Like those famous Japanese soldiers still fighting World War II on a remote island decades after everyone else had ended hostilities, a minority of healthcare settings in the U.K. enter 2024 with local managers attempting to insist that visitors and patients wear “face coverings” into a fourth consecutive year. For allowing the dogged persistence of this superstitious practice we can thank the U.K. Health Security Agency (UKHSA), despite the fact its own boss, Dame Jenny Harries, made a series of incredible admissions about the value of masking at the recent Covid Inquiry. There was no solid proof masks ever slowed the spread of Covid, Harries explained. The advice to the public to make their own “face coverings” was “ineffective”. Worst of all, by creating a false sense of security, masking may have actually made things worse, she said. Of course, if you’d been paying attention, you’d know Harries was really just coming full circle.
On March 11th 2020, in her previous role as Deputy Chief Medical Officer for England, less than two weeks before the first lockdown Harries was telling the public in a televised interview with then-Prime Minister Boris Johnson that “for the average member of the public” masks “are really not a good idea… people can put themselves at more risk than less… you can actually trap the virus in the mask and start breathing it in”. Harris was far from alone in dismissing the value of mask-wearing, of course, because in the early spring of 2020 the public health experts spoke with one tongue. “In terms of wearing a mask, our advice is clear: that wearing a mask if you don’t have an infection reduces the risk almost not at all. So we do not advise that,” Professor Chris Whitty, England’s Chief Medical Officer, had told Sky News on March 4th. “We do not recommend masks for general wearing,” echoed England’s Deputy Chief Medical Officer, Professor Jonathan Van Tam, on April 3rd. On the same day, Professor Jason Leitch, Scotland’s Clinical Director said, “the global evidence is masks in the general population don’t work”.
The experts were so clearly united in their anti-mask stance that, around this time, the Advertising Standards Agency (ASA) banned the advertisements of two companies because of spurious claims that their face coverings would protect against coronavirus. The intervention by the ASA won the unequivocal support of NHS Medical Director Professor Stephen Powis who said, “callous firms looking to maximise profits by pushing products that fly in the face of official advice is outright dangerous and has rightly been banned”.
On April 16th, then-Transport Secretary Grant Shapps had told ITV that wearing masks would be “counterproductive… the suggestions people would make their own masks; whether it’s clothing and that sort of thing which doesn’t really provide that much protection. Secondly, the way people take it off can sometimes do the reinfection [sic]. Thirdly, it can provide a false sense of security”. But only 49 days later, on June 4th 2020, Shapps announced that “face coverings – not surgical masks – the kind of face covering you can easily make at home” – would be compulsory on public transport from June 15th, on pain of fines of up to £100. A day later, Government announced that, effective June 15th, staff would be required to wear surgical masks – and visitors and outpatients “face coverings” – in all NHS hospitals, a state of affairs that would persist by law for almost two entire years.
Some may argue that, as there is no longer a legal requirement, there is therefore no problem. But there is no shortage of commentators periodically agitating to make the practice a legal requirement again. And in any case, healthcare settings see us at our most vulnerable. Why should we even be asked to live out an intrusive, dehumanising charade? Especially off the back of two years of state-driven hysteria and an unprecedentedly draconian global restriction regime that achieved the grimmest of logical conclusions when one victim, Stephanie Warriner, was choked to death by hospital guards for the ‘crime’ of wearing a mask too low on her face.
It has long been recognised that masks achieve no appreciable reduction in the transmission of respiratory viruses. We knew this in 2015-16 with regard to surgeons and their patients (here and here). We knew this in 2020 from a gold-standard Cochrane review, an analysis of 14 studies on influenza and a healthcare investigation that concluded that masks “may paradoxically lead to more transmissions”. The amount of robust evidence pointing to the ineffectiveness of face coverings has only increased since this time, culminating in the 2023 Cochrane review. On healthcare settings specifically, a study in April 2023 concluded that mask requirements in a large London hospital made “no discernible difference” to Covid transmission rates. UKHSA guidance acknowledges that the evidence of the effectiveness of non-pharmaceutical interventions (including masks) is “weak” and “would be graded as low or very low certainty”. Even when masks were legally required in healthcare settings, no quality standard was ever specified – we were asked to swallow the absurdity that strapping any old bit of rag to our faces was to ‘Follow the Science’. Refer to the Health and Safety Executive (HSE) and you will find that even surgical masks are not regarded as personal protective equipment (PPE) under the European Directive 89/686/EEC (PPE Regulation 2002 SI 2002 No. 1144). HSE notes that surgical masks “are normally worn during medical procedures to protect not only the patient but also the healthcare worker from the transfer of microorganisms, body fluids and particulate matter generated from any splash and splatter. Whilst they will provide a physical barrier to large projected droplets, they do not provide full respiratory protection against smaller suspended droplets and aerosols”.
Even leaving aside Harries’s now repeated suggestions that masks can cause more harm than good when it comes to Covid, health is of course about much more than attempting to avoid one virus, and masking has never been a benign intervention.
Routine masking, particularly for long periods of time, is increasingly recognised to be associated with a wide range of physical, psychological and social harms (see here for an overview). A recent research study highlighted the potential risks of elevated carbon dioxide levels associated with long-term mask wearing, particularly for children, adolescents and pregnant mothers.
Then there are the human costs of routine masking in healthcare settings: the exclusion of the hard-of-hearing; the re-traumatising of the historically abused; the increased risk of falls in the elderly; the exacerbation of confusion in the already confused; the aggravation of the autistic, anxious and panic-prone; the marginalisation of already stigmatised groups; and the impediment to the goal of soothing the frightened child or suicidal teenager. Faceless interactions impede the development of healing relationships. Humane healthcare, delivered with demonstrable warmth and compassion, will always be more effective than the robotic version emitted by a faceless professional hidden behind a veneer of sterility.
But patients in healthcare settings aren’t the only victims of the mask farce. Respect for institutional science has rightly taken a knock as well, as Peter Horby, Professor of Emerging Infectious Diseases and Global Health at the University of Oxford, conveyed to the Covid Inquiry. During peak Covid, Horby chaired NERVTAG, a high-profile group of scientific experts who routinely provided advice to SAGE. Appearing before the Inquiry on October 18th 2023, he confirmed that “NERVTAG had looked at the issues of face masks in the past… and had taken quite a stringent scientific view that the highest quality evidence is randomised controlled trials… and those data were fairly clear… that the evidence was weak. And we maintained that position on how we saw the evidence, focusing on the data from randomised controlled trials.”
Lady Hallett (the less-than impartial Chair of the inquiry) interrupted, saying, “I’m sorry, I’m not following, Sir Peter. If there’s a possible benefit, what’s the downside?”
“The downside is that you are making a population-wide recommendation based on weak evidence which may weaken trust in your scientific independence and integrity,” Horby replied.
Why would scientists and public health experts risk this very obvious downside? The most obvious explanation is that forcing the public to wear masks was a highly visible way to be seen to be ‘doing something’ that came with at least a couple of attractive bonuses to politicians and bureaucrats. One, the practice had superficial ‘gut feel’ appeal to the layperson – if you didn’t think about it very much, and never looked at the evidence, masking felt like it should work. Two, as with most of the non-pharmaceutical interventions (NPIs) it shifted blame for Covid impacts away from the state and health service and onto individuals. ‘Rule breakers’ among the public – now easily identifiable by sight – made for convenient folk devils and scapegoats.
On June 1st 2022, in a letter co-signed by the same Professor Stephen Powis who had been so withering about “callous firms” promoting face masks to stop the spread of Covid, new guidance from NHS England – referencing “updates from UKHSA” – effectively passed the buck for masking down to local healthcare managers, amid general talk of “transitioning back” to pre-Covid policies.
At the time, the Smile Free campaign wrote:
Two years after the imposition of masking in English hospitals, it is most regrettable that NHS England and the authors of this latest guidance could not simply have signalled a clean break and consigned this unprecedented, poorly evidenced and ultimately failed policy to history. Since they have chosen not to, by far the most likely outcome is that masking in English hospitals will now become a ‘postcode lottery’ based on the whims of local staff.
In an open letter co-signed by over 2,200 doctors, scientists and healthcare professionals in summer 2022, we had called on the NHS Chief Executives in each of the home nations to revise the guidance for doctors, nurses and other health professionals with immediate effect, leaving the individual – whether a professional or service user – to decide whether he or she wanted to wear a mask or not, thereby bringing healthcare into line with other community settings. But with the Government having terrified the public with lurid fear campaigns, advised gravely that masks would “keep everyone safe” and endorsed this claim with the law and eye-watering fines of up to £3,200 for non-compliance, perhaps we should not be surprised that simply pulling the comfort blanket away again was rather too rich for the NHS’s blood.
A reply, dated October 4th 2022, from Dame Ruth May, Chief Nursing Office and national lead for infection control at NHS England, justified current mask advice to hospitals with a computer modelling report linked to Professor Neil Ferguson’s Imperial College that by its own admission was “highly uncertain”. We were startled to find the report was also literally labelled “Should not be used to inform clinical practice” on page one.
Despite masks never having actually gone away in many healthcare settings, the following day, news outlets were reporting the “return of the mask”. Between the Mail and Sun’s accounts, eight different NHS Trusts were reintroducing a range of measures, prominent among which were mask “requirements” for patients and visitors.
In all cases, these measures were apparently being introduced as a result of “Covid’s resurgence” with “surveillance data suggesting Covid is on the rise in England”.
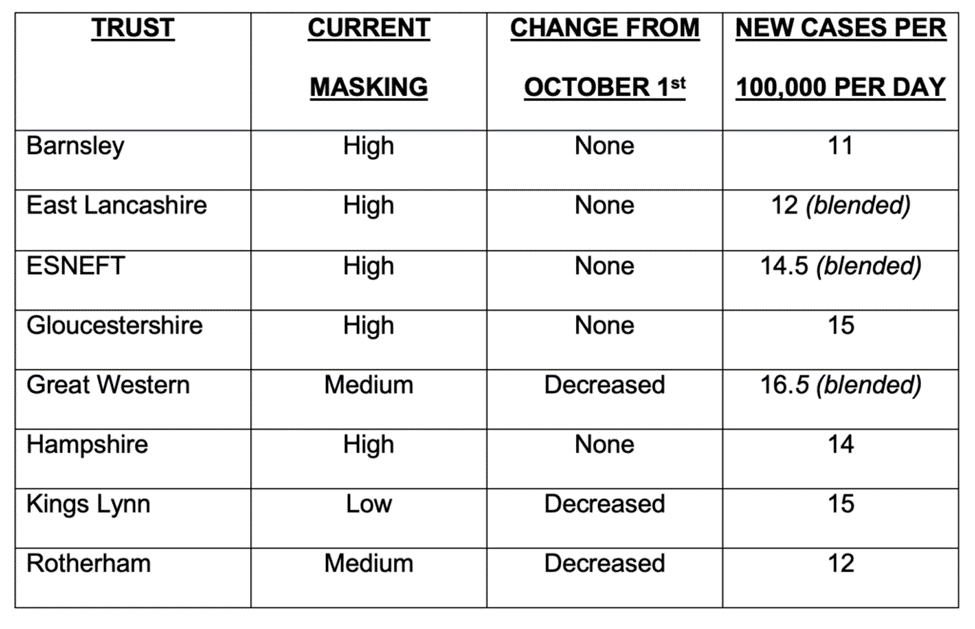
Were those trusts imposing mask “requirements” in areas of above-average Covid prevalence? It appears not; there was no discernible pattern and, in fact, glaring contradictions. For example, Barnsley, with continuing significant restrictions, had a catchment area with the lowest daily new cases per 100,000 people; while Swindon and surrounding areas, served by the Great Western Trust that had reduced its mask restrictions, had the highest rate.
In investigating one trust, ESNEFT, the 10,000 patients reportedly seen every day were still being subjected to “safety theatre” going into a third year of the Covid saga, seemingly driven by a very small and unaccountable infection control team, if not in reality the whims of one man.
Even into autumn 2023, ESNEFT’s website giving advice for visitors to wards and to Accident & Emergency still states that people are required to wear “surgical face masks covering their nose and mouth” where there is a “high-risk of transmission of contagious respiratory infection” or if clinical staff ask them to wear one.
On September 26th 2023 the Smile Free campaign submitted a Freedom of Information (FOI) request to ESNEFT, seeking three pieces of information:
- Within the geographical boundaries covered by ESNEFT, COVID-19 case numbers (per 100,000 people) by month since October 2022.
- A copy of the full risk assessment document used to determine that it is necessary for ESNEFT to keep “mandating” the wearing of face masks.
- The most recent date that these mandates were subject to risk assessment and updated.
ESNEFT replied a month later, saying that it “does not have access” to any data related to Covid case numbers within its locality. Obviously, this raises the question as to how its staff ever knew whether ‘Covid cases’ were increasing, decreasing or staying flat? It further raises the question as to how they were ever able to make any decisions on mandating, or even recommending, the wearing of face coverings as ‘protection’ against a respiratory virus? It also throws into doubt ESNEFT’s operational competence. ESNEFT also claims that, as it hasn’t operated a “universal mandate” since May 2023, it doesn’t have a risk assessment. ESNEFT never answered the final question, concerning the most recent date at which it conducted a risk assessment. Should we conclude it has never done one?
In response to a similar FOI request around the same time, Sheffield Teaching Hospitals NHS Trust, which had reintroduced masking “requirements”, told us it doesn’t “hold the data for regional/community Covid data”, nor “a formal risk assessment” that would justify reintroduction of mask-wearing. In fact, it doesn’t have any “formal risk assessment” used to justify the mandating of masks at all, from any time. Instead it claims it has “a trust-wide expert group which reviews and agrees all actions required depending on the Covid prevalence level which includes the wearing of COVID-19 face masks”. In other words, unilateral decisions are made by a group of staff who don’t feel it necessary to follow the prescribed decision-making processes within their organisation (the NHS) and who don’t record their findings and document them in any formal way. We therefore followed up, asking for the roles of the individuals in this group. At time of writing, the trust had not provided an answer despite being long overdue based on FOI requirements.
In a second open letter in summer 2023, this time co-signed by over 2,500 doctors, scientists and healthcare professionals and 7,500 members of the public, we called on the NHS Chief Executives to immediately issue clear new guidance explicitly discouraging any routine requirement for staff, patients or visitors to cover their faces in healthcare settings.
This time, NHS England’s Dame Ruth May specifically referenced UKHSA guidance as the reason for the ongoing “postcode lottery”, stating “the current UKHSA guidance… sets out that in health and care settings, non-pharmaceutical interventions (such as mask wearing and enhanced ventilation) may be used, depending on local prevalence and risk assessment, with the aim to reduce the spread of SARS-CoV-2”. It is interesting that “local prevalence and risk assessment” should be emphasised as the key considerations, since our investigations show hospitals unable to provide any evidence of increased local prevalence, nor risk assessments, to underpin their arbitrary decisions.
On November 2nd 2023, a few weeks before Harries’s appearance at the Covid Inquiry, we wrote an open letter to her at UKHSA asking her to explain the discrepancy between UKHSA’s current guidance, which, while broadly recommending a return to pre-pandemic normality, continues to allow re-imposition of masks where there is a local appetite for it, and its recent literature review, which concluded the evidence for masks reducing viral transmission was, at best, very weak.
We asked Harries to immediately update UKHSA guidance so as to:
- Acknowledge the ineffectiveness of masks as a viral barrier;
- Explicitly recognise the range of harms associated with the masking of staff, patients and visitors in healthcare settings;
- Actively discourage the routine wearing of masks in all clinical areas.
At time of writing, we still await a reply – though we note that via her Covid Inquiry testimony Harries has clearly conceded point one above, and identified one extremely significant harm – the false sense of security engendered by masking – from point two.
In everyday life, it only makes sense to initiate a new action if we are reasonably confident it will not result in more harms than benefits. The importance of this notion is amplified manyfold when it is powerful actors – politicians and their public health experts – forcing the change on their citizens. The ‘Precautionary Principle‘ in its original form endorsed this important rule and complemented the Hippocratic oath of our medical doctors to “first do no harm”. Yet throughout the Covid saga we have witnessed a total disregard for this principle with the imposition of a series of non-evidenced restrictions, driven more by politics than science, where the resulting collateral damage – to both the public and to the reputation of medicine and institutional science – has dwarfed any benefits. A prominent example of such absurdity has been the mask requirement in community settings.
Dr. Gary Sidley is a retired NHS Consultant Clinical Psychologist and co-founder of the Smile Free campaign opposed to mask mandates.















To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
Repeat after me:
Data are racist.
Facts are lies.
Breath is death.
Strokes are normal.
And as Monkey Pox shows, anal Schwabs are bad for your health.
this could also be to do with the massive backlog of people who have not been treated and left to suffer for the last two yrs, if you can’t get a doctors appointment or are left with a video call and left un or mis diagnosed, more people are becoming sicker as a result. These jabs are also a contributing factor as well as doctors etc dismiss that the jabs may be causing an effect which leads to a overlook of conditions etc.
Stress, depression, unemployment, overeating and drinking during lockdowns, mass vaccination.
All predicted as dangerous here by us two years ago.
Indeed. All of this was predicted by so many people, which makes one wonder why no real ‘risk-benefit” analysis occurred before these “health” and “safety” protocols were mandated. They all produced extra and unnecessary deaths. “Public health” has never been worse in my lifetime.
“jabs may be causing an effect” – we need to get real!
Time is getting short.
Coronavirus lockdown could cause ‘200,000 extra deaths’ | Metro News
is 200 greater than 6?
The cult becomes a cull
Every cloud
If this continues then by my calculation by the time winter fuel payments etc come due in October they will have saved themselves £30,588.800
They’ll call it a good start
Hmm, let’s see what could have caused this to happen?
Blame it on Liverpool fans
I didn’t know Trump supported Liverpool?
https://rwmalonemd.substack.com/p/monkey-pox-update?s=r
Malone posted this an hour ago. Suggests that the monkeybollox has been genetically manipulated.
In conclusion, the preponderance of current evidence is pointing towards a hypothesis for the origin of this outbreak which is increasingly consistent with prior “war game” scenario planning, remarkably akin to that which occurred during Event 201, which posits emergence of an engineered Monkeypox virus into the human population during mid-May of 2022.
When asked why so many people in their twenties and thirties were dying prematurely of heart attacks and strokes, a spokeswomxn for the regime said “new regime science shows that coffee, bananas, atmospheric conditions, listening to the wrong kind of music, muffins, not sleeping enough, dogs, curtains, jelly beans, freedom, free speech, the right to protest, voting and cold air have all started causing heart attacks in 2022, and the novel cell therapy known to cause clots has nothing do to with it, bigots.”
These hypothesised current excess deaths of 10% or so associated with prior lockdown and or vaccines could have been running for the last twelve months.
Up until now masked in the weekly death data by the ‘premature [by a year or so] deaths’ of the very old and frail of 2020 being subtracted, or having been ‘brought forward’, from 2021-2022?
Those 120,000 excess deaths covering circa 2020 to early 2021 have to be deducted from later death data at some point.
‘According to data from the Office for National Statistics (ONS), Covid deaths have been dropping as the Omicron waves have subsided…’
Lying toads!
Omicron was so mild it was indistinguishable from a slight Cold, so how could it be causing any more than a few chance deaths?
What they mean is Omicron has done what coronavirus do, start disappearing due to seasonal change, and they can’t pin deaths on it.
So add more than 1 000 because of tricksy ‘underlying’ double-talk.
Increase in all-cause mortality: mRNA ju-ju brew deaths which unlike CoVid are being vastly under-reported, deaths from other diseases due to weakened mRNA spike immune systems, and lack of medical care because the permanently overwhelmed NHS is overwhelmed.
But the real cause = Government. When will the arrests and trial start?
If we look at the occurrence data for all cause deaths for England and Wales (which aren’t affected by when bank holidays fall and distorts reported deaths) we can see there has been a move in all cause deaths above the 5 year (2015-2019) average since around the end of March. This increase associates with the latest booster experimental vaccine doses. Association isn’t proof of causation of course.
Ignore the very last point on that chart (20th May) as estimates of deaths that have occurred but not been reported will be subject to major uncertainty.
And essentially the same chart but this time showing the percentage that all cause deaths exceed the 2015-2019 average (i.e the percentage above the blue line the green line is in the previous chart)
There is this very good analytical substack, FC, it may interest you.
Causes of death in Massachusetts
https://coquindechien.substack.com/p/neoplasm-to-ectoplasm-in-months?s=r
Thanks. I’ll have a look later.
Needs to be broken down by age cohorts. I’d wager the 20-50 groups show a sharp increase compared to baseline.
Nothing to see here.
Your Govt loves you xxx
If they’re jabbed it serves them right, frankly.
Whisteblower’s Lawyer: Pfizer Got Away With Vaccine Fraud Because Government Was Co-Conspirator
https://amgreatness.com/2022/05/30/whisteblowers-lawyer-pfizer-got-away-with-vaccine-fraud-because-government-was-co-conspirator/
The gene therapies are working, slowly but steadily and surely.
Just another faint and fall and another cancer comeback after 25 years of remission in my circle of acquaintances came to my attention last week.
“Dear Friends, Sorry to Announce a Genocide”
https://naomiwolf.substack.com/p/dear-friends-sorry-to-announce-a?s=r
Worth reposting here.
Noone can still believe in a cockup after having read just this.
“In the internal trials, there were over 42,000 adverse events and more than 1200 people died. Four of the people who died, died on the day they were injected.”
“The side effects about which Pfizer and the FDA knew but you did not, include blistering problems, rashes, shingles, and herpetic conditions (indeed, a range of blistering conditions oddly foreshadowing the symptoms of monkeypox).”
“The internal documents show that Pfizer (and thus the FDA) knew that angry red welts or hives were a common reaction to the PEG, a petroleum-derived allergen in the vaccine ingredients — one that you are certainly not supposed to ingest. Indeed, PEG is an allergen so severe that many people can go into anaphylactic shock if they are exposed to it. But people with a PEG allergy were not warned away from the vaccines or even carefully watched by their doctors, EpiPen in hand. They were left to their shock.”
Confirms for me for sure if I had had even one of those jabs I wouldn’t have suffered a jab injury. I’d be dead.
There was a very interesting article from a German pathologist which I saw this morning, basically saying that whenever he carries out an examination he finds tissue which has been damaged by the “vax” jab and which caused or contributed to the death by strokes, aneurysms etc.. The immune system tries to destroy the vax induced spike – with consequences which were predictable i.e. death.
I intended to provide a link – but guess what, it appears to have disappeared.
If anyone can find it please let me know.
It was, I think, from the Hart group.
Not the link you were on about, but covers the same information.
https://doctors4covidethics.org/vaccine-induced-damage-to-our-vascular-system/
Thanks for that, much obliged.
It is the same one, but I kept getting the dreaded P. 104
Non- Covid but what about Covid Vaccine deaths then?
I read Comment Sections for important anecdotes. This morning at a Substack site I read a post from someone who said a close friend works at a florist shop. This person said that her shop has never had so many orders for flowers for funerals.
I prefer to compare weekly deaths with those from years completely outside the hoax pandemic. I use ONS data for 2010-2019, adjusted by population totals to 2020.
What this shows is that this week is 10.6% above the ten-year maximum.
Even averaged over the last 3 weeks, it is 4.0% above maximum and 13.7% above average.
I update regularly on Telegram here.
Yes we all know the covid vaxx is driving excess death in every country that pushed the dangerous and lethal covid vaccines. Read Steve Kirsch, Joel Smalley, Jeff Childers, el gato on their substack. The information is all there. Also read Expose. Demand your gp and mp face reality and have access to this data. Legacy media will not print it. Until we are given back truth, honesty and integrity, this will continue. Demand your rights back.
See infant mortality rates in Scotland – shock increase reported!