – Singapore, January 23-March 16, 2020. MMWR Morb Mortal Wkly Rep 2020;69:411–5.
2 Madewell ZJ, Yang Y, Longini IM Jr, et al. Household Transmission of SARS-CoV-2: A Systematic Review and Meta-analysis. JAMA Netw Open 2020;3:e2031756.
3 Yanes-Lane M, Winters N, Fregonese F, et al. Proportion of asymptomatic infection among COVID-19 positive persons and their transmission potential: A systematic review and meta-analysis. PLoS One 2020;15:e0241536.
4 Buitrago-Garcia D, Egli-Gany D, Counotte MJ, et al. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: A living systematic review and meta-analysis. PLoS Med 2020;17:e1003346.
5 Luo L, Liu D, Liao X-L, et al. Modes of Contact and Risk of Transmission in COVID-19: A Prospective Cohort Study 4950 Close Contact Persons in Guangzhou of China. papers.ssrn.com › sol3 › paperspapers.ssrn.com › sol3 › papers. 2020. doi:10.2139/ssrn.3566149
6 Zhang W, Cheng W, Luo L, et al. Secondary Transmission of Coronavirus Disease from Presymptomatic Persons, China. Emerg Infect Dis 2020;26:1924–6.
7 Mayers Carl And. Impact of false-positives and false-negatives in the UK’s COVID-19 RT-PCR testing programme. 2020.
8 Koh WC, Naing L, Chaw L, et al. What do we know about SARS-CoV-2 transmission? A systematic review and meta-analysis of the secondary attack rate and associated risk factors. PLoS One 2020;15:e0240205.
9 Byambasuren O, Cardona M, Bell K, et al. Estimating the extent of asymptomatic COVID-19 and its potential for community transmission: Systematic review and meta-analysis. Official Journal of the Association of Medical Microbiology and Infectious Disease Canada 2020;:e20200030.
10 Lavezzo E, Franchin E, Ciavarella C, et al. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of Vo’. Nature 2020;584:425–9.
11 Chaw L, Koh WC, Jamaludin SA, et al. Analysis of SARS-CoV-2 Transmission in Different Settings, Brunei. Emerg Infect Dis 2020;26:2598–606.
12 Wong J, Jamaludin SA, Alikhan MF, et al. Asymptomatic transmission of SARS-CoV-2 and implications for mass gatherings. Influenza Other Respi Viruses 2020;14:596–8.
13 Wong J, Chaw L, Koh WC, et al. Epidemiological Investigation of the First 135 COVID-19 Cases in Brunei: Implications for Surveillance, Control, and Travel Restrictions. Am J Trop Med Hyg 2020;103:1608–13.
14 Cao S, Gan Y, Wang C, et al. Post-lockdown SARS-CoV-2 nucleic acid screening in nearly ten million residents of Wuhan, China. Nat Commun 2020;11:5917.
15 Zhou X, Li Y, Li T, et al. Follow-up of asymptomatic patients with SARS-CoV-2 infection. Clin Microbiol Infect 2020;26:957–9.
16 Petersen I, Phillips A. Three Quarters of People with SARS-CoV-2 Infection are Asymptomatic: Analysis of English Household Survey Data. CLEP 2020;12:1039–43.
17 Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 Infections and Transmission in a Skilled Nursing Facility. N Engl J Med 2020;382:2081–90.
18 Ing AJ, Cocks C, Green JP. COVID-19: in the footsteps of Ernest Shackleton. Thorax 2020;75:693–4.
19 Oran DP, Topol EJ. Prevalence of Asymptomatic SARS-CoV-2 Infection : A Narrative Review. Ann Intern Med 2020;173:362–7.
20 Kutter JS, Spronken MI, Fraaij PL, et al. Transmission routes of respiratory viruses among humans. Curr Opin Virol 2018;28:142–51.
21 WHO Says Covid-19 Asymptomatic Transmission Is ‘Very Rare’. 2020
22 Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N Engl J Med 2020;382:970–1.
23 Study claiming new coronavirus can be transmitted by people without symptoms was flawed. 2020
24 Silver A, Cyranoski D. China is tightening its grip on coronavirus research. Nature 2020;580:439–40.










Donate
We depend on your donations to keep this site going. Please give what you can.
Donate TodayComment on this Article
You’ll need to set up an account to comment if you don’t already have one. We ask for a minimum donation of £5 if you'd like to make a comment or post in our Forums.
Sign UpLatest News
Next PostLatest News