Some recently published scientific papers explore the longer term consequences of Covid. Yesterday, I looked at one which considers the impact of vaccination, finding no robust support for the claim that vaccination reduces the risk of Covid after-effects but highlighting a worrying vaccine safety signal which the authors had failed to mention. Today I will look at four other papers. In summary, I conclude that:
- Vaccinated individuals get sequelae (after-effects) in the months following Covid infection.
- Some of these sequelae are serious.
- The most common sequelae are, however, fatigue and loss of smell.
- People that get symptomatic Covid that requires them to seek support from healthcare professionals appear to have high levels of sequelae.
- There are no supporting data on whether vaccination reduces the risk of sequelae following Covid infection.
- There appears to be a high risk of vaccine side effects in the weeks and months following vaccination.
- The CDC likes to scare people.
This is a great paper – it is really well done and bases its analysis on a matched cohort, the best way to undertake studies like this. Sure, it is a retrospective study not a prospective study, but that’s to be expected given that authorities worldwide started jabbing people without any attempt to understand what the consequences might be. Well, I say that it is great, but unfortunately it suffers a significant flaw that spoils everything – more on that in a minute.
This study looked at Covid infections in around about 100,000 individuals that sought healthcare assistance in the months following their infection, some of whom were vaccinated. They then matched the general characteristics (age, sex, ethnicity, health-related issues) and date of infection of the vaccinated and unvaccinated to get 9,479 ‘matches’ – that is, each infected vaccinated person was matched with an unvaccinated individual that was ‘similar’ and who had his or her Covid infection at around about the same time.
Their data appear pretty conclusive.
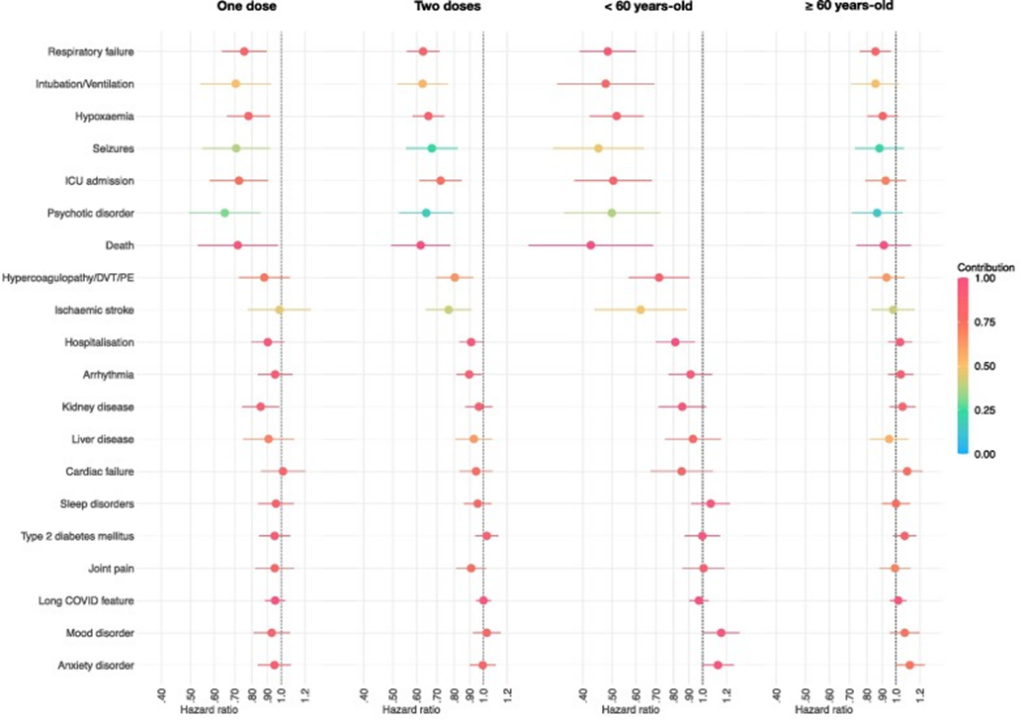
The two graphs on the left (for sequelae (disease after-effects) hazard ratio for one and two doses of vaccine) suggest that there’s much less risk of a large range of post-infection sequelae in the vaccinated compared with the unvaccinated, with lower risk for those having taken two doses of vaccines.
More interesting are the graphs on the right – these suggest that all the benefits are in those aged under 60, with practically no benefit for those aged over 60. This would be a shame, because it is those aged over 60 that suffer the greatest risk from Covid; while there appear to be benefits for those aged under 60, these individuals are at lower risk from these health outcomes anyway, and the reduction in risk apparently offered by the vaccines is perhaps of less relevance.
An important part of those graphs are the data for ‘Long Covid feature’, a set of broad symptoms that have been identified by others as ‘Long Covid’ – abdominal symptoms, abnormal breathing, anxiety/depression, chest/throat pain, cognitive symptoms, fatigue, myalgia, ‘other pain’. This statistical analysis found no difference in the incidence of ‘Long Covid’ in the vaccinated versus unvaccinated, suggesting that vaccination doesn’t help reduce the risk of Long Covid.
Ah, but what about the big flaw? For some reason this study, like the study I examined in my previous post, also included those that had been vaccinated after their Covid infection in their ‘unvaccinated’ cohort. Again, the authors don’t indicate the proportion of ‘unvaccinated’ that were vaccinated after infection, but given the very high take up of vaccination in the USA, this is very likely to apply to the majority of those in the ‘unvaccinated’ group. Unlike the previous study, the authors don’t give us information on the average period between vaccination and infection; all we know is that it was at least 42 days (individuals weren’t considered as vaccinated until 14 days after vaccination, plus the data in the study were only gathered from 28 days after infection to remove acute Covid symptoms from their analysis).
Thus, while the study declares itself to be an analysis of sequelae in vaccinated compared with unvaccinated, the reality is actually a comparison of:
- Infection sequelae and vaccine side-effects that occur no sooner than 42 days after vaccination and probably much longer, and ignoring sequelae/side-effects that occurred within 28 days of infection;
versus
- Infection sequelae and vaccine side-effects in a population that is mostly vaccinated, including any sequelae that occur in the short and medium term after vaccination (including same-day side effects), and ignoring sequelae/side-effects that occurred within 28 days of infection.
What’s particularly notable is that there appears to be no difference between vaccinated and ‘unvaccinated’ cohorts at greater than four months after infection; I suggest that this is because most of the ‘unvaccinated’ cohort had become vaccinated by this point and had already suffered the high risk period for vaccine side-effects in the weeks following vaccination.
I find this such a shame, because they’d started so well in their use of a matched cohort study design. Perhaps it is too much to ask that they redo their analysis with only truly unvaccinated individuals in their ‘unvaccinated’ cohort.
Summary:
- A great start spoiled by a strange choice of cohorts.
- The data don’t give any useable information on the incidence of sequelae in vaccinated versus truly unvaccinated individuals, despite the study title.
- The results suggest that if you include the period immediately after vaccination you find significantly more negative health consequences compared with ‘similar’ individuals some time after vaccination.
- Or, to put it more succinctly, this is exactly the result you’d expect to find if there were significant levels of side-effects after vaccination.
I quite like this paper – it is nice and simple, and doesn’t try to be something it isn’t. The purpose of the analysis is exactly as described in the title:
- They looked for factors associated with post Covid sequelae. Note not incidence rates or the impact of vaccination; simply what factors seem to be associated with problems after Covid infection.
- They looked at data from inpatients and outpatients – thus the data were taken from people who were sufficiently ill with Covid to seek the support of their healthcare provider, not simply those infected with Covid.
- They used a diverse cohort – that is, they included lots of different types of people in their analysis in an attempt to discover if some people were more at risk of problems after Covid infection.
Sure, there’s no control group, no ‘unvaccinated group’ and no attempt to identify more serious sequelae after Covid infection – but those weren’t necessary for the authors to explore the aspect of the data that were of interest to them.
The study found that approximately a third of their sample population had problems that could be described as ‘Long Covid’ six to nine months after Covid infection. These problems were mainly fatigue, loss of taste/smell, shortness of breath and possibly chest pain. Fatigue was the main problem found.
While they found long-term problems in a third of the people that took part in the study, this must be interpreted in conjunction with the types of people included in the study – either those hospitalised with Covid or those not hospitalised but who were deemed to be “clinically high risk by their primary care providers”.
There are some that have said that this study shows that ‘Long Covid’ affects a third of those infected with Covid, but the study itself makes no such claim – it merely states that a third of the types of people included in the study developed ‘Long Covid’.
The main outcome of the study was that there didn’t seem to be any pattern in those developing Long Covid – individuals included in the study seemed to be at the same risk of developing Long Covid no matter their race, socio-economic group or fitness level. The study didn’t offer any data on the incidence of sequelae in healthy individuals in the period after Covid infection.
Summary:
- A decent paper that sticks to its remit and doesn’t try to make inferences outside of the study data.
- People who read the paper and yell that a third of those infected with Covid develop Long Covid are misunderstanding the paper and its results.
This is an interesting paper but only because it records the first stage of a long term study (‘longitudinal’). Its findings can only really be interpreted in this context. When the study reports that 55% of the infected group have symptoms consistent with Long Covid at the start of this long-term study (‘baseline’) it only applies to the types of people that enrolled in the study based on it being an investigation into Long-Covid i.e., people that already had concerns about their health after infection with Covid would be much more likely to want to take part in the study than those that had no sequelae. Indeed, considering the study design, a reasonable interpretation might be that this aspect of the study merely suggests that the other 45% of individuals that enrolled in the study thought that they had Long Covid but didn’t actually have anything wrong with them.
Nevertheless, the study did find some interesting results even at this baseline stage. Approximately one quarter of the unvaccinated infected had no antibodies to the N-protein at the point of testing, whereas 100% of the vaccinated had these antibodies. As the unvaccinated-infected had completely recovered from their infection this suggests that antibodies aren’t essential to clear Covid (i.e., the infection was cleared by innate or cellular immunity) but that vaccination biases the immune system to try to use antibodies to control the infection (which might actually be cleared using cellular immunity, despite the presence of antibodies). This is consistent with investigations into coronaviruses (‘colds’) undertaken prior to 2020, which indicated that antibodies were a relatively unimportant factor in the clearing of coronavirus infections.
The main output of the study (which created a bit of a social media feeding frenzy) was that it found that the presence of Long Covid wasn’t associated with any physiological markers i.e., they couldn’t find anything ‘wrong’ with the individuals with Long Covid to explain their symptoms. However, they did find that those with symptoms of Long Covid were much more likely to have a history of ‘anxiety’ prior to 2020. It has been suggested that this means that Long Covid doesn’t exist other than in the minds of the individuals concerned; this isn’t quite fair – the results simply show that they couldn’t find anything wrong with the individuals. It is quite possible that they simply didn’t manage to identify what was wrong with the individuals.
This is a longitudinal study; it’ll be interesting to see what the next update to the study finds.
Summary:
- This is a paper describing the characteristics of a set of people that the researchers are going to keep track of for the coming months and perhaps years.
- It doesn’t show that 55% of people that had Covid are suffering from Long Covid.
- It also doesn’t show that those suffering with Long Covid have nothing wrong with them other than being highly anxious (this is only one possibility and there are others).
I don’t like this paper from the U.S. CDC. It seems like they’ve tried very hard to make Long Covid appear as a terrible affliction that’s blighting a large proportion of those infected with Covid. I’ll cut and paste part of their abstract and embolden parts that illustrate this:
Among all patients aged ≥18 years, 38% of case-patients experienced an incident condition compared with 16% of controls; conditions affected multiple systems, and included cardiovascular, pulmonary, hematologic, renal, endocrine, gastrointestinal, musculoskeletal, neurologic, and psychiatric signs and symptoms. By age group, the highest risk ratios (RRs) were for acute pulmonary embolism (RR = 2.1 and 2.2 among persons aged 18–64 and ≥65 years, respectively) and respiratory signs and symptoms (RR = 2.1 in both age groups). Among those aged 18-64 years, 35.4% of case-patients experienced an incident condition compared with 14.6% of controls. Among those aged ≥65 years, 45.4% of case-patients experienced an incident condition compared with 18.5% of controls. These findings translate to one in five COVID-19 survivors aged 18–64 years, and one in four survivors aged ≥65 years experiencing an incident condition that might be attributable to previous COVID-19.
That sounds absolutely dreadful.
The problem is that they don’t put these risks into a real-world context. Sure, pulmonary embolism risk might well be doubled after Covid infection, but it isn’t a common condition to start with and it certainly won’t be the case that a quarter of those having suffered Covid infection will go on to suffer a pulmonary embolism. It is most likely that the vast majority of their ‘high percentage’ that suffer ‘Long Covid’ are suffering a mild fatigue, disturbed sleep and ongoing problems with smell-taste. The huge problem with the paper is that they don’t actually say this anywhere.
There are other problems with the paper:
- They only looked at people that had a Covid infection with sufficiently serious symptoms to warrant interaction with their healthcare provider. They don’t give any information at all on the incidence of Long Covid for those with mild disease that cleared without healthcare support (i.e., the majority of individuals).
- While they track Long Covid from 30-265 days after infection, they don’t report on how the Long Covid risk changes over this period. It is very common for people with a viral infection serious enough to warrant seeking support from their healthcare provider (some of whom are admitted to hospital) to have lingering ill-defined symptoms in the weeks following recovery. This study would have been stronger if they’d reported the risk for different periods after infection, or simply ‘started the clock’ at 60 days instead of 30 days. As it stands it is likely that a good proportion of those suffering ‘Long Covid’ had their symptoms clear up by 60 to 90 days after infection.
It is a shame that the authors used this paper to present scary statistics about Long Covid. There are clearly useful data in there; even if the more common symptoms of Long Covid are relatively benign (fatigue, loss of smell) and only last a few months, they’re still real and concerning to those affected. It would have been more useful if the paper had spent more effort in describing the real-world implications of their findings, including absolute rates (not relative) and the timescales for recovery.
Summary:
LONG COVID IS VERY SCARY AND DON’T YOU FORGET IT.
Conclusions
These four papers and the one I looked at previously, published over the last two months, have been used to support claims that Long Covid is a common condition in the months after infection, and that the vaccines reduce the risk of Long Covid occurring.
This analysis of the detail available in the papers suggests that these interpretations are not supported by the data.
The main conclusions that should be reached from these papers is that:
- Vaccinated individuals get sequelae in the months following Covid infection.
- Some of these sequelae are serious.
- The most common sequelae are, however, fatigue and loss of smell.
- People that get symptomatic Covid that requires them to seek support from healthcare professionals appear to have high levels of sequelae.
- There are no supporting data on whether vaccination reduces the risk of sequelae following Covid infection.
- There appears to be a high risk of vaccine side effects in the weeks and months following vaccination.
- The CDC likes to scare people.
Amanuensis is an ex-academic and senior Government scientist. He blogs at Bartram’s Folly.












To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.