On August 31st, a new randomised controlled trial on mask efficacy was published online. This study is the first of its kind. While the well-known Danish mask study looked at whether wearing a mask reduces one’s own risk of infection, the new study looked at whether community masking reduces the general level of infection.
The main argument for wearing a mask has always been that it makes infected people less likely to transmit the virus, rather than it provides any protection to the wearer. Hence the new study is a far more valid test of the claim that community masking ‘works’.
As I’ll explain, however, it’s a missed opportunity. And this is a shame because some aspects of the experimental design are quite powerful, and – given the number of people involved – it must have been very expensive (meaning there’s now less money available for the next big study).
The basic set-up was as follows. The authors randomly assigned 600 villages in rural Bangladesh – comprising more than 300,000 people – to one of two groups: an intervention group and a control group.
Villages in the intervention group received an eight-week mask promotion campaign, which involved distribution of masks, promotion of masks in public spaces, and role-modelling by community leaders (including imams at local mosques). Villages in the control group did not receive any interventions.
The main outcome variables were measures of seroprevalence. Using phone and in-person surveys, the researchers obtained data on the number of people who experienced COVID-19 symptoms after the intervention. They then collected blood samples from some of those individuals to gauge the number who were seropositive.
Overall, mask-wearing reached 42.3% in the intervention villages, compared to 13.3% in the control villages. What about the outcome variables? 7.6% of participants in the intervention villages reported COVID-19 symptoms, compared to 8.6% in the control villages.
And when the researchers zoomed in on those who reported COVID-19 symptoms and tested positive for antibodies, the seroprevalence was 0.68% in the intervention villages, versus 0.76% in the control villages. (Note: the figure in the chart below is ‘0.69’ because it’s an adjusted value from a model.)
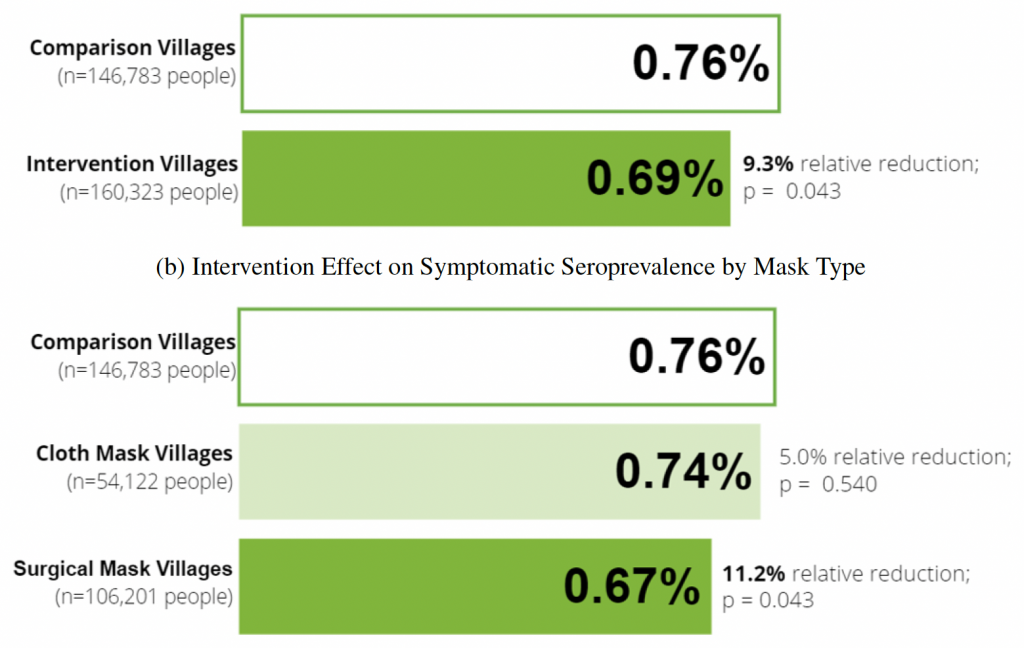
Among the intervention villages, some had been randomly assigned to get cloth masks, whereas others had been randomly assigned to get surgical masks. The researchers compared these two groups, and found that the reduction in seroprevalence was larger for the surgical mask group. They also found that the reduction was concentrated among individuals aged 50+ (see p.28).
Given that the intervention increased mask-wearing by 29 percentage points, the results suggest that going from 0% to 100% mask-wearing could reduce the seroprevalence of COVID-19 by as much as 36%. (That is, 100/29 x [0.76 – 0.68]/0.76.) And the reduction could be even greater for individuals aged 50 and over.
However, there are several weaknesses of the study, which mean that this interpretation is not necessarily correct, and – in fact – may very well be wrong.
One criticism is that the ‘p-values’ corresponding to the main results are rather high (see chart above). Note: a p-value quantifies the degree of statistical confidence one can have in an ‘effect’ of given magnitude; the smaller the value, the more confidence.
Although two out of the three are below the conventional threshold of 0.05, they are only just below it. This raises questions about the robustness of the results. On the other hand, the p-value corresponding to the difference in seroprevalence among those aged 60+ does appear to be quite low.
However, a much more serious criticism is that the study is not actually a randomised trial of mask-wearing. Rather, it is a randomised trial of mask promotion campaigns. This means that, even if the intervention did have an effect, that effect was not necessarily brought about by more people wearing masks.
A true randomised trial of mask-wearing would have had two groups: each receiving the same promotion campaign, except in one group the masks would have been genuine, and in the other they would have been fake (e.g., made out of a more porous material). For ethical reasons, this kind of study might not be allowed.
As an alternative, the researchers could at least have given each of the two groups a ‘COVID-19 awareness campaign’, and then only distributed masks to the intervention group.
Yet in the study itself, the control villages received no interventions. It’s therefore plausible that seroprevalence ended up being lower in the intervention villages not because of greater mask-wearing, but because the campaign made people more concerned about COVID-19 in general, and hence caused them to change their behaviour in other ways.
For example, they might have become more likely to avoid crowds, to ventilate their homes or to stay at home when sick. As a matter of fact, the researchers also measured physical distancing, and found that this was greater in the intervention villages.
One counter-argument is that the greater efficacy of surgical masks than cloth masks suggests the results really are explained by mask-wearing. (Surgical masks appear to be more effective in lab experiments.) However, this result is also consistent with the alternative explanation.
Given that surgical masks are ordinarily worn by healthcare workers or people dealing with hazardous materials, seeing them every day may have prompted greater concern among participants. And in fact, physical distancing increased by slightly more in the intervention villages that received surgical masks. People in those villages may have also changed their behaviour more in ways that weren’t measured.
Some commentators have argued that it doesn’t matter whether the effect came about through greater mask-wearing or other behavioural changes. What matters, they say, is that the mask promotion campaign reduced seroprevalence.
However, this is not a convincing argument. First, while a mask promotion campaign could plausibly affect people’s behaviour in remote Bangladeshi villages, it would be unlikely to have any such impact in countries like the U.K., where the pandemic is already highly salient.
Second, if it was the campaign that mattered, rather than the mask-wearing itself, the same effect could be achieved far more cheaply in the future. For example, rather than distributing thousands of masks to villagers, one could simply inform them about the risks of COVID-19, as well as the importance of social distancing and ventilation.
The Bangladesh mask study could have resolved the debate over whether community masking ‘works’. Unfortunately, it’s a massive missed opportunity. All it really tells us is that promoting mask-wearing while also making the pandemic more salient leads to a reduction in seroprevalence among older people living in rural Bangladesh.











To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
The Guardian ceased to be a neutral investigative paper about 10 years ago when MI6 paid them a visit after they had released some Snowden Files.
It is now run by Head Girls and read only by teachers.
They are sell about 60,000 copies – mainly to the BBC and other leftie organisations – and so were steadily going bankrupt so Bill Gates stepped in to prop them up.
Having, of course, been founded using Taylor’s profits from trading in US cotton…
With slave connections. Nice
https://www.youtube.com/watch?v=79t_gmfue54
Would The Guardian have quit “X” had Trump not won? I reckon not. This looks more like a fit of pique caused by Musk’s support for Trump than any principled stand against the immoral horrors of “X” which have remained consistent since Musk took it over.
If Trump had not won, it is likely that the US Gov’t would increase their on-going investigations and eventual prosecutions of Musk and all his companies. Goal to destroy his businesses and his life, along with same for so many others. Musk risked everything. All In. His style.
A friend commented about X that if you want to know what is really going on it is the only way to get news.
So much for the Grauniad. Throwing their toys out of the pram but taking their ball away so no one else can play with it and them.
Ha, ha, ha, ha, ha.
A fake newspaper if ever I saw one. You cannot get a straight take on anything in the Grauniad so I stopped even looking at it despite being free. After all it is only worth as much as anyone is prepared to pay for it and nowt is my bid.
Nuff said.
Socialists, by their nature, have to be capable of juggling two completely opposite propositions at the same time. Such as their support for gay people, but their support for religious groups who kill gay people. Or, supporting democracy, but not for you, just for their friends. It must be exhausting to live in such a fantasy world where everything matters, but nothing matters..
I have hopes that their heads will explode as a result.
Leftists support democracy – just so long as it comes up with the “correct” result.
A bit like the EU. Remember how they forced countries to re-run the Maastricht referendum if it produced the “wrong result?
Take the Red Pill and the Blue Pill at the same time.
The socialists I know stopped reading The Guardian many years ago when it was taken over by neoliberals.
Socialism is a form of mental illness.
Are your friends(?) receiving appropriate treatment?
As ‘stakeholder’ Blobs … have captured Western government departments and intergovernmental agencies … so ordinary people have been increasingly denied any formal mechanisms for confronting politicians with their grievances.
As the British Left became imbued with Marxism – after the Second world War – it also imbibed the Leninist poison that the working class is comprised of ignorant dolts who should be disenfranchised (and preferably replaced). This is the reason the contemporary marxo-fascists (e.g. The Guardian and its readers) believe that the leadership role in society belongs to “those who know better”. The purpose of this arrangement is to prevent politics from being an arena of public choices.
A fundamental left wing driving force is the march towards some distant Utopia where all social and political and moral aspects are perfect.
And the more recent development is the polarisation into those who are committed to the march, and those who are not. From which it ‘follows’ that those who don’t support the march to perfection must be social, political, and moral enemies.
Many years ago, The Guardian ran a TV advert video showing a skinhead pushing over a well-dressed man walking on the pavement.
The camera would pan out showing the skinhead was saving the man from being crushed by falling bricks.
Their catch line was “there is always two sides to every story”.
Unfortunately, now, The Guardian only show one side of the story and that is of the establishment corporatists and their Globalist, neoliberal, warmongering propaganda.
I used to buy the paper for 35 years and have witnessed its decline.
I stopped buying it about 15 years ago and now only comment on their page every time they get something wrong, which is quite often.
They are probably the most dangerous media outlet as they have this air of respectability and balance when in fact, they promote phony wars, bogus man-made climate change and dangerous vaccines.
I also remember that ad and thought is was very powerful, in fact it often pops into my head when shouty idiots can’t/won’t acknowledge there may be different interpretations of a situation.
I also bought the Guardian but not for well over 40 years.
Similar to me, I stopped buying it about ten years ago.
However I am no longer allowed to comment because I fell foul of their “Community Rules” about four years ago.
Needless to say they wouldn’t/couldn’t tell me precisely why the ban – but I think it just might have been my anti vaccine/bigpharma/Vallance comments. I had quite a few arguments with “Dave 4567” or similar who professed him/her/itself to be A Scientist, but I suspect he may well have been 77th
Yes, I was “moderated” for below the line comments years ago so I just troll them now on facebook.
I went to offGuardian when it first started but ended up being banned for berating the “viruses do not exist” clowns.
Wow! I just found that old Guardian advert on Youtube, using your description, and it is superb! Thanks for that. Here’s the link for those who haven’t seen it, or want to remember it:
The Guardian 1986 Points of View
It’s only when you get the whole picture, you can fully understand what’s going in
is something the people making the Guardian are still perfectly aware of. The 2024 version of this ad would continue with It’s our job to prevent this from ever happening!
Too true!
Establishment media do actually present “the other side” normally.
But they do so dismissively through ridicule, parody and distortion.
Just like the BBC then!
Yes. The BBC relies on the UK government for its funding by allowing it to tax the population with a license. The license is compulsory, and you will be fined if don’t have one. The UK government appoints the Director General. Ergo the BBC is “state funded”, part of the UK and Western world “establishment” and is a very poor news media outlet and far from “independent”.
I used to read it online and comment (in the years running up to the EU Referendum) and, despite my clear right-wing views, which were expressed very politely, I managed to never be censored/banned.
I reckon I’d last about 24 hours if I did that now. Dissent from their worldview is not tolerated.
And so has La Vanguardia in Spain.
What good news from Ben Pile, and a great photo of the Argentinian President Javier Milei!
His leading the Argentinians out of the CPO29 is astonishing and superb.
Why Google’s first reference to just about every single question asked is the Guardian? Why most public sector recruitment ads appear in the Guardian? Why Whitehall mandarins have limitless airtime in the Guardian? Are the BBC and the Guardian related?
“Focus groups and opinion polls have taken the place of dialogue between the public and politicians, and such forums are invariably controlled by Blobbish wonks whose views are narrowed even further by their funders’ priorities.”
Succinctly put. They ignore the masses and then present themselves as somehow “progressive”. Not an ounce of honesty between them.
Trump by name & his name has Trumped Cop (out)29 Fancy arranging this latest Private Jet Fest just as Trump forms his team of realists ! Starmer & Milipede now look like the dumbest arse lickers at this phoney gathering, glorious




Put the Chainsaw to Net Zero
Keep tweeting … and support / keep supporting the non-conformist alternative media/podcasts …. the keyboard and broadcasting warriors who are fighting back on our behalf. Many of them are free. Some charge a small amount – little more than the price of a coffee a month – so you CAN afford it.