Richard Horton, the Editor-in-Chief of the Lancet, once observed:
The history of medicine is littered with wonderful early results which over a period of time turn out to be not so wonderful – or in fact even adverse… there are a whole string of recent examples where preliminary data led to a lot of excitement and caused changes in clinical practice and then eventually we realised they had done more harm than good. Why is it we never learn these lessons?
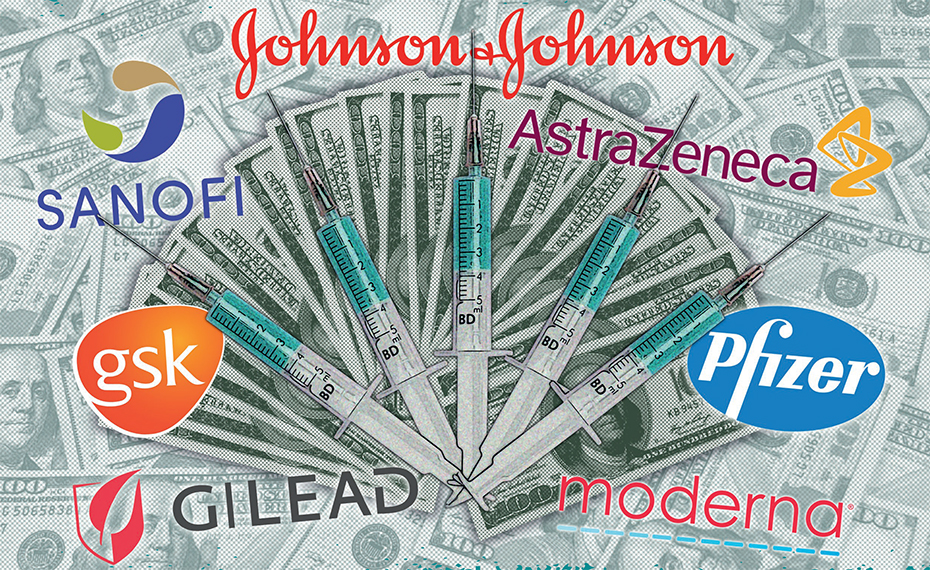
The pharmaceutical industry makes drugs for medical purposes. The industry campaigns hard for stronger patents throughout the world, though many economists are highly critical of patents in medicine. In some cases, patented drugs sell for thousands of times as much as they would cost if there were no patents. The industry illustrates some of the worst aspects of corporate power, corporate crimes, and ‘free lunches’ (or rents) that enrich executives and shareholders.
Social Costs, Private Profits
The early stages of drug research and development are often funded publicly, with universities and governments throughout the world paying much of the costs. Corporations often become involved only after early tests show promise. As one commentator pointed out:
The whole ecosystem in which innovation is housed – patents, copyright, finance, universities, research, knowledge transfer, ownership rules, regulation to ensure common standards – is co-created between the public and the private.
However, the companies that receive the patents keep the profits. Once they have a patent for a drug, companies can charge whatever will maximise their profits. In other words, whatever richer people can afford to pay. In an extreme case, a drug called Cerezyme cost over $200,000 for a year’s treatment, even though almost all of the development had been funded publicly. Healthcare systems in rich countries end up rationing drugs because of their cost.
Under these circumstances, allowing private companies to keep all of the profits from patented drugs, the development of which has been largely publicly funded, makes no sense. It is an example of how the economy is rigged to transfer immense wealth into the hands of executives and shareholders of big companies, whilst causing harm to others.
To make matters worse, it’s estimated that up to a third a of new drugs are no more effective than existing drugs. The Canadian government published a review of the 61 drugs patented in Canada in 2018. It concluded that only one was what is called a breakthrough, and 56 provided little or no improvement compared with existing medicines.
The U.S. National Institute of Health (NIH) carried out a large study published in 2002 to see if existing drugs for high blood pressure worked. Some of the drugs were among the world’s biggest sellers, yet the study found that old-fashioned diuretics worked as well or better than anything else. The diuretics cost $37 per year. The other drugs tested cost $230-$715 dollars per year, yet doctors were mostly prescribing the more expensive drugs.
Huge amounts of money have been spent on diabetes drugs, such as Avandia, that turned out to be ineffective. When they were first introduced, they were initially promoted as life-saving. The flu drug, Tamiflu, had minimal value, but massive stockpiles were purchased against H1N1 influenza in 2009 due to misleading research data and corporate lobbying. The manufacturer, Roche, withheld data to mislead everyone. This should be considered a serious crime, but is not actually illegal.
Fraud and Deception are Widespread
If a drug is really effective, it requires no marketing. Proper scientific studies demonstrate the benefits, and doctors and healthcare networks all over the world will use it. However, because most drugs are not very effective, companies need to spend huge amounts ‘persuading’ doctors to prescribe them. This includes gifts, holidays and other inducements (a euphemism for bribes). Many doctors are happy to go along with this. In some countries there is also a great deal of more general advertising. In total, more is spent on marketing than on research. This marketing is ultimately paid for by the people who buy the drugs, making them much more expensive.
Many new drugs are copycat drugs. In other words, variations of existing drugs. Good examples are Cialis and Levitra, which are variations of Viagra. The companies have an oligopoly, so they can control prices. Huge sums are spent on marketing these copycat drugs, but if they did not exist, nobody would miss them.
All big pharmaceutical companies have been convicted of selling harmful, sometimes fatal drugs. The industry has been fined over $50 billion during the last twenty years. In 2012, the pharmaceutical company Glaxo Smith Kline (GSK) was fined £3 billion in the U.S. for mis-selling drugs; for fraud, bribery and overcharging; for paying lavish inducements to doctors; for covering up negative research evidence; and for making false claims about medicines. GSK has also been fined in India, South Africa and the UK. Although these figures sound large, they are not enough to deter the companies from continuing to commit these crimes. The sales of a single drug can be worth many times these amounts, so as far as the companies are concerned, crime pays. No individual is prosecuted for criminal offences. In 1997 some pharmaceutical companies were fined for operating a global price-fixing cartel. One author has gone so far as to say that the official definition of organised crime closely describes the activities of the drug companies.
The industry has a long history of exaggerating the benefits of its drugs, understating the downsides and hiding negative results. A recent study showed that in the real world, medicines tend to be four times more harmful than the manufacturers claim. Adverse effects hospitalise a quarter of a million people in the U.K. and 2 million in the U.S. each year. There were 55,000 deaths from the pain-relief drug Vioxx, but the data were withheld by the manufacturer, Merck. Large numbers of heart attacks, strokes and deaths were caused by the diabetes drug, Avandia. One expert commentator stated that:
Until more meaningful penalties and the prospect of jail time for company heads who are responsible for such activity become commonplace, companies will continue defrauding the Government and putting patients’ lives in danger.
Numerous studies have found that when corporations foot the bill, research is more likely to come up with results that support new drugs. In other words, there is now overwhelming evidence that drug companies manipulate the research. Companies test their own medicines, so testing is cleverly designed to emphasise benefits and understate harms. Negative trials have not always been published. They can get away with this because of inadequate regulation.
The pharmaceutical industry spends more than any other industry on lobbying the U.S. Government, spending $280 million in 2018. The purpose of this is to keep regulation of the industry favourable to its interests. The U.S. regulator is called the Food and Drug Administration (FDA). It is underfunded, has shown little interest in safety and has no ongoing, long-term safety analysis. It also has serious conflicts of interest, with many staff connected to the industry. The former FDA chief went to work for the drug company, Pfizer. Many former members of the U.S. Congress have taken jobs as lobbyists for the pharmaceutical industry.
Astonishingly, the regulatory situation in Britain is even worse. The U.K. regulator (MHRA) has not successfully prosecuted a single firm, and the fines total just £73,300. The regulator boasted in 2012 of having given 467 warnings and 151 cautions, but these have no effect. Laws and regulations are not enforced, and conflicts of interest exist throughout the whole drug approval system.
All of these factors have been at work during Covid. There is increasing concern that the World Health Organisation (WHO) has been captured by pharmaceutical interests. There is also evidence that university research has been manipulated by funders. The profit motive in the hands of companies with immense power seems to corrupt everything it touches. The injections that are labelled ‘vaccines’ are described by governments and manufacturers as ‘safe and effective’, yet the evidence shows that the claimed effectiveness has been hugely exaggerated, the short term harms have been greater than claimed and the long term harms remain unknown. Governments have paid huge amounts to private companies, such as Pfizer, for these experimental drugs, giving shareholders and executives a free lunch beyond their wildest dreams. They have indemnified the companies against liability for any harms from the drugs, diminishing their incentive to ensure they are safe.
Within the pharmaceutical system, the focus on corporate profit, rather than medical need, tends to push in the wrong direction, creating perverse incentives. In other words, profit-seeking companies will always try to claim that their medicines are more effective and less harmful than is actually the case, and they can earn more profits by committing bribery and fraud. The pharmaceutical industry is a glaring example of an industry that is ‘not fit for purpose’. It fails the populations of both rich and poor countries.
Possible Solutions?
I should stress that in discussing solutions I have no strong ideological bias towards markets or state. All successful economies have been combinations of the two. The main goal with the pharmaceutical system should be to eliminate financial motives to manipulate drug trials and minimise the expenditure on marketing. This might require an organisation that is not profit-orientated being responsible for the large-scale testing of possible medicines. This would have to be much more transparent than existing research carried out by private companies. Pharmaceuticals might be one area where the elimination of patents would benefit society, so there would be no overpriced medicines or windfall profits. (I’ll write an article about more general problems with patents in the future.) All successful drugs, developed mainly via public means, would be available to every country to make as cheaply as possible. Private companies could still participate in other aspects of the process, such as early research or manufacturing drugs.
There have been debates for generations about whether the system should be partly nationalised and these have resurfaced recently. Proponents suggest that this could provide the same medicines for a fraction of the cost. There would be no financial incentive to commit fraud or bribery, no copycat drugs, no expensive marketing, no lobbying, no legal battles over patents and no depriving poor countries of medicines. But would there be perverse political and bureaucratic incentives in their place, to appear successful and hide failure? Would public bodies do a better job of developing the drugs we need?
If you have any thoughts on the best way to reform the pharmaceutical industry, let us know.









To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
For a start, the Pharmaceutical companies must never again be indemnified by Governments against claims for damages for one of their products. The potential penalties for marketing a poorly tested, dangerous product must be prohibitive.
As we are currently seeing, the families of those who have been killed by the gene therapies and those who have been permanently disabled or injured, have no recourse to the Pharmaceutical companies and the Government’s which coerced the population to take the product are basically refusing to admit they have caused any harm, even as their own monitoring systems are sky-rocketing with deaths and injuries and Coroners are recording that death was caused by the “vaccine.”
I’m assuming our friend making the one and only thumbs down is one of the executives of big Pharma.
A good article, which sets things out ‘fairly’…and that’s the problem…that fairness goes one way..and in my opinion the wrong way…..
Like many people I have probably thought, or never given much thought in the past, to pharmaceuticals.. believing my doctor when they said I needed something.
But I now honestly believe ‘fairness and honesty’ just isn’t in their lexicon….they will do anything…and I do mean anything to make money and to push their products, and if it maims injures and kills…so what? They genuinely don’t care…that much is obvious, both from the history you’ve mentioned to the Covid fiasco…The collusion with Governmental bodies is now so intertwined that there isn’t a chance of it ever being fair or independent.
(The TV programme ‘Dopesick’ shows this brilliantly)…
In light of the Pfizer papers one might think eyes had been opened, that ‘fairness’ might have crept in…that they might take a break to assess things….hahaha…but they are still jabbing with gusto….any day now from six months old for goodness sake…and in light of evidence to the contrary they are still telling pregnant women it’s safe!!
It’s like asking Nazzis to take a minute to reflect on their policies…They are liars, untrustworthy, and don’t give a fig who they harm and kill…it really is that plain to see.
but if you don’t want to see it you won’t….
I have no intention now or ever of giving them a ‘pass’…and I’m afraid when ALL snouts are so firmly in the trough they don’t see the problem or want a solution either..everything from their perspective is hunky-dory.
There is no question now that Bozo and his comrades are wholly complicit. They knew these injections were unsafe but still allowed, and continue to allow, indeed push their use. Bozo and Co should be first in the dock.
The charge street will be the longest in British history.
“There is no question now that Bozo and his comrades are wholly complicit.”
His comrades include those in allegedly ‘opposition’ parties who have fully supported the government in this crime against the people…and then we have the despicable actions of the ‘caring’ NHS which has wantonly taken on the key role in the massive indefensible charade…
To reminisce
https://childrenshealthdefense.org/news/response-to-the-british-government-proposal-to-roll-out-a-covd-19-vaccine-before-christmas/
1) There should be executive criminal liability ie people should go to jail for life
2) Penalties and fines for companies should be large enough to affect their ability to trade
3) In the UK companies are effectively protected from legal suits by the politicised Legal Aid Agency – this should stop. In the UK citizens were unable even to sue Merck over the notorious Vioxx
4) If we are going to have licensing agencies they should do a proper independent job not the present sham which confuses the public about safety
5) Otherwise get rid of licensing and make suing the companies easy if they misrepresent things.
A wise article. A major problem now is the fact that at the governmental level, there is no independent organisation acting in the public interest. Instead, they seem to be operating on the commercial side of the field, encouraging the use of trial products, from “free” advertising to insurance (via granting financial immunity) for any damage done.
Excellent article. Thank you.
It’s very hard to suggest how to reform a system that is so completely broken.
Change is only likely to happen from the bottom up. So reforming medical training has to be an important element. Medical training needs to completely independent of the pharmaceutical industry. And that training needs to emphasise the importance of extreme sceptism of the pharmaceutical industry with all it’s corruption, perverse incentives and conflicts of interest. The training needs to emphasise the importance of identifying the root cause of chronic illnesses rather than identifying pharmaceutical interventions to mask symptoms. The training for chronic illness needs to concentrate on lifestyle interventions such as nutrition as a much better alternative to pharmaceutical drugs for chronic illness. And that nutrition training must be independent of the arguably equally corrupt processed food industry. At the moment clinicians are largely trained representatives of the pharmaceutical industry. As I understand it doctors get next to no training on nutrition.
Incidentally this video covering statins by Maryanne Demasi is a good case study that shows everything that is wrong with the pharmaceutical industry and the whole eco system that relies on them.
Great link, thanks. My scepticism is spreading to all aspects of healthcare.
Also thought this was an excellent article.Having worked in the NHS for over 30 years as a clinician & trainer before retiring, I have seen numerous treatments and interventions be introduced with high expectations, only to lose favour as the side effects and lower than anticipated outcomes emerge. This was really brought home to me working in the management of long-term pain and being clinically involved with people experiencing dependency and addiction problems after being prescribed opioids. I know this has been said numerous times but I have found it hard to understand the lack of critical thinking when it comes to the vaccine rollout & the levels of coercion involved. It is sites like this that have provided some sort of balance amongst the mayhem. I do have concerns about the new format and already feel that the flow of information has been reduced now a donation is required to comment. Can appreciated the need to generate income but for me the comments were as least as important as the articles.
The lack of critical thinking isn’t that strange, most people don’t care to think too hard, just makes life more difficult. Certainly when the so-called regulatory bodies that are supposedly there to protect us from the profit seekers keep maintaining that the vaxx is safe and effective. Even a fool can see that the claim of safety is extremely dubious and the claim of effectiveness starting to sound like a bad joke, but as long as responsibility can be placed with the regulatory agency, most people refuse to think beyond that. At this point I’m not sure who I despise more, the profit seeking pharma companies or the shameless sell-outs that call themselves regulatory bodies.
As for your latter point, I wholeheartedly agree. The comments BTL are a big draw to this site, even for people who don’t comment – or, more likely, take a while before getting around to commenting – I was lurking on the site for about 3 months before I got an account.
Some people commenting had made the point that they had lost jobs / businesses during the lockdowns, perhaps for some 5 pounds may still be more than they can afford. I too understand that income is necessary, but is there not a better way? I know I felt this seemed to be dropped on us, it might have helped to say this was coming (if it was stated somewhere beforehand and I missed it, my apologies). It might also be an idea to provide an option of paying a 3 month or 6 month amount? Maybe an option to donate on someone else’s behalf? I read of someone doing that on one of the substacks.
I don’t think it’s always about the money. Donating to a website involves identifying yourself, so maybe some people are concerned about privacy. But we need to be bold.
An annual payment option (as on many substack accounts) would be good, and it would bring in money up front.
Yes, I agree with the privacy issue and donations. This raises the issue of things like privacy policies etc. The downside is that levels of bureaucracy get higher & higher & regulation increases. Something of a double-edged sword with the sense that something important has been lost. I do think there needs to be an option to delete account information. I for one, don’t like my details being held ad-infinitum.
This site is so important it needs to be sustainable. It also needs to expand and add even more smart journalists and researchers. There are very few sites in the world providing the service as this site. Its mission is going to become even more important going forward (when increasing censorship will try to stifle all debate).
As such, IMO, it is imperative that this site has some kind of financial security.
I do agree that the loss of comments is lamentable, but I don’t know how the site can continue indefinitely – at a high quality – absent some steady revenue streams.
Maybe the subscription or donation minimum could be reduced?
I’ve noted that many mainstream news organizations have inflated their “paid subscriber” numbers by offering $1/month subscriptions for, say, four months. This seems to have worked. I mean $1/month is the same as 50 cents/month a couple of years ago – which would be about a penny a day.
People need to have some “skin in the game” if even it’s just a few cells of skin .. because “the game” ain’t no game anymore.
Cerezyme at $200K a year is not actually a particularly extreme example. There’s a common protein folding disorder ATTR amyloidosis for which there are I think 3 official treatments costing between $215K and $450K annually. Alternatively, there’s green tea extract or curcumin (turmeric), both of which showed considerable promise for halting and reversing the underlying pathology in shoestring preclinical studies a few years back; of course in the current system they won’t be investigated further. Were we ever to abolish pharmaceutical patents and the perverse incentives they create, there are a lot of potential low cost treatments out there.
That would be my idea as well: Abolish patents on so-called intellectual property. The term is already a misnomer as property is always something physcial no two people can own at the same time. Ideas are not physical, they can be shared freely without diminuishing their value to each individual.
The ideal way to reform the pharma industry would just be to abolish pharmaceutical patents, which are a relatively recent invention, with some European countries such as Italy only recognising them in the 1970s. With the exception of trade marks, disrespect of which is a form of identity fraud, “intellectual property” is not required for free markets to flourish, indeed it often stifles the very innovation it is claimed to promote. See for example the book Against Intellectual Monopoly, available here for free: http://dklevine.com/general/intellectual/againstnew.htm
The problem is bigger than this.
Our entire financial system is based around sales and profit and ‘short termism’.
We have had housing bubbles, off-shoring, wars, tech bubbles, gyms, health emergencies, space, year 2000 etc etc (feel free to add your own). The pharma financial complex is integral to pension funds and making the money go round.
I worked with a pharmacist years ago and he had worked in development and said that they were finding new chemicals almost on a weekly basis. The expectation was that would continue, but it didn’t. Since the 1980’s new drugs which actually do some good have become a bit of a rarity. Patents for slightly modified line extensions of existing drugs prolonged sales as did marking up prices for generics (Shkreli is out of prison now BTW).
The drugs that have been ‘invented’ have often been shown to have limited efficacy and lots of side effects and are becoming increasingly more expensive to produce (a bit like digging up coal).
The governments are forced to support the activities that generate money and quash any that don’t.
I think they have justified it to themselves for the following reasons:
So we get:
Specifically on the question above in relation to Pharma, my suggestions are:
1.Disband NICE. Provide information to doctors not guidance and allow comments so that doctors can get a range of opinions on treatments and then decide what is best for the patient. Such comments to be uncensored.
2.Halt the vax schedules for all injections and carry out studies to look at the difference between injected and not injected (without placebo at all).
3.Change the way that the vax efficacy calculations are done so that the absolute value is used not the relative value.
4.Set up a government production unit for generics.
5.Review all funding programmes currently ongoing in universities and ensure that where funding is given that it is not subject to external influence. Where funding is given half of that must be given free of any controls for research institutions to us as they see fit on their own projects.
6.Where research institutions have carried out research or development work of a product they must be legally entitled to a percentage share in any later sales. Where the work is government funded it must come back to the government.
7.Liability has to be held by manufacturers.
8.Holistic and naturopath practices to be supported.
9.Ban all research on human gene therapy products.
10.Research programme must state clearly who is providing funding, donors must not be permitted to fund projects that compete against each other (this is just a form of hedge funding).
11.Immediately pull all NGO’s into regulatory control and if turnover exceeds 1m tax them as a company. That these huge organisations have no real oversight is appalling.
I can dream….
With this development in Australia, pharma & governments will be committing further crimes against humanity.
Bodily autonomy? Forget it!
Nuremburg Code for Doctors Ethics re experimental medicine? What code???
https://worldtruth.tv/australia-to-forcibly-vaccinate-citizens-via-chemtrails/?amp=1
Suppression of alternative treatments, but especially silencing of preventative measures, by big pharma for disease ensures that they always have a ready supply of profitable customers. Interesting article on some of those cheaper alternatives
https://greenmedinfo.com/blog/6-bodily-tissues-can-be-regenerated-through-nutrition1?utm_campaign=Daily%20Newsletter%3A%206%20Bodily%20Tissues%20That%20Can%20Be%20Regenerated%20Through%20Nutrition%20%28QWVteb%29&utm_medium=email&utm_source=Daily%20Newsletter%20Sends-%20Updated&_kx=wjclBKoUFUBPS9g773etL09PHMLiMauxjdDIFTdRYnM%3D.K2vXAy
My Father used to maintain that the cure for cancer is already locked in a cupboard somewhere. There’s no money in curing diseases, only in treating them…
It’s actually worse: Imagine someone could cure cancer. Would the non-smoker and teetotaller lobbying organizations who are both politically powerful and very well connected be amused about that? Or would they rather try to to bury this disinformation together with the person who dared spread it as quickly as possible?
Cancer is the universal bogeyman everyone with a health-chip on his shoulders uses to justify his set of lifestyle commandments. Many of the people who are adamant about this work in the medical sector or rather, in the public health sector. They wouldn’t want to let go of their settled science. Certainly not if it meant people doing things they despise would nevertheless be living longer and in better health.
The MHRA stepped in to protect the best interests of their cronies in this instance:
https://www.ukcolumn.org/article/gcmaf-and-persecution-david-noakes-lyn-thyer-immuno-biotech
In my opinion, the pharma industry is a bunch of vultures feeding of a carcass someone else put in place. A cure or effective treatment (in the sense of manageing it) or even just serious research into cancer is politically undesired. Cancer is the just punishment for people making the wrong lifestyle choices, smoking, consuming alcoholic drinks and eating wrong things (like bacon). As these sinners must be forced to repent, there are ever increasing sin taxes supposed to effect that. That the government makes a handy sum from these is certainly just coincidence.
If the NHS (a government agency) was interested in curing cancer (instead of using it to browbeat sinners into submission), the pharma industry would provide a (doubtlessly patented and very expensive) cure. The government would make sure that it can be patented, even if it was stuff from undergraduate biology books which has been known for centuries.
“My Father used to maintain that the cure for cancer is already locked in a cupboard somewhere.”
I have been reliably informed that is indeed the case.
Still, if your “company” has an income of £640 million tax free and your head honcho takes home a very relaxing £240 k per year there isn’t really much point in spoiling the jamboree by announcing that cures for cancer have been known about for decades.
Cancer Research UK. My apologies.
We should remember that big pharma only get away with their crimes because governments and government agencies turn a blind eye, while much of the media has been bought off too. Read Robert Kennedy Jr’s book “The Real Anthony Fauci” to get a better picture of the corruption in the world of the pharma mafia. Money talks, and Fauci and Gates have together been involved in many highly dubious activities to say the least. The covid clot shots are the culmination of years spent perfecting their double act to dupe the entire world into believing in the existential threat of covid and that their “vaccines” are the only way back to normality. That these two men aren’t behind bars for life is disturbing in itself.
I think Horton says such things to enhance his own credibility but doesn’t remotely care. You think because he’s said it that Lancet is a good brand!
A lot of this one sided commentary applies to the USA, not the UK. There are errors over HERE, the MHRA approving the poisonous and useless Covid ‘vaccines’, but the Government controls prices and price gouging is not as common as is made out in the article.
What happens in the UK is that NICE, which vets treatments for the NHS, doesn’t approve the $400K a year treatment so you are still left to pay the $400K; I’ve contributed to a number of crowdfunding campaigns to fund expensive medication. But yes, the US has its own unique anti-competition laws that enable their healthcare system to charge absurd prices even for standard medicines. At least the UK has a more or less free market in standard medicines.
Some discussion here: https://lowdownnhs.info/drugs/billions-are-spent-by-the-nhs-on-drugs-every-year-but-how-does-it-work/ on the NHS’s purchasing power and how it helps to keep drug costs down.
The considerable purchasing power of the NHS can somewhat reduce the cost of a given expensive drug but what it doesn’t address is the bias of the drug development process itself towards expensive, dangerous and ineffective drugs that can be patented, and away from cheap, safe and effective drugs and non-drug treatments that cannot be patented. In fact as we’ve seen from the response to COVID, the NHS colludes with and promotes that bias.
Medicines take up around 14% of the NHS budget, just as they have since the late 1960s. Also, marketing excesses have been brought under control by the ABPI
Most manufactured items have become far cheaper since the late 1960s, even after massive innovation and improvement. There’s something very wrong with a system that approves Remdesivir for COVID and doesn’t approve fluvoxamine.
https://expose-news.com/2022/06/15/vaccinated-4-in-5-covid-deaths-canada-since-feb/
It is now quite evident from the covid panicdema that the goals of big pharma are: to get all vaccines mandated, to be protected against all liability and to have them all funded directly from government treasuries. The sums of money involved are staggering and so the funds available for influencing public health officials and politicians is enormous. Sadly IMO this will have a very negative outcome on the whole vaccine industry and trust in the Medicall Profession generally. I am not sure trust in politicians can get much lower.
This generation’s Thalidomide
This is an excellent article. There is so much evidence that the public are being harmed but what I find most alarming is how the Government and pharmaceutical companies get away with all this evidence being covered up. I believe (maybe naively) that the vast majority of humans are well-meaning and wish to do no harm to others, so how can there not be enough of these human beings in the world wealthy and powerful enough to bring successful legal action within a reasonably quick time frame? We have irrefutable, damning evidence against those responsible for hiding all this information from the public. This is what puzzles me the most. I’m an optimist, please help me.