It’s not two weeks since Lockdown Sceptics was casting doubt on Public Health England’s alarming claim that the Delta (Indian) variant had more than double the risk of hospitalisation of the Alpha (British) variant. How long will they take to backtrack after the panic has done its damage, we asked?
Well, it turns out that even before Boris took to the podium on Monday PHE had already released a new study claiming that vaccines after all are more effective at preventing hospitalisation against the Delta variant than the Alpha variant. Here’s the story in the Telegraph:
Vaccines are more effective at preventing hospitalisation against the Indian/delta variant than they were against previous types, once people are double-jabbed, new data shows.
Real world data shows the Pfizer/BioNTech vaccine is 94% effective against hospital admission from the variant after one dose, rising to 96% after two jabs.
The Oxford/AstraZeneca vaccine was found to be 71% effective against hospital admission after one dose, rising to 92% after two jabs.
In both cases, two doses had a greater impact preventing hospitalisations than was the case with the Kent variant.
The new study and the earlier study aren’t quite showing the same thing. The earlier study showed the risk of hospitalisation with the Delta versus Alpha variant for all those testing positive, not just the vaccinated, though subsequently adjusted the results for “vaccination status”. The new study specifically looks at the hospitalisation risk in those vaccinated with respect to the Alpha and Delta variants and compares them. However, the two studies should come to broadly the same conclusion, as they are both looking at how much more serious disease is with the Delta variant. At any rate, given that a large proportion of the vulnerable population is now fully vaccinated, we certainly shouldn’t see a doubling in the hospitalisation rate with the Delta variant if, as is claimed in the new study, the vaccines are better at preventing serious disease from that variant.
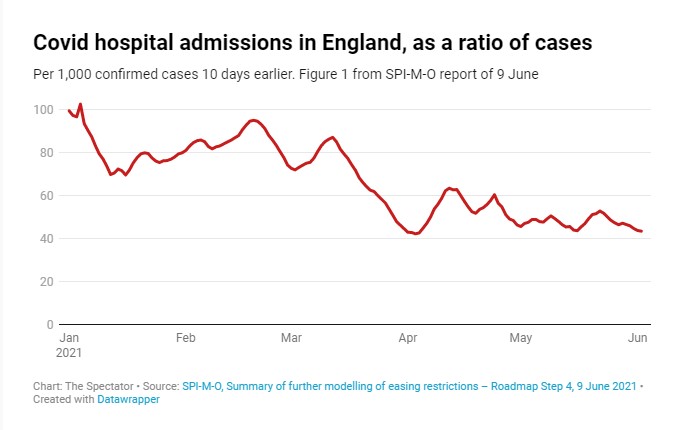
Ross Clark suggests the problem with the earlier data was that the sample size was small and biased. As he notes, PHE’s modelling misses the most obvious data point, that the rate of hospitalisations per case has not increased as the Indian variant has become dominant (see graph below). How then can the Indian variant have twice the risk of hospitalisation?
Is the new study any more reliable than the earlier one? As usual with a PHE observational study, it’s hard to tell, as much of the method is hidden behind opaque statistical techniques with working that is not set out. All the reader knows is that raw data is taken and transformed by some statistical process into hazard ratios and vaccine effectiveness estimates that are all but impossibly to verify. What we can do, though, is look at the results of this largely concealed data-processing and see if it makes sense.
Below is the table from the study (there’s only one, it’s a very short paper), and it shows something very curious.
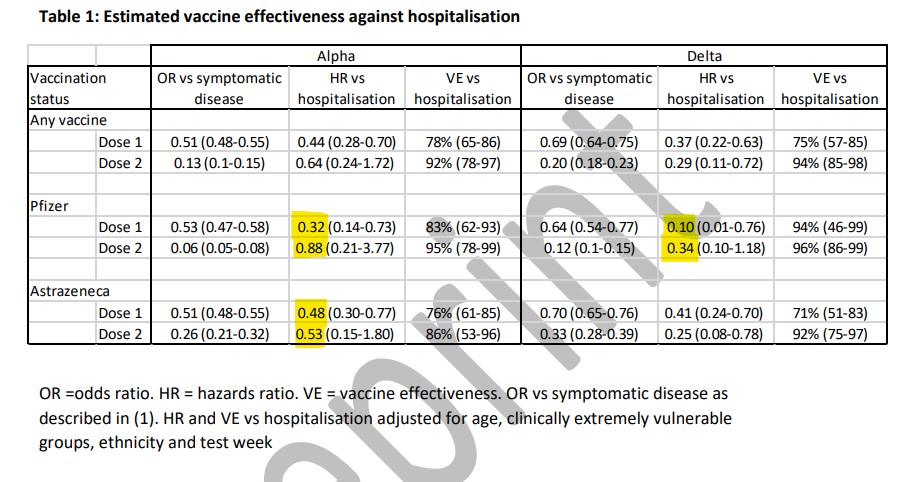
It shows that, once testing positive with the Alpha variant, one dose of Pfizer reduces the risk of hospitalisation by 68% (the 0.32 highlighted), but the second dose only reduces the risk by 12%! That’s 12% in total (the 0.88 highlighted), not 12% on top of the 68%. So the second dose significantly increases your risk of being hospitalised compared to the first dose? That can’t be right. But it’s what it says.
The same thing happens with AstraZeneca against the Alpha variant: the first dose reduces the hospitalisation risk by 52% (the 0.48 highlighted) but the second dose only by 47% (the 0.53). And again with Pfizer against the Delta variant: the first dose reduces hospitalisation risk by 90% (the 0.10), the second dose only by 66% (the 0.34). The only combination where the risk-reductions are the right way round is AstraZeneca against the Delta variant: one dose reduces the risk by 59% (the 0.41 not highlighted under the 0.34) but two doses reduces it by 75% (the 0.25 beneath).
The gaping confidence intervals (0.21-3.77; 0.15-1.80; 0.10-1.18; 0.08-0.78) are also giveaways of a lack of reliability in the findings. For instance, the Pfizer dose-2-against-Alpha confidence interval of 0.21-3.77 means the authors are 95% sure the hospitalisation risk lies somewhere between a reduction of 79% and an increase of 277%! That’s basically meaningless.
How did the authors avoid these blatant red flags in their data and modelling (the hazard ratios are a modelled value) showing up in the headline figures? By keeping the report very short, not discussing the limitations of the study, and only converting to a percentage value (which is readily understood by many people) the overall vaccine effectiveness against hospitalisation (i.e., the risk of hospitalisation-once-infected multiplied by the risk of being infected), while leaving the dubious hospitalisation hazard ratios as an obscure decimal. It seems to have worked: journalists have dutifully reported the headline vaccine effectiveness figures but not queried the strange hazard ratios behind them.
A separate study from Scotland, published as a research letter in the Lancet and reported alongside the PHE study in many places, claims to find the vaccines are a bit less effective against the Delta variant. But it too is heavily adjusted, its positivity figures are all over the place (e.g. the Delta-variant test-positivity for AstraZeneca 13 days after the second dose is nine times as high as for Pfizer) and the confidence intervals again are huge, suggesting a small sample with low confidence.
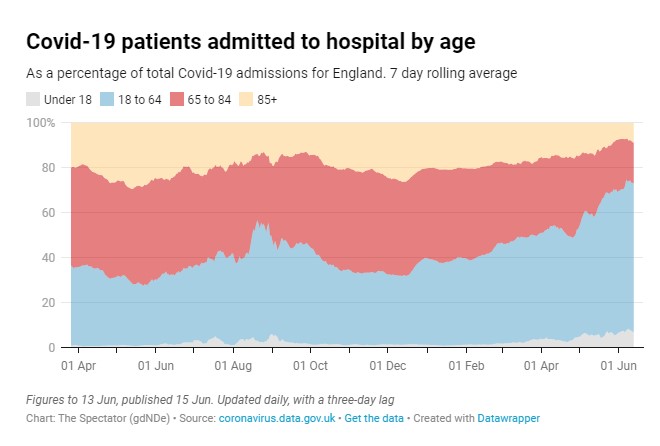
Despite these problems with both studies, I do think the vaccines probably are effective against serious disease to some degree. (Safety is a separate matter.) The reduction in the proportion of Covid hospital admissions in the over 65s in the past few months (see graph below) is perhaps the most striking data point on this. This fits with the detection of antibodies in the blood post-vaccination – if the disease progresses to a systemic stage then the body has additional antibodies to fight it.
I’m less convinced at the moment on how effective the vaccines are against infection and transmission. Almost all the studies on this are confounded by declining background incidence (among other problems). Also, we know the vaccines do not produce mucosal (IgA) antibodies, which have been shown to dominate the early response to SARS-CoV-2. This suggests the defence they offer against infection and mild disease may be less robust. Places with high vaccination rates and high case rates such as Seychelles, Maldives, Bahrain and Chile also suggest the protection against infection may be limited. But perhaps more data and new studies will alter that picture – I’m certainly on the lookout. They’ll have to do better than PHE, though.















To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
“Risk increases after second dose”
So what the hell are the crooks playing at talking about denying dedicated caring staff jobs in care homes for not taking the “dose”?
And did they ever tell us how many people have died within 28 days of “vaccination”?
Either way, it’s a disgrace if people are refused work in care homes for not taking these experimental drugs. And that PHE are being dishonest/shambolic with the statistics.
They are also hounding the lapsed first dosers to get the delayed second dose in order to be ‘protected’.
As I keep stating Hugh, the deeper down this rabbit hole you get, the darker it gets.
This has nothing to do with a virus, public health or saving lives. This is an agenda to commit genocide and enslave what remains of humanity.
My criticism of Peter McColluogh when I first heard him speak was he wasn’t emotional enough. I thought he was another shill “talking head” but I persevered and realized he was actually just being ridiculously calm. He’s now calling the “vaccines” bioterrorism.
Prof. Dr. Luc Montagnier is calling the vaccines a “catastrophe”.
Dr. Yeadon is calling these things a potential “genocidal weapon”.
Sucharit Bhakdi has stated that the “vaccines” will kill everyone who takes them, as has Delores Cahill.
Everyone around here who has been alarmed at the “vaccines” needs to wake up and smell the coffee.
I’ve spent the last month on Twitter talking to some of the best scientists in the world, including a couple from the Fauci emails, and the verdict is the same from ALL of them: the “vaccines” have one purpose – genocide.
These people aren’t wrong. They comprise some of the best epidemiologists, immunologists, virologists and vaccinologists in the world.
Please wake up and see what is happening. These people – including Boris – are full on Globalist eugenicists and they literally DO NOT CARE WHO lives or dies. These f*ckers are playing for ALL the marbles, and the WEF is quite clear in what THEY want humanities’ future to be.
“will kill everyone who takes them”.
Extraordinary and frightening if true”. I don’t understand why they would do that (unless over quite a long period of time) or how they would hide it. Perhaps you could expand on this and provide links?
My reading of it has the following scenarios – pharmaceutical companies seeking profit; climate scare believers seeking to change the climate etc.; Marxists who want a one world government; eugenicists/Malthusians who want population reduction. I seem to remember the Optimum Population Trust talking about a desirable world population of one billion people, so killing 90% would seem a bit strong even for them. What exactly is going on?
and while we’re at it, is it safe to be around “vaccinated” people? are they likely to be breathing out material that could be harmful? (And I’m no scientist or philosopher, so layman’s terms would be helpful)
Of course the snake oil won’t kill everybody. if it was going to do that we’d be seeing the evidence already. But it doesn’t do anybody any good either. Like face knickers, it’s a protection against Fascist persecution and that’s all.
Well, I’d like to think it won’t. Certainly that would be unprecedented. Apparently it is the “booster shots” that will cause the trouble. In any case, a mass roll out of experimental “vaccines” on healthy people is madness. And certainly on healthy children.
I am already seeing damage in my elderly parents after just one jab – which got worse after 2 jabs – and I am dreading the impact of the “booster jabs” which I see no way of persuading them to refuse as they are convinced that covid is deadly [from watching BBC news] and they think that having the jabs is “the right thing to do” almost on some kind of moral grounds. I am reconciled now to losing my parents – long before their time – and watch them dying one day at a time. I imagine there are a lot of other people in the same boat but this is breaking my heart.
I absolutely sympathise with watching your parents get ill. My mother is one hundred next month. But are you sure that the damage is due to the jabs? Correlation is not causation and the sad truth is that elderly people do tend to get less well as time goes on (and they are particularly vulnerable to Covid).
Well, yeah – first it was the first shot that was gonna kill everyone, then the second shot… and when we see that people who have had the 2nd jab are still walking amongst us… now it’s the ‘booster’ that will be the one to get us.
Or the 2nd booster, or possibly the 3rd…. ad infinitum.
It seems the delay to all the deaths is similar to the delay in stopping the Covid restrictions/rules/laws.
Sometimes it’s hard to define the point at which something is reasonable or is just a whacky ‘conspiracy theory’.
My partner had the Pfizer jab 4 weeks ago, has noticed no side-effects at all, and is still alive and (apparently) well. That’s a fact. Despite me being suspicious of the ‘Covid scamdemic’ from the start, and not dismissing out-of-hand theories as ‘rubbish’, I also look at what is real. Of course, she may have all kinds of things wrong with her now, due to the vaccine, but I have no proof of that.
But I have seen the people-control, and the fear, and the abuse from ‘the believers’ hurled at the ‘unvaxxed’ and the mindless obeying of orders – that is certainly true.
I suppose it definitely was the Pfizer jab? Someone suggested that there could be doctors who knew it was harmful and were giving placebos instead. though whether there is any evidence for this I don’t know.
Brett Weinstein and guests: Vaccine is dangerous clip: https://youtu.be/Du2wm5nhTXY
Full video 3hrs: https://youtu.be/-_NNTVJzqtY
Reposting the scholarly review article. https://ijvtpr.com/index.php/IJVTPR/article/view/23/49
Steve Kirsch article “Should you get vaccinated?”
https://trialsitenews.com/should-you-get-vaccinated/
The Trial Site news article is brilliant – basically the fraud of the pandemic and the vaccine in a nutshell
It won’t happen immediately. There is good evidence the spike protein is a prion, meaning CJD, Alzheimers and other prion diseases are a risk. 95% of the humanised mice used in trials died after 2 weeks and in their brains were signs of spongiform encephalopathy. 2 weeks mice life equates to 18 months in humans I understand. Dr Fleming has talked about this here https://principia-scientific.com/globalists-patent-human-form-of-mad-cow-disease/
There are currently 48 new cases of CJD being investigated in Canada, coincidentally https://t.me/The_Censored
Also cancers will rise as the spike protein disables the cancer blocking mechanism in the body.
And don’t forget the risk of ADE and the 3rd wave affecting largely the vaccinated this winter.
So we will see a gradual but mounting death toll a lot of which will be attributed to other things, and there will be plausible deniability.
If there are 7 billion in the world, then reducing this to 1 billion would be an 86% reduction according to my sums
I think it’s nearer 8 billion now.
You need to read the whole thing, not just the headline. The whole study is rubbish yielding non-sensical results.
Will misunderstood the data – risk does not increase with second dose See my post above.
“Curiouser and curiouser“ cried Alice.
“That depends a good deal on where you want to get to” said the Cheshire Cat.
As always with these releases nothing makes sense.
The simple fact of the matter is that the S-Protein generated by the body in ALL Western “vaccines” is the original Wuhan variant.
I’m going to go with Dr. Yeadon on this and say that a 0.3% genetic variation SHOULD be a nothingburger, even for the “vaccines” at this stage.
The major problem at this stage is we have no idea on the following variables:
I’m fairly confident this is where the absolute numbers come in. From the hospitalization numbers I have seen recently (assuming they aren’t also lies like everything else) then it’s fairly safe to say that the hospitalizations between stabbed and organic humans are effectively a coin flip. Assuming a 0.3-1.1% absolute risk reduction if you were stupid enough to get stabbed voluntarily this probably makes sense.
This notion of the over 65s being “protected” by the vaccine: Sorry, I call absolute bullshit.
The majority of over 65 year olds I know, including my own mother who I have been red-pilling on all this BS – are absolutely terrified of this virus because of the brainwashing.
My mother would have been more than happy to roll her sleeve up until I told her she was massively contraindicated due to being on blood thinners for phlebitis and I’m almost 100% convinced we had Covid in December 2019.
So tl;dr on that point is, we know for a fact that over 65s are still “shielding” despite being “vaccinated”. We are also in the summer when respiratory viruses are at their weakest ebb.
Anything happening right now is bollocks and the proof of the pudding comes in three-four months time.
As a final point: as this article basically states, using a vaccine for prophylaxis is just about the most retarded thing I have ever heard of. You get vaccinated to be IMMUNIZED against a disease. If you want prophylaxis then use the Dr. Zelenko Covid-19 Prophylaxis Protocol:
Protocol for Low and Moderate Risk Patients:
* Elemental Zinc 25 mg once a day
* Vitamin C 1000 mg once a day
* Quercetin 500 mg (OTC) once a day
~ If Quercetin is unavailable, then use Epigallocatechin-gallate (EGCG) 400 mg (OTC) once a day [EGCG is found in Green Tea extract]
Taking the above every day is probably a great idea anyway – vitamins, minerals and anti-inflammatory/anti-oxidants.
I tend to agree with you across the whole lot. W.r.t. the last para in the article, they have never claimed that the so-called ‘vaccine’ would prevent infection or transmission; on the contrary, in the leaflets recommending it they pretty much say the opposite. It is only intended to reduce the symptoms, according to the published paperwork back in March. Admittedly, it’s a different story on the advertising posters etc. Economical with the truth, they are.
It’s called a Nonsterilising Innoculation and the way it is being used will create huge evolutionary pressure to make escape variants that actually will kill people. So buckle up and get your ivermectin now before Winter.
Comparing zinc. Zinc acetate.
https://www.biorxiv.org/content/10.1101/2021.06.15.448551v1
“It shows that, once testing positive with the Alpha variant, one dose of Pfizer reduces the risk of hospitalisation by 68% (the 0.32 highlighted), but the second dose only reduces the risk by 12%! That’s 12% in total (the 0.88 highlighted), not 12% on top of the 68%. So the second dose significantly increases your risk of being hospitalised compared to the first dose? That can’t be right.“
Why “can’t be right”?
This might be explained by the details of the study which I haven’t see, but just based on this summary it’s surely relatively easy to speculate that the full treatment has consequences that result in more hospitalisations, that almost (but not completely, it appears) wipe out any gains from the partial treatment?
It’s not clear to me from this summary whether it is talking about overall hospitalisation (which would therefore include side effects) or just hospitalisation with covid, but either way it seems perfectly conceivable that the second jab could reduce benefits gained by the first only. It could easily, for instance, render some people more vulnerable to serious consequences if they catch the disease even while giving some protection to most, surely?
Granted, the simplest explanation might well be poor study design, but I’m just not seeing the logic here.
This is a good point – it’s also worth questioning whether they controlled for the differing characteristics of the groups of jabbed once / twice / unjabbed as this is an observational rather than RCT study.
As the vaccine roll out has targeted higher risk groups first there will e.g. be many more old people who have been doubled jabbed. Thus the increase in relative risk may be due to more older people being double jabbed rather than due to the jabs themselves.
He’s using irony. He knows perfectly well the implications, but he is not saying them aloud.
The explanation is even simpler – Will misunderstood the meaning of the hazard ratio. See my post above.
So the second dose significantly increases your risk of being hospitalised compared to the first dose? That can’t be right. But it’s what it says.
Well this is a problem because the vaccines don’t do what you think they do. Will, I think you may need to catch up. Too many on LDS are playing the government at their own game, which is rigged, by claiming the vaccine has been working when we have correlation not causation.
Come winter flu season, those injected with these Nonsterilising inoculations are going to get very ill when they come into contact with the next strain.
The injections do not stop infection or create immunity, they merely reduce some symptoms at an absolute percentage of about 1%.
However they expose the recipient to risks of severe illness from subsequent exposure to the ‘wild’ virus ( and maybe other coronavirus, like the common cold). As the prevalence of SARS2 and its multitude of variants is very low in the summer , the effects will not start to be seen until later in the year.
This report starts hinting at these facts, but doesn’t explore what appear on the surface to be contradictory numbers.
I think Will has misinterpreted the hazard ratio. It does not reflect your probability of being hospitalised with one dose or two doses compared to no vaccine. That would be the VE. It reflects your probability of being hospitalised if you are symptomatic with our without vaccine. So the higher probabilities for the second dose mean that if you get symptoms despite having had two doses then your chances of going on to hospital are greater than if you get symptoms having had just one dose. This is interesting but not particularly surprising. For example, it may be that if you get symptoms despite having had two doses than you must have had a particularly large or virulent exposure which means you are that much more likely to go on to hospital than the one dose cohort.
Forget it.
As I’ve said, there is no chance now of abstracting any uncorrupted data. It’s all malfeasance, wishing and guess work.
Simply, by any normal safety criteria (as said), the snake oil should be taken out of the hands of the Mengele Memorial Brigade – and withdrawn.
Well duh!
To think a vaccine into your vein will protect you from an airbourne virus always seemed daft to me. Otherwise why not vaxx against common colds… Oh that’s right it’s well k own to do so would create more and newer strains. Likewise with kung flu.
Why should the method of transmission affect the efficacy of the vaccine? Flu, measles and mumps are all airbourne viruses with vaccines that have a long history of working. There is no vaccine against the common cold because it is caused by many different viruses.
I rather suspect that; elderly, frail & clinically vulnerable people make up the vast majority of the people who fail to generate antibodies after vaccination. Thus, the same kind of people who died from covid previously will be the same as the people who die in the future. The vaccine will make little difference to the vulnerable, & the people for whom antibodies are generated didn’t need a vaccine anyway.
I suspect the Government have realised this & so are now pursuing a zero covid policy to avoid people realising that everything to date was pointless as the same vulnerable people die at the same rate regardless of what they do.
I think it is a zero covid policy – but just as the means to achieve control as the measures required to get to zero covid are so restrictive they give them absolute control
“observational study”
Of course, this term is being seen all over the place.
Why? – because it is now the only available data regarding the effects of the snake oil, since proper testing was abandoned. There is absolutely no chance now of getting proper blinded RCT data – normally a requirement for anything of this significance. Vast stages of normal testing have been skipped – including sufficient preparatory animal studies.
Simply – one cannot judge the relative safety of this gene therapy withoutthat data.
‘Observational’ studies are important as follow-up, but they immediately run into all sorts of statistical complications re. manipulation and confounding variables etc. if the data is used as a substitute for honest trialing.
They cannot replace the need for proper controlled basic testing over a sufficient period of time. It’s as simple as that.
So what mechanism could be at work here? We know that generally the reactions to Pfizer are worse at the second jab. Is the exposure to the wild virus acting like a third jab, setting up some bigger inflammatory response which might be fatal in the old and frail?
Or an auto immune response?
The people who know are the vaccine research scientists, discussing all this behind closed doors.
Those who have not looked at the death of Simone Scott, 19, after her second dose of an rna, should urgently look at Alex Berenson’s Twitter. The most worrying aspect – after her death – is the parents’ report that the doctors would not report it to VAERS for evaluation. A doctor’s “assistant” eventually said it would be done. (Was it?) If even the horrible death of a 19 year old after the second jab is not automatically and immediately flagged from a sense of moral duty, then under reporting must be massive.
No need for an elaborate “mechanism”. All this is saying is that if you have had two jabs and nevertheless get symptoms then you are somewhat more likely to end up in hospital than if you have had one jab and nevertheless get symptoms. One plausible explanation is that an infection that gives you symptoms despite having had two jabs is particularly virulent. Another might be that the type of person who gets symptoms after two jabs is also the type of person who ends up in hospital.
A co-worker told me today that symptoms for the indi….sorry DELTA variant include hay fever symptoms. I haven’t read newspapers or watched the MSM propaganda for ages but please tell me this isn’t the case. F**ks sake!! they’ll have a field day, really high pollen count at the moment, they can claim that half the f**king country has this so called variant!!
In the UK the peak was early to mid April 2020 and it was unseasonably warm, prime conditions for hay fever symptoms to kick in. I did wonder if that might have had something to do with the whole debacle!
Not meaning to rain on the parade, but the conclusion in the header ignores the uncertainty in the estimates. The numbers vaccinated who develop symptomatic disease is large enough for the odds ratio to be well-estimated and incremental benefit shown. The numbers admitted to hospital are so small that there is a very imprecise estimate of hazard ratio, and it is the width of the intervals in the table, not the highlighted point-estimate that matters.
A better interpretation would be that there is insufficient data to distinguish the effects pf vaccination on hospitalisations by strain.
There is a more serious problem with the headline. See my post here.
https://dailysceptic.org/2021/06/16/phes-latest-vaccine-study-suggests-hospitalisation-risk-increases-after-the-second-dose/#comment-523517
Basically Will did not read the paper carefully enough.
Surely that is the age effect superposed on the vaccine uptake, all such relative metrics need to be age-banded for comparison.
Hi Will – I see you’ve posted the Spectator covid-19 hospital admissions by age which shows hospitalisation increases in ages 18-64 (lol). The issue is I’ve tried to find this data separately from the gov uk website and cannot find it anywhere – anyone know where The Spectator found this admissions by age data from on the gov.uk website? Am I being blind?