In last week’s post I mentioned that prior to the vaccines’ release there were calls for there to be rigorous monitoring of the vaccines’ safety and effectiveness. Thus I was pleased to read last Wednesday of the latest attempts by the the Health Advisory and Recovery Team (HART), an independent group of medics, scientists and academics, to get the U.K.’s medical products regulator, the MHRA, to explain why it hasn’t kept its promises to monitor the safety and effectiveness of the Covid vaccines in the time since they were rolled out back in December 2020. I’d add that this situation has been mirrored worldwide, with remarkably little in the way of the type of monitoring that would be expected of a new medical product.
The importance of these post-approval monitoring studies can’t be understated – pre-approval testing can definitely give an indication of safety and effectiveness, but a full understanding of the impact of medical products, including longer term effects and interactions with other drugs, is generally only obtained through rigorous monitoring on release. It is for this reason that initial roll-out of new medical products is generally limited to those with the greatest risk, with the product being offered to those at a lower risk once the results from the initial roll-out show effectiveness and safety in the ‘real-world’. I have found it troubling how medical authorities worldwide didn’t explain this need for rigorous monitoring of new medical products – instead they merely repeated the mantra that the pre-approval studies showed the Covid vaccines to be ‘safe and effective’, as though science had found the truth and that there was no more discussion to be had.
Indeed, the Covid vaccines had more need than usual for very rigorous post-approval monitoring:
- Their testing was rushed. This was sold to the population as being ‘all the parts of the testing being done in parallel’, but it really doesn’t work this way – by the time a medical product is ready for approval there will be many years’ worth of data from those first given the product. For the Covid vaccines there were only data from clinical trials on the impact of the vaccines for a few months post vaccination. It would have helped if the pharma companies had given regular updates on the fate of their human guineapigs during 2021. However, there has been little update of the continued safety and effectiveness in those individuals beyond the six month point post vaccination.
- The product was a vaccine. By design this means that it will be given to individuals who aren’t, at that point, under any particular risk (as opposed to a treatment for an individual who has already caught a given disease). This is doubly true for healthy younger individuals who weren’t at risk from Covid in the first place. I was expecting the vaccine rollout to stop after those aged over 65 had been vaccinated, to allow for the impact of the vaccines to be studied without risking those who weren’t at risk. I still don’t understand why our medical authorities proceeded with a universal vaccination policy at that point.
- The experimental nature of the vaccines. All of the Covid vaccines used in the West were based on novel technologies for which there were limited data on the longer term impact of the technological approach. The viral-vector vaccines (AstraZeneca, Janssen) were not quite so novel as that technology has been used for a number of candidate vaccines for a number of diseases, though never for very large numbers of people. Prior to Covid the only approved viral-vector vaccines were for Ebola, which have only been given to relatively small numbers at very high risk, as ‘ring vaccination’. The mRNA based vaccines were much more novel, and before the Covid vaccines only very limited numbers of people had ever been given this type of medical product. It is truly bizarre that our medical regulators decided that it would be appropriate to inject these mRNA vaccines into a large proportion of the population, most of whom were at little risk from the disease itself.
- The outcomes from prior attempts to make a coronavirus vaccine. Scientists have been trying to make a vaccine to protect against coronavirus infection (‘colds’) for decades. They all failed – not simply because ‘they didn’t work’, but also because some candidate vaccines resulted in increased risk from disease, potentially coming to light some time after the vaccines were given.
The undertaking of rigorous vaccine effectiveness and safety studies isn’t trivial. The chief difficulty is that different people have different vulnerabilities to a given disease (particularly noticeable as an age effect), different risks of catching the disease and different health-seeking behaviours. These introduce a source of bias in any efforts to identify the effectiveness of a vaccine (or, indeed, any medical treatment). The traditional way of dealing with this bias is to split the group (vaccinated vs unvaccinated) into multiple risk and behaviour groups and undertake the analysis such that differences between groups are (almost) compensated for (e.g. the outcomes for vaccinated elderly male individuals with no co-morbidities who don’t wear face-masks will be compared only with unvaccinated elderly male individuals with no co-morbidities who don’t wear face-masks). The best studies are prospective, meaning individuals are put into the different risk and behaviour groups before the medical products are given; this is what should have been done for the Covid vaccines. Nearly, but not quite as good, are retrospective trials where the individuals are put into different groups after the medical products were given. It is still possible to do these; however, few have actually been done.
These prospective and retrospective matched cohort trials are effective and accurate, if done properly. But because of the effort involved in grouping the different individuals appropriately they are quite expensive and effortful to undertake. Ever mindful of the need to spend taxpayers’ money wisely (or perhaps from some other motive), governments worldwide chose to use other, cheaper and easier, methods instead.
At the end of each Vaccine Surveillance Report is a long list of references for the studies providing the supporting data for the claims made in the report. The vast majority of these studies that relate to vaccine safety and effectiveness used the Test-Negative Case-Control (TNCC) method as the basis of their design. This is quite a smart way to undertake vaccine effectiveness studies; it is certainly a far easier and cheaper approach than other methods, primarily those that use the matched cohort approach. However, it isn’t completely clear that this method is appropriate for use with the Covid vaccines.
TNCC is quite simple in concept – it compares the positive rate of infection with the incidence of disease that ‘looks like’ the disease in question but which isn’t. For example, for influenza you might investigate the proportion of people with typical flu like symptoms that have a positive test for influenza with people who also have typical flu like symptoms but that test negative for influenza. This method automatically takes into account multiple potential differences between different vulnerabilities and behaviours, and eases the analysis process. TNCC is, in principle, an excellent and accurate method to measure the effectiveness of a vaccine. However, it makes a fundamental assumption – that all factors that might change the probability of an individual testing positive affect equally the probability of an individual testing negative. Thus TNCC assumes that:
- If a proportion of the population were more vulnerable to catching the specific disease being vaccinated against they’d be equally vulnerable to catching a similar-but-different disease.
- If a proportion of the population exhibited risky behaviours that resulted in them being more likely to catch the specific disease they’d also be more likely to catch a similar-but-different disease.
- If a proportion of the population were more likely to get themselves tested with only minor symptoms they’d also be more likely to get themselves tested if they had minor symptoms after catching a similar-but-different disease.
The problem with the TNCC should now be clear – it assumes that the vaccine itself has no impact other than in the risk of the disease being vaccinated against. This is often a fair assumption; however, it is by no means guaranteed. In particular, if the vaccine happens to increase the risk of catching a similar-but-different disease then this can result in the TNCC giving misleading results.
To illustrate this point, consider a theoretical vaccine that halves the risk of a certain disease, but where individuals were ten times more likely to have a ‘similar but different’ disease before vaccination started and where the vaccines didn’t alter the chances of catching this ‘similar but different’ disease. For a similar number of vaccinated and unvaccinated (let’s say 10,000 and a 1% chance of catching the disease in question) the numbers tested might be:
- Unvaccinated: 100 positive tests (1% actually had the disease) and 1,000 negative tests (10 times more likely to catch the ‘similar but different’ disease).
- Vaccinated: 50 positive tests (the vaccine halves the chance of catching the disease to 0.5%) and 1,000 negative tests (same incidence as the unvaccinated as the vaccine doesn’t impact on the ‘similar but different’ disease).
- The TNCC estimate of vaccine effectiveness is given by 1 – (50/1,000)/(100/1,000) = 0.5, i.e., 50% VE.
Thus TNCC estimates that the theoretical vaccine halves the risk of catching the disease, which means it agrees with our initial definitions of how well the vaccine performs. Great – the TNCC approach works.
However, consider an alternative scenario, where the vaccine increases the risk of both catching the target disease and a similar-but-different disease. To continue the example, consider that the risks of both are doubled:
- Unvaccinated: 100 positive tests (actually had the disease) and 1,000 negative tests (10 times more likely to catch the disease). Again, this is the same as the previous example.
- Vaccinated: 200 positive tests (twice as likely to catch the disease ) and 2,000 negative tests (twice as likely to catch the ‘similar but different’ disease).
- The TNCC estimate of vaccine effectiveness is given by 1 – (200/2,000)/(100/1,000) = 0%.
In this case the vaccine appears to have no impact (perhaps the interpretation is that its effectiveness has waned with time). However in reality it is actually increasing the risks both of the disease in question and of similar-but-different diseases. Because the assumptions of the TNCC method aren’t valid the estimate of VE is incorrect. Note that a matched cohort study would have identified the increased risks of vaccination in the above example, and should also have identified the increased risks of catching the similar but different disease.
Obviously this is an oversimplified example, but the fundamental is the same. If vaccination results in an increase in the incidence of a ‘similar but different’ disease then the TNCC method will give highly misleading results.
But how can vaccination cause a change in the risk of a disease different to the one vaccinated against? This goes against our idea of how vaccines work – they’re a marvel of science that in some cases have resulted in significant benefits to global health. However, there are instances where vaccination does change risk from other similar diseases. These cases are unusual in vaccines actually in use, but that’s because the years of clinical trials (in animals first, and then humans) generally identify such a risk before they are used in the general population. Nevertheless, before TNCC is used it is necessary to test whether there is any change in the ‘test-negative’ condition. This hasn’t been done for the Covid vaccines. However, I note that there is anecdotal evidence that there might be changes in infection risk for other diseases following vaccination: the arrival of ‘the worst cold ever’ last autumn; monkeypox (a disease not normally associated with human-to-human transmission); meningitis in Florida; an increase in cases of norovirus in the U.K. this spring; a nasty influenza outbreak in Australia and New Zealand during their recent winter. I’m sure there’ll be a repeat of last year’s ‘worst cold ever’ this autumn, and we’re already hearing shouts of the imminent danger posed by influenza. It is important to note that an increased risk of infection with other diseases isn’t only faced by the vaccinated. There might be an increased risk of disease in the vaccinated, but as they will have some prior immunity to most common viruses this might not have much impact on the individuals themselves beyond a mild cold. However, young children will often have no prior immunity and there’s a risk of them getting quite ill even with common viruses, and the elderly have impaired immunity in general and can also get rather ill with these viruses. I believe that this is what we’re seeing in the U.K. (earlier this year) and USA (now) with increases in hospitalisations in the very young and very old due to RSV infection. Again, note that just because the hospitalisations are in the young and old it doesn’t mean that only the young and old are getting infected, just that they’re the ones that seek healthcare support; the majority of those not old nor young will simply moan about having a cold.
One interesting piece of circumstantial evidence pointing towards viral interference is the incidence rates of ‘other respiratory infections’ compared with Covid infections. These data are seldom gathered because ‘colds’ are usually rather inconsequential and the assumption is there would be no link with Covid. However, data from the Zoe Symptom Tracker might suggest otherwise.
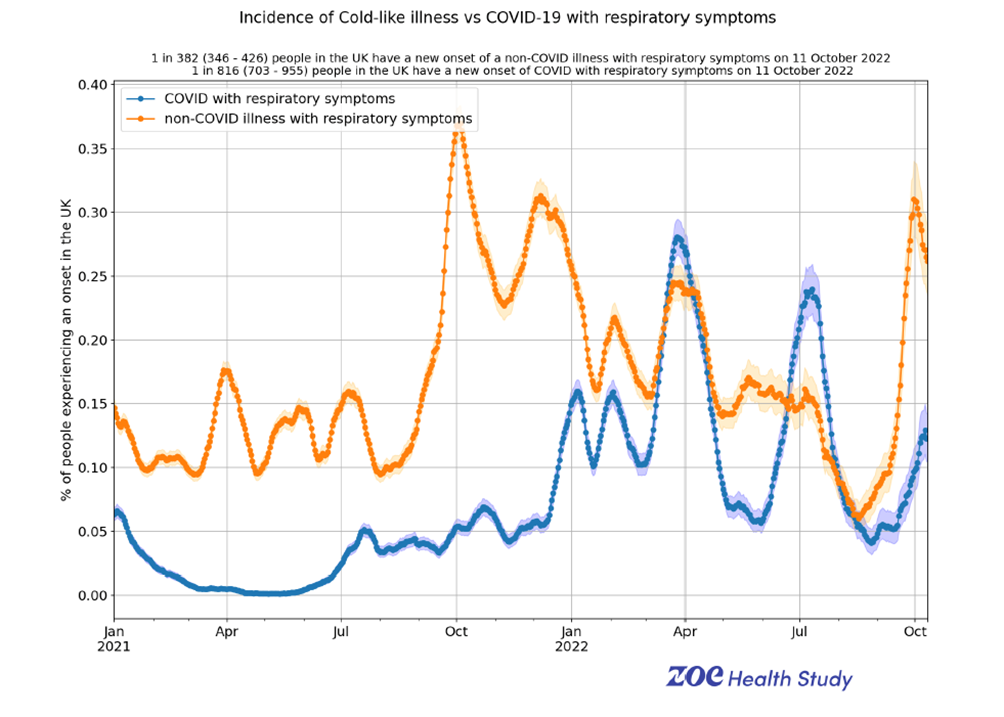
These data certainly suggest that there’s some kind of connection between risk of infection with Covid (blue line) and risk of infection with other respiratory viruses (orange line); this appears to start to emerge last autumn and become prominent with the arrival of the Omicron variant last winter.
Is there any other evidence? One of the fundamentals of any measure of vaccine effectiveness is that whatever the method it should give a similar result. While most estimates of the Covid vaccines’ effectiveness use TNCC there are a few instances where a study has included the results of both a matched-cohort analysis and a TNCC analysis. There have been hints of this in many studies over the months; my favourite was a study undertaken last year by Imperial College. The results?
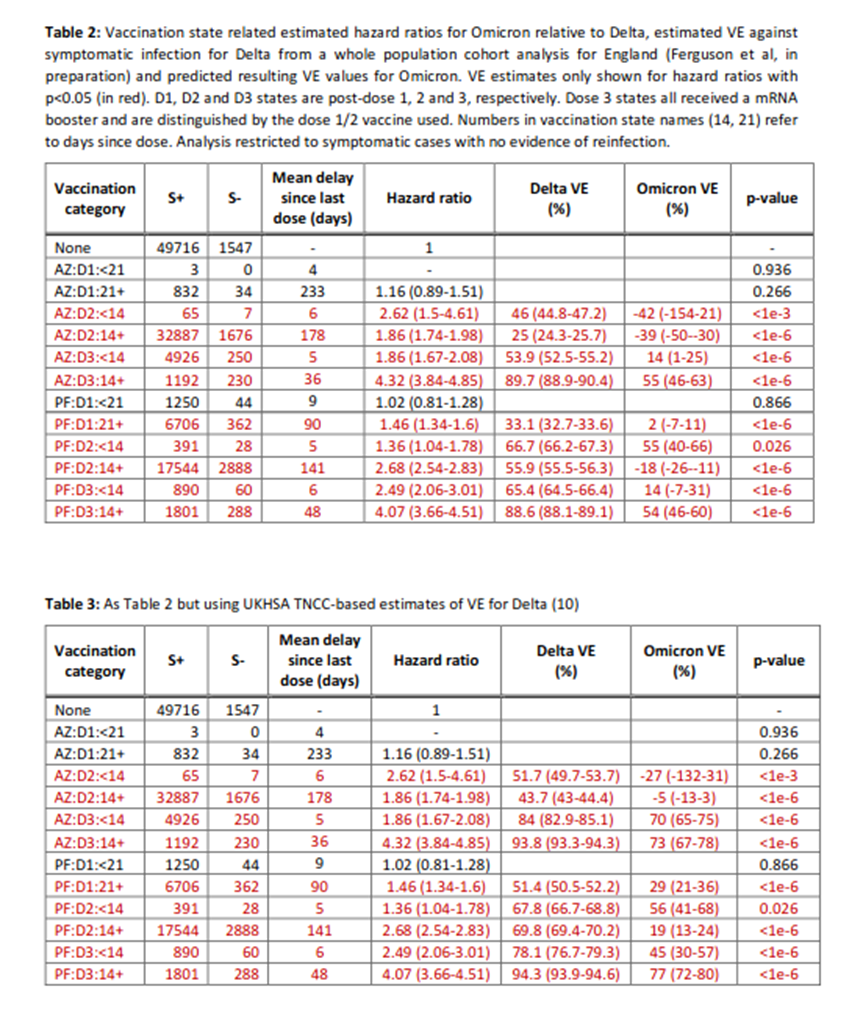
The estimate of vaccine effectiveness (VE) using the matched cohort method is consistently much lower than the TNCC method, falling below zero for some data points. This isn’t definitive proof that TNCC is giving misleading results. But it very much is evidence to support looking much harder at the assumptions of TNCC and whether they’re introducing bias and thus an overestimate of VE. My favourite part about this study was how Imperial released the data in one of their occasional reports on Covid – and the data were never seen again. I wonder if this is because the data were inconvenient.
The study suggests that the vaccines offer negative effectiveness – that is, that they make it more likely to catch the disease. Can this even be possible? Interestingly, it isn’t that unusual to find vaccine candidates that increase risk of disease. Of course, we don’t see this in our experience of vaccines because those vaccine candidates that did increase disease risk are usually filtered out by the clinical trials that are needed to obtain regulatory approval (with some infamous exceptions, such as RSV and measles vaccines in the 1960s, and more recently a Dengue virus vaccine). What’s more, prior coronavirus vaccine candidates did often show a propensity to increase infection risk or disease severity – (for example, see Jaume et al.). Thus there should have been some expectation that the Covid vaccines might have led to negative vaccine effectiveness.
There have been other studies that have suggested that the vaccines might be increasing the risk of infection with Covid. Just to consider recent publications, Oxford University published the results of a matched cohort study that showed a negative vaccine effectiveness – that the vaccinated have a higher risk of infection than the unvaccinated. This has been discussed in the Daily Sceptic, as have two other recent studies that show negative vaccine effectiveness. I’ll note again a point that I made earlier – if matched-cohort and TNCC studies give different results it is a huge red-flag that the assumptions necessary to use TNCC aren’t valid, and that we should disregard these data and focus on using more robust methods to measure vaccine effectiveness.
One final point on the impact of the vaccines on reducing (or not) Covid infections: there has never been any serious mention of the impact of natural immunity in the UKHSA Vaccine Surveillance Reports. I suppose this might be excused (as it is a vaccine surveillance report). However, people are using these documents (and similar) to decide whether it would be worthwhile taking the vaccines. Without information on the protection offered after natural infection, how could individuals give fully informed consent? The lack of any real information on the protection gained after natural infection has been a fairly reliable theme from various authorities worldwide. It was almost as if these authorities were mainly interested in getting everyone vaccinated, and underplayed any information that might make an individual more likely to choose to forgo vaccination even if this was what was supported by the science.
In my post next week I’ll discuss an aspect surprisingly not actually covered by the Vaccine Surveillance Reports but that should have been – the side-effects of the vaccines.
Amanuensis is an ex-academic and senior Government scientist. He blogs at Bartram’s Folly.












To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
I used to believe that. Now I have serious doubts.
I wouldn’t be at all surprised that if we subjected other vaccines to the same scrutiny that we are beginning to apply to the covid jabs we would find that most of them don’t help and in fact do more harm than good.
Here’s a long article on the toxic vaccines rejected by the West then foisted on the Third by the philanthropath, Gates. Gates should swing.
https://thegrayzone.com/2020/07/08/bill-gates-global-health-policy/
Philanthropath. Excellent new word.
Indeed
http://vaccinepapers.org/
This 6min segment from Dr Paul Thomas’ presentation earlier this year highlights his and others’ work demonstrating vaccinated kids/adults are significantly less healthy than unvaxxed across the board.
https://yummy.doctor/video-list/lets-compare-the-vaccinated-to-the-unvaccinated/
On autism/vaccine links here are 160 papers in support of that harm
https://www.scribd.com/doc/220807175/160-Research-Papers-Supporting-the-Vaccine-Autism-Link
There will have been many many vaccine candidates that have been found out by the rigorous trials and discarded. So prior to Covid I would be inclined to trust the ones we have as they have been vigorously tested. That doesn’t mean I rush out to have the flu jab every year, as I still don’t need it. But i am pretty confident in their overall safety profile.
The problem now is that the health regulators seem to have decided their role is to promote new products rather than to monitor and regulate them. So I would be extremely wary of any new product from this point on.
I’m not convinced that the influenza vaccines offer any meaningful benefit.
I am absolutely convinced ‘flu vaccines are utterly bloody useless.
Remember that recently, in the UK, they have widened the age range for “free” ‘flu jabs. If they have overstocked on it in the hope that they would be popular, they could have overspent, as each one has a short annual shelf life. Guess which firms made a profit from that idea.
Are we sure past vaccine trials have been rigorous enough?
If they are so safe why do vaccine producers insist on liability exemptions for vaccines on the child immunisation schedule as a condition of their production?
They certainly are a mixed bag.
I’d say that there are a few vaccines that really are highly effective.
Many others appear to be less effective. Some appear to have some efficacy, but the side-effect rate looks concerning.
I do worry about the number of vaccines that are being promoted where the risk to the individual from the disease itself is negligible.
There’s also the question of the importance of moderate levels of exposure to pathogens over a lifetime that acts to ‘top up’ immunity without any actual symptomatic disease (and low viral loads). If this mechanism is disturbed, such as by mass vaccination reducing childhood illness significantly, then this opens up the risk of breakthrough infection or other disease symptoms emerging. There is evidence that this has occurred in the USA following mass childhood vaccination for chickenpox, resulting in significantly increased cases of shingles in older adults (ie, the repeated exposure to chickenpox virus suppressed reactivation of the virus in those that had caught chickenpox earlier in life). We don’t know if this mechanism might turn out to be rather important.
Finally, we don’t yet have a mature understanding of the role of mass vaccination in the evolution / selection of vaccine escape strains.
There’s certainly a great need to be cautious with the use of vaccines.
There’s also the question of the importance of moderate levels of exposure to pathogens over a lifetime that acts to ‘top up’ immunity without any actual symptomatic disease (and low viral loads).
I think that may well be a very important and little understood point. (Caveat on the rest of this post: I have no medical background.)
Way back in late April/early May 2020 it occurred to both me and Mrs TJN, after looking daily at the data coming in from various countries, that not only were lockdowns having no beneficial effect on the spread and death rate from SARS-COV-2/covid, they actually appeared to be making things worse.
But what might be a mechanism to explain such an observation? The following occurred to me back then, and I posted about it at the time, here and on the Spectator site.
In non-lockdown, where the virus is spread on public transport, door handles, surfaces, crowded streets, and so on, a great many people become infected by picking up low viral loads – allowing them to develop some sort of immunity, possibly only temporary, without suffering any meaningful symptoms.
A high initial viral load appears to have a high correlation with the subsequent severity of the disease. Thus if lots of people pick up the virus though low viral loads then presumably they will gain immunity at a cheap price. Hence the best way to achieve herd immunity.
In contrast, in lockdown conditions the virus is spread within households more, with the consequential high viral load, and thus more serious illness. Hence, through the ensuring of high viral loads, did not universal lockdown make the situation far worse than it might otherwise have been?
I was interested to read the other day an article by Eugyppius looking at respiratory illness data and observing that during the various ‘waves’ total infections appear to be limited to fewer than 10% of the population.
https://www.eugyppius.com/p/the-mysterious-disappearance-of-influenza?utm_source=post-email-title&publication_id=268621&post_id=79792616&isFreemail=true&utm_medium=email
Clearly, something is stops a typical respiratory virus in its tracks, at least for a few weeks or months until it is ready to take off again.
Eugyppius offers no mechanism to explain this, but I do wonder if exposure, especially repeated exposure, to a virus at low viral loads enables a great many people to develop at least temporary immunity. That might explain what we have seen.
An analogy: anything the body wants to do it has to train at it: muscles and cardiovascular systems soon deteriorate if they are not used. An athlete has to train in order to gain fitness. Surely we might expect the same thing of an immune system: it has to train against pathogens in order to maintain fitness.
Regarding the downvote, I’m more than happy and interested to hear criticisms and contrary ideas on such speculative topics. Please be my guest and I’ll read with an open mind.
We’re all stumbling in the dark and if others see different shapes in the gloaming I’m more than happy to hear.
There is a downvoter about, just about all sane contributions get that -1 red thumb. One of the damaged is among us.
Thing is, if anyone has anything o add to this, even if it goes completely against what I’ve written, I’d be pleased to hear. On this site we’re pretty well after the truth rather than pushing our own views.
One only has to look back at the history of what happened to the indigenous population in some parts of the world, when faced with immigrants that happened to have certain infections which they were normally able to cope with, but presumably the locals had never dealt with. E.g. some of those in north east America, when various Europeans invaded.
Indeed. Good point.
(Although afaik not all of them died – some had genetic dispositions which enabled them to survive, so there wasn’t a complete wipe out.)
Stewart, I have come to exactly the same conclusion.
We have been conned and lied to all our lives re “vaccines.”
Great article, amanuensis, but can we just clear up one thing:
“The product was a vaccine”
Huh? If I decide to change the definition of “The King of England” to include married white males living in Yorkshire, aged over 40, with two kids, a terrace house, a campervan and a motorbike, does that make me the King of England?
People were told the jabs were/are vaccines.
Also, quite handily, the definition of “vaccine” was changed some years ago to include incompletely tested mRNA “products”. Now ain’t that strange…
Thanks again for your articles!
The 500 notes from my monopoly set decided to self identify as pound sterling, but unfortunately my bank would not pay them in to my account. I was shocked at their bigotry and transphobia and have filed a complaint.
😁 😁
I also don’t like calling them vaccines. I hold my tongue and use the term because ‘everyone knows what I’m talking about’ and it is more understandable that ‘genetic based immunostimulatory agents’.
“I also I also don’t like calling them vaccines.”
Well, if you feel you must continue with the word, certainly on here, we would understand your meaning if you wrote “vaccines. “
I prefer “injectable prophylactics”, but with the same efficacy as a condom full of holes.
Agreed. The definition of a vaccine was changed to protect the guilty bar stewards who came up with the gunk.
Regarding natural immunity in the UKHSA surveillance reports: I emailed these people back in December 2021 regarding a statement in their report which stated (when referring to the unvaccinated) “this gives them some natural immunity to the virus for a few months”, pointing out that that “a few months” had zero grounding in science, and was obviously another lie being perpetuated to exaggerate the importance of being ‘vaccinated’. After an exchange of emails they actually agreed to remove the words “a few months”. This change can be seen in the reports between weeks 1 & 2 of 2022. Probably nobody noticed, but it was a small and important win and does prove that we can all make a difference – no matter how small.
Hats off to you sir!
Thanks for putting that effort in — if we all do a little then things can change; if we do nothing then they won’t.
Although I agree with that to some extent, it gets tedious and repetitious having to remind everyone that the sky is blue on a frequent basis.
A very interesting video ( 24mins ) from the co-author of Dissolving Illusions, looking at the history of vaccines, how Jenner’s famous Cowpox experiment was a flop and how the mandatory mass smallpox vaccination was totally ineffective.
https://odysee.com/@IvorCummins:f/Amazing_Short_Docu_on_the_History_of_Vaccine_Effectiveness:c
An excellent article, as per usual.
Might I suggest a slight alteration of bullet point 2 at the top to “The product was being passed off as a vaccine”. I know a lot of people go on about not calling it a vaccine, that’s not really what I’m getting at. When it was introduced, those producing it knew full well it would at best be a therapeutic along the lines of the mAb products that were being used, except that people’s own bodies were to be the production line, reducing costs for the manufacturers. Pfisser admitted it was not really a vaxx in the EU parliament when it said it had never tested for transmission or infection.
Now that it’s become known that a major PR/marketing firm representing pfisser and murderna had staff members embedded in the CDC, this explains a lot about why government agencies switched to wanting to shove this garbage into every living creature on earth, regardless of whether this was necessary or advisable. The CDC’s remit is (well, used to be) about safeguarding public health, a pharma marketing department/agent is only concerned with flogging as much of their product as is possible. Add a full exclusion of liability and they’d flog that garbage till the cows come home, regardless of effectiveness, injuries and deaths (as we are now seeing).
At this point I would like to see how much influence pharma marketing agents had on politicians and public health authorities – the CDC story is unlikely to be the only one. If there was ever a need for an enquiry, it is into the role of pharma companies in essence controlling and commanding public health authorities.
Thanks Jane.
I too don’t like the term ‘vaccine’. I’d have preferred it if they’d called them ‘something else’. I use the term because it really has been pushed so hard that it becomes clumsy to use a different term. I know that there have been ‘changes to definitions’ to include the genetic based immunostimulatory stuff as ‘vaccines’, but that doesn’t make it right. Anyway, Perhaps I should be more careful with my wording.
The situation with the CDC and other agencies is alarming. In the UK we’ve even had the MHRA decribing itself as an ‘enabler’. I’ve worked in clinical trials over the decades and everyone was scared of the MHRA, and quite rightly so. I very much worry about this change in tone.
We really do need to have some urgent investigations into the power that the pharma companies appear to be wielding now.
Same here. Manipulating the definition may well have been a marketing tactic. As ever, money talks, and if they had classified it as something like “protective mitigation drug against xyz”, would the procedure for developing the new product been more complex and financially risky?
As with the MHRA in the UK becoming an “enabler” rather than a “regulator” according to their chief executive.
Excellent article thanks. Amanuensis is the swedenborg of ATL.
The interaction of different virus types with each other is clearly of immense practical importance, and a subject about which very little is known, or even speculated upon.
Truth be told, with the non-pharmaceutical interventions (lockdowns etc.) and especially the vaccines we’ve been messing around with an incomprehensibly complex eco-system – playing God with things we know nothing about. That this should end in disaster should come as a surprise to absolutely no one – no one with a functioning brain that is.
You don’t need a medical background to be able to grasp this. But hubris was ever a human frailty, and the consequences of hubris a recurrent feature in human affairs.
However, surely never before has there been hubris on such a scale, and I feel in the pit of my guts that we are going to see consequences like never before.
The hubris is terrifying.
Was it the Greeks who said that nemesis follows hubris? I’d like to think that would be the case and every ‘guilty party’ faces sanctions. However, I am also long enough in the tooth to know that ‘The Establishment’ will look after its own. No individual will be found culpable but ‘lessons will be learned’.
“I feel in the pit of my guts that we are going to see consequences like never before.”
What will pan out in the next few years is the appearance of an ever more poorly, indeed very poorly, and high mortality population. The result of course of the depopulation agenda instigated via the injections.
Thanks very much, Amanuensis. These most recent reports you’re writing are extremely helpful to non-experts like myself.
As much as I appreciate these detailed analyses of this absolute crapshow, there’s one fundamental that is pivotal to all of it – how we’ve been testing for the illness we’re [supposedly] combatting against. The fact we’re using these PCRs in such a fraudulent manner any of the resulting diagnoses are all so up in the air it’s ridiculous. None of the data can be relied upon given how sketchy these diagnoses have been.
As its inventor Kary Mullis warned about, we each and all have many an RNA strand of pretty much anything and everything (at least potentially) and you’ll likely find it if you look hard enough. We live in symbiosis with bacteria [and viruses if those really are a thing] and at any given moment, and in reality have “an infection” – it’s just a matter of degree. So at what point do we say “you’ve got it”? That used to be when you’re showing symptoms (which made obvious sense) but not anymore.
Running these tests at such high amplifications, anything could be considered an infection – and is, I suspect, what we went through during the years from twilight and explains why such a high death toll with little anecdotal evidence in our streets (if it weren’t for the mockingbird media no one would’ve even noticed). Even from this starting point of dodgy testing, all the subsequent data is essentially useless, which makes the intervention even more worthless.
I know it’s all we’ve got and like I say I appreciate those who are pulling the numbers apart, at the very least we should be able to debunk the fraudsters with their own data but when we really get down to it – we’re playing stupid games… and we all know what type of prizes we get from doing that.
I agree — we’ve not really had a good understanding of the infection levels we’ve actually had, and (just as important), how they compare with ordinary ‘colds’ where symptoms are far below the level of clinical significance (ie, just a sniffle).
Eg, I’d like to have information on ‘deaths within 28 days of a cold’, etc. IMO this would give some context to the hysterical reporting we’ve had.
Great post.
Even from this starting point of dodgy testing, all the subsequent data is essentially useless
Yes, that’s the fundamental problem with all analysis based on infection numbers. I’m gobsmacked that more people can’t see this.
People are generally very bad at making sense of statistics, often because many of these statistics are lies and damn lies.
Orwell warned how authoritarians change the meanings of words, rendering them senseless and thereby robbing you of the ability to think.
The moment we give in to their definitions we are losing a crucial battle.
A positive PCR test is not an infection.
An mRNA jab is not a vaccine.