by Dr Clare Craig FRCPath

Outbreaks of Covid in care homes appear to have spiked in September in the UK. Does this mean we will see a resulting spike in deaths? This article explores the possibility that a significant number of the alleged outbreaks in care homes could be based on false positive test results. The continuing absence of systemic cross-checking of alleged positive results against established clinical and diagnostic evidence such as loss of smell and distinctive CT chest scans remains deeply disappointing. At an absolute minimum, anyone who receives an alleged positive Covid result should be retested from scratch.
The percentage of tests carried out in the community that were reported as positives reached a steady state over the summer at 0.8 per cent of tests. Reaching a steady state like this over a period of weeks is suggestive of having arrived at the baseline false positive rate. Similar figures have been used by SAGE. Matt Hancock has said the figure is “less than one per cent”.
The argument in support of the idea that a significant proportion of national UK Covid diagnoses in July and August 2020 were actually due to false positives is provided in a separate blog post. This paper addresses the narrower issue of alleged outbreaks in care homes.
This is how a false positive ‘outbreak’ in care homes could conceivably happen:
Step 1
Start by testing the entire UK population of care home residents every 28 days for Covid. There are currently more than 460,000 people who are being systematically tested in this way in 17,000 care homes. With a 0.8 per cent false positive rate this will result in more than 3600 randomly distributed false positive results every month. These false positives are treated as if they are real cases. When two positive results occur in residents who have been in direct contact, an official outbreak is declared. Mass testing of this kind, with a constant false positive rate, would be sufficient for fake Covid ‘outbreaks’ to be officially declared at a steady monthly rate in random care homes all around the country. Indefinitely. This would happen without any actual Covid infections occurring at all.
Step 2
Once an outbreak has been declared in a particular home, residents of that care home are required to be tested at least every week (and sometimes as often as every 4 days). Let us consider, as a case study, a hypothetical care home with 40 residents (which happens to be an average number according to this report).
We will call our imaginary care home ‘Everglades’. After the outbreak is declared, Everglades test all their residents at least every week. As a direct result of the 0.8 per cent false positive rate, a new false positive case will be diagnosed in Everglades on average after every three rounds of further testing. If we include staff testing, then it would be even more frequent (because the average number of staff is 47 according to the same report).
When a further false positive result occurs, this will give the mistaken impression that the ‘outbreak’ is continuing in Everglades, even though no one in the home has had Covid at all. The same will happen in many other similar care homes where an ‘outbreak’ has been declared.
Step 3
Current policy is that an outbreak is not declared to be over until a full 28 days has passed with no new positive tests in that particular care home. To end an outbreak, each of the 40 individuals in Everglades must avoid the 0.8 per cent false positive rate on four occasions (without even considering tests on staff). This is assuming testing is carried out weekly – it would require seven lucky outcomes for each resident and staff member if testing is carried out every four days.
Consequently, if testing is weekly, there is only a 30 per cent chance that the non-existent ‘outbreak’ in Everglades will be declared to have ended after 28 days has passed. Over 70 per cent of the time, another false positive test will restart the 28-day clock and perpetuate the mistaken belief that an outbreak of Covid has occurred when there is no Covid outbreak.
These statistical realities mean that false positive results across care homes will continue to accumulate over time. Of course, larger care homes will be particularly prone to having fake outbreaks and will find it even more difficult to end them. After four months of weekly testing, a quarter of affected care homes with 40 residents could well still be stuck in their fake outbreak. The self-perpetuating statistically inevitable nightmare will have restarted the clock time and time again. The other three quarters are likely to have escaped after four months until their next unlucky false positive result. This is Kafkaesque.
Furthermore, all the residents affected may then think they are immune because they will mistakenly think that they have had Covid. They and their carers may start to alter their behaviour with potentially disastrous effects if a real outbreak occurs. Some residents may think they have caught Covid more than once as time goes by and the random false positive results keep coming. The terror and confusion this situation could cause amongst elderly people is a genuine disgrace.
Step 4
The fake outbreaks will inevitably feed through into the data on Covid deaths. A third of care home residents die every year which is equal to 3 per cent dying every month. Having mistakenly labelled multiple patients as having Covid, those that die within a month of ‘diagnosis’ will be recorded as having died of Covid because all deaths within 28 days of a positive result are presumptively labelled as having been caused by Covid, regardless of the clinical reality. As a pathologist, I find this kind of careless data gathering deeply frustrating. It is also potentially misleading on many levels.
Mass testing is leading to ‘outbreaks’
Mass testing in care homes, as described above, was started in July and was due to reach all such residents by September. Mass testing using a test with a false positive rate even as low as 0.8 per cent is a recipe for trouble. Public Health England’s guidelines were to test every care home resident (at least 460,000 people) every 28 days. This policy is questionable unless treated merely as a screening tool where subsequent confirmatory retesting is conducted de novo or where independent clinical evidence independently supports a positive diagnosis of Covid.
An attempt was made to try to avoid labelling hundreds of care homes as having outbreaks due to the known problem of false positives. It was mandated that an outbreak can only be confirmed where direct contact can be demonstrated between two residents who have both tested positive. The better policy option would have been mandatory retesting of all alleged positive Covid patients. The problem with the ‘direct contact’ rule is that the small size of many care homes means that direct contact could easily have happened by chance in such homes.
Across averaged sized care homes, like our imaginary Everglades, purely random allocation of positive results would statistically result in roughly a 1 in 4 chance of having one positive Covid test result and 1 in 25 chance of having two or more positive test results every month. Based on a random distribution of false positives to average sized cares homes, roughly 690 care homes would have two residents test positive every month.
There were 228 official outbreaks in the first week of September alone (see Figure 1). This was despite the care taken to ensure only direct contact between two alleged Covid patients could lead to the formal declaration of an outbreak. There is no way of knowing how many of these ‘outbreaks’ were generated by false positive test results due to the total failure to double check, by retesting, or clinically cross-check positive test results by requiring recognised independent diagnostic evidence.
The September spike now appears to be fading. Some, even many, of these may have been real outbreaks that are now slowing down. However, the decrease may have partially resulted from wider pressures on testing in September reducing the number of false positives found in care homes because results from testing were delayed significantly – but the data on this is opaque so no conclusions can be drawn yet. It is unconscionable that we cannot be sure how many of these official outbreaks were genuine.
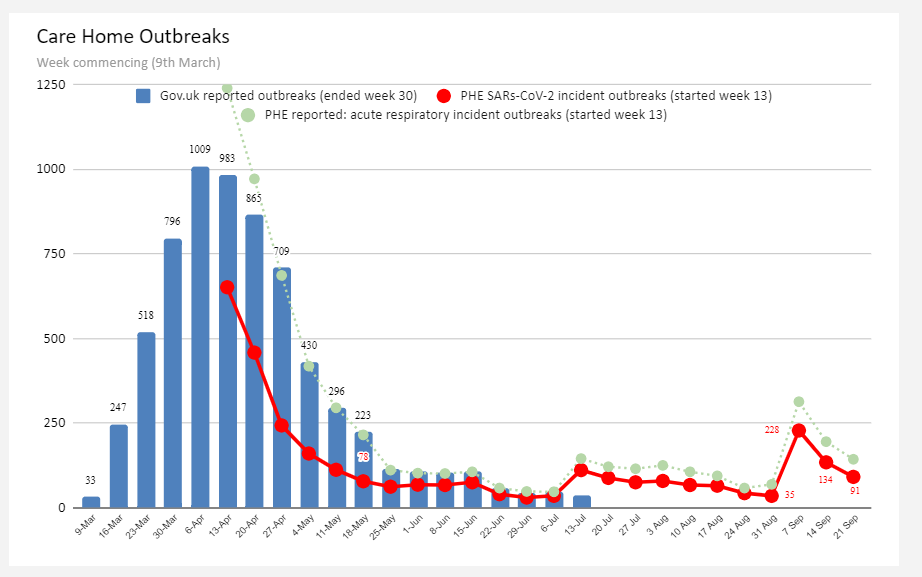
Figure 1 is a graph from Prof Carl Heneghan showing government reported Covid outbreaks in red. The green line shows all acute respiratory infection outbreaks including Covid.
There have been at least 900 official outbreaks in care homes since July. The impact of these can be estimated based on a few assumptions. Say that 4 per cent of care homes have an outbreak currently, which is not an unreasonable percentage to assume. With that starting assumption, we can calculate that 4 per cent of the care home population equates to roughly 18,000 residents. The much higher-frequency testing of this cohort will therefore result in about 150 false positive diagnoses every week or roughly 600 a month.
Misdiagnosed patients can lead to distorted deaths data
If 600 nursing home residents are labelled as having Covid every month and 3 per cent of all nursing home residents die every month, then the random deaths of these patients within 28 days of them being labelled as having had Covid will be wrongly called Covid deaths. This translates to roughly 18 false positive Covid deaths every month.
These numbers will rise over time as more outbreaks are declared whilst simultaneously the declaration of the end of an existing outbreak is statistically fraught with difficulty, as we have seen. Assuming current policies are maintained then by Christmas, with accumulating fake outbreaks, we can statistically expect over 25,000 care home residents to be part of a fake outbreak in more than 1,000 homes. Based on the same calculations as above, these homes will account for over 26 deaths being wrongly attributed to Covid per month from fake ‘outbreaks’ because natural deaths will be wrongly attributed to Covid.
In addition to these 26 deaths from higher-frequency screening of fake ‘outbreaks’, the remainder of the care home population will still be screened every 28 days. This screening will result in thousands of further false positive diagnoses every month and the standard 3 per cent deaths per month from this cohort will result in 100 further wrongly labelled deaths per month. Finally, 95 false positive deaths could be expected per month when 30,000 tests were used screening the entire inpatient hospital population because a fairly steady proportion of the patients labelled with false positive Covid die from the problem that brought them to hospital in the first place. Inpatient testing has now increased to 70,000 tests a day. If patients are being tested twice the number of false positive deaths attributable to this screening will double.
Taken together, these errors could cumulatively account for around 50-70 deaths wrongly attributed to Covid per week from care homes and hospitals alone.
There is no evidence as to whether care homes with a declared outbreak are receiving inferior healthcare as a result, but since 3% of such residents of such homes die per month, anything that could result in a reduction in immediate and vital healthcare would be a serious cause for concern.
European comparators
Despite the striking rise in case numbers, death rates in Europe have remained minimal except in France and Spain. All countries are trying their best to contain the spread of what at first sight appears to be a second outbreak of Covid and carrying out screening testing in care homes is a common strategy.
Given the rise in deaths in Spain and France, it would be interesting to know if they have started screening care home residents in a way that looks similar to the UK. This may also have resulted in deaths being wrongly attributed to Covid if they have also failed to take steps to double check alleged positive cases.
The true death rate, which may still be significant, can only be observed once these false positive deaths are removed from the data both here and elsewhere in the world.
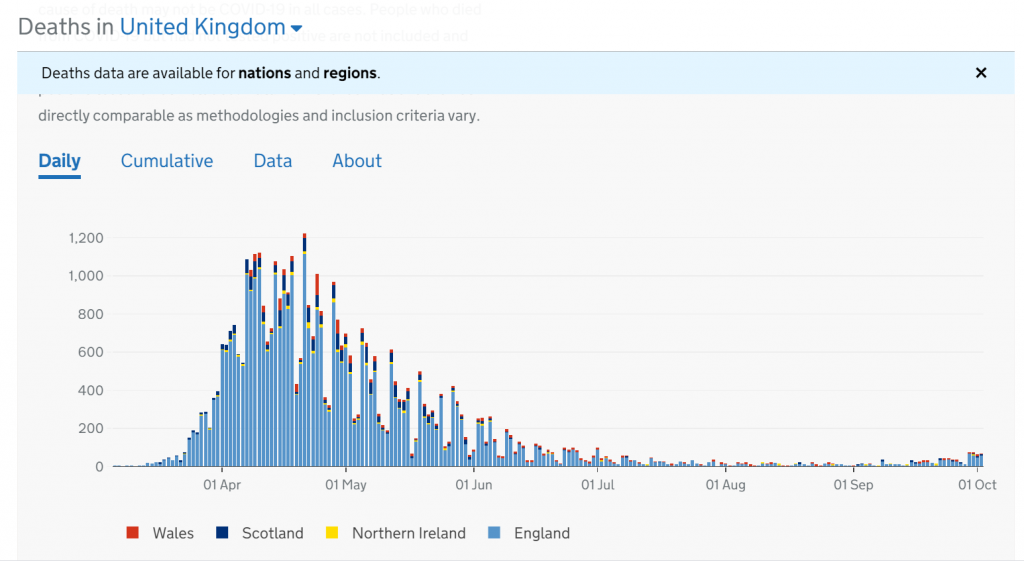
Figure 2 shows government recorded Covid deaths by date that the diagnosis was reported.
Data beyond death statistics may also be distorted due to misdiagnoses
As well as the distorting effect of false positives on the death statistics, a similar inference may be drawn about the data for total hospital and for intensive care admissions generally. Screening hospital patients on admission will result in a fraction being labelled as Covid due to false positive results. Worse still, the care home population being labelled as Covid positive are elderly, vulnerable and prone to respiratory infections at this time of year anyway so these patients may well present in hospital with symptoms consistent with Covid despite not having Covid. This could stretch the resources and facilities of hospitals unnecessarily if these cases are in fact false positives as well as skew the statistics on the alleged spread of Covid.
Diagnosing false positive test results as cases in care homes has the effect of increasing workload for the homes, instilling fear in residents, staff and relatives and artificially boosting the case numbers. Large numbers of elderly, frail patients may well be wrongly labelled as having Covid. When this is combined with their high risk of dying anyway, it is possible that multiple deaths could be wrongly attributed to Covid. The impact of these false positive Covid cases in care homes could easily have skewed the overall data on deaths from Covid, impacting negatively on policy making.
Suggested policy solution
All that is needed to distinguish real Covid outbreaks from fake ones is for the initial allegedly positive ‘cases’ to be retested from scratch with a different test kit. Testing needs to be carried out with care. A true Covid outbreak should only be declared when accompanied by clinically specific symptoms and signs. For example, 97 per cent of people suffering a sudden loss of their sense of smell in the spring had caught Covid. In addition, loss of smell is present in 65 per cent of real Covid cases and statistically would therefore be present in 96 per cent of true outbreaks of more than three individuals. Likewise, characteristic chest CT findings are also highly specific, even in mild cases.
The continued failure to cross check alleged Covid outbreaks using established clinical evidence of genuine Covid symptoms is a serious policy failure. The potentially material effect that the inflated figures relating to care home deaths may have had on public policy making means it is imperative that the evidence that such deaths have in fact been caused by Covid is watertight.










Donate
We depend on your donations to keep this site going. Please give what you can.
Donate TodayComment on this Article
You’ll need to set up an account to comment if you don’t already have one. We ask for a minimum donation of £5 if you'd like to make a comment or post in our Forums.
Sign UpLatest News
Next PostLatest News