by Dr Clare Craig FRCPath
One thing that Public Health England has been world beating for before and during this pandemic has been the sharing of data. Data is collected from every aspect of the healthcare system and we now have the full dataset for 2020. The beginning of the graphs therefore give an indication of the levels expected at this time of year.
A selection of this data is presented that tells the story of a Spring pandemic. However, what this data reveals about Autumn and Winter does not fit the hypothesis that there has been a second wave. PCR testing results are an outlier in the data and only data related to PCR test results has led to the impression that there is currently a Covid problem.
Let’s take each dataset in turn.
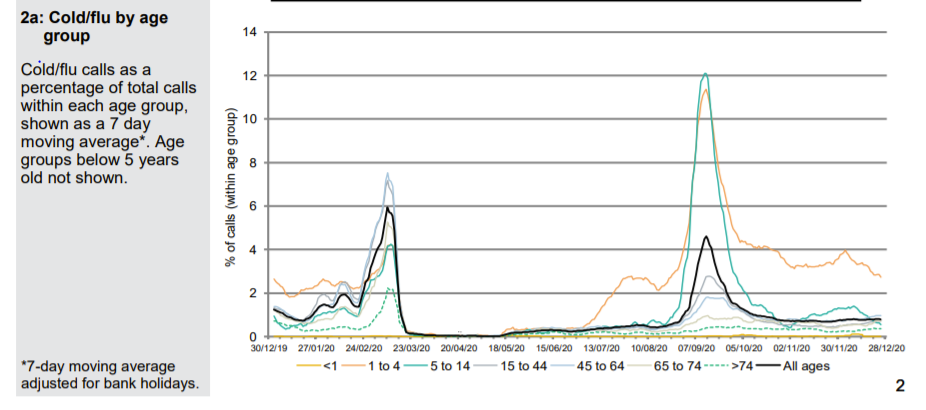
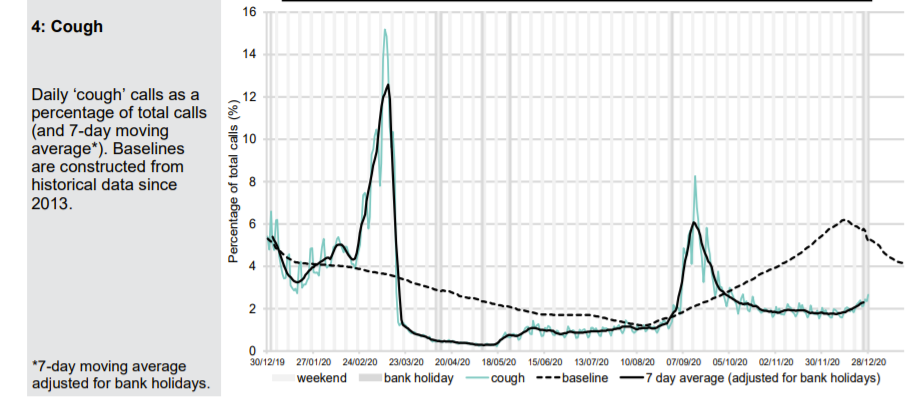
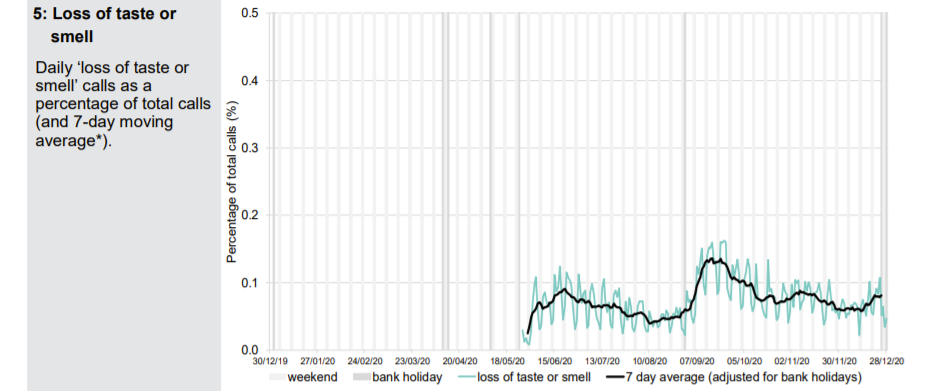
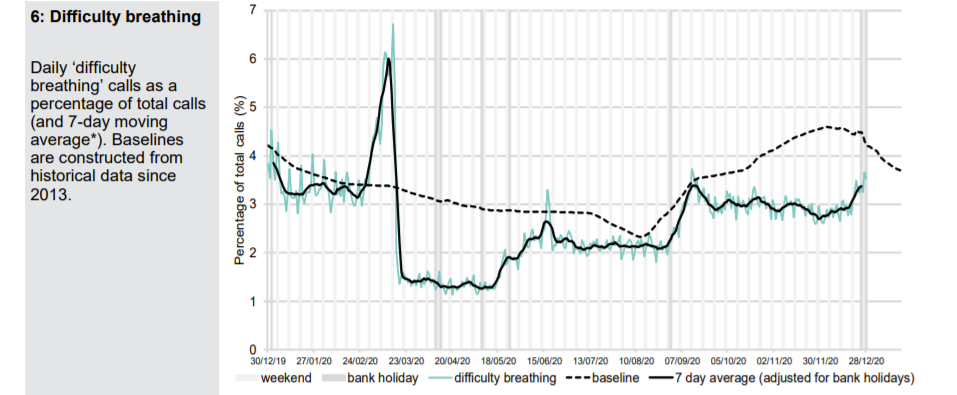
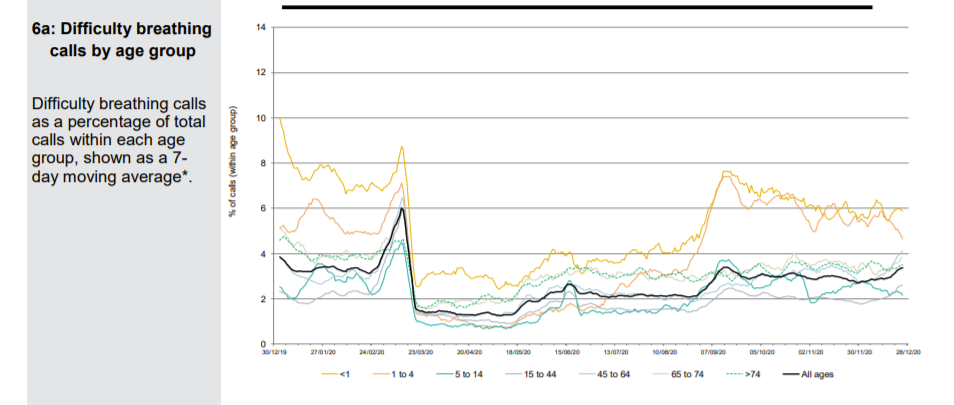
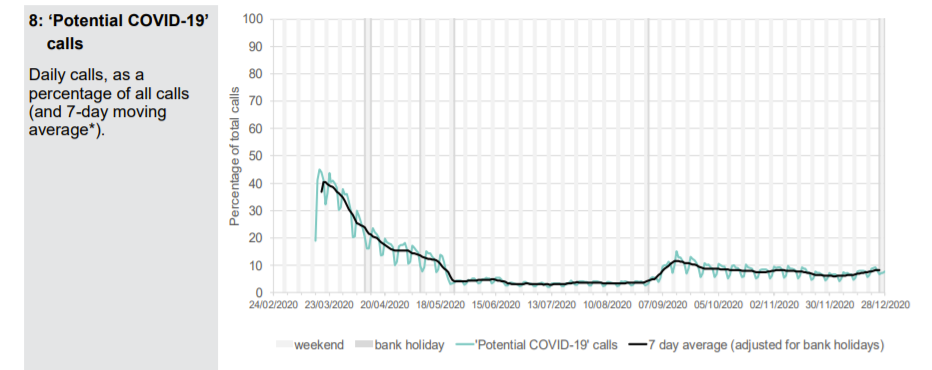
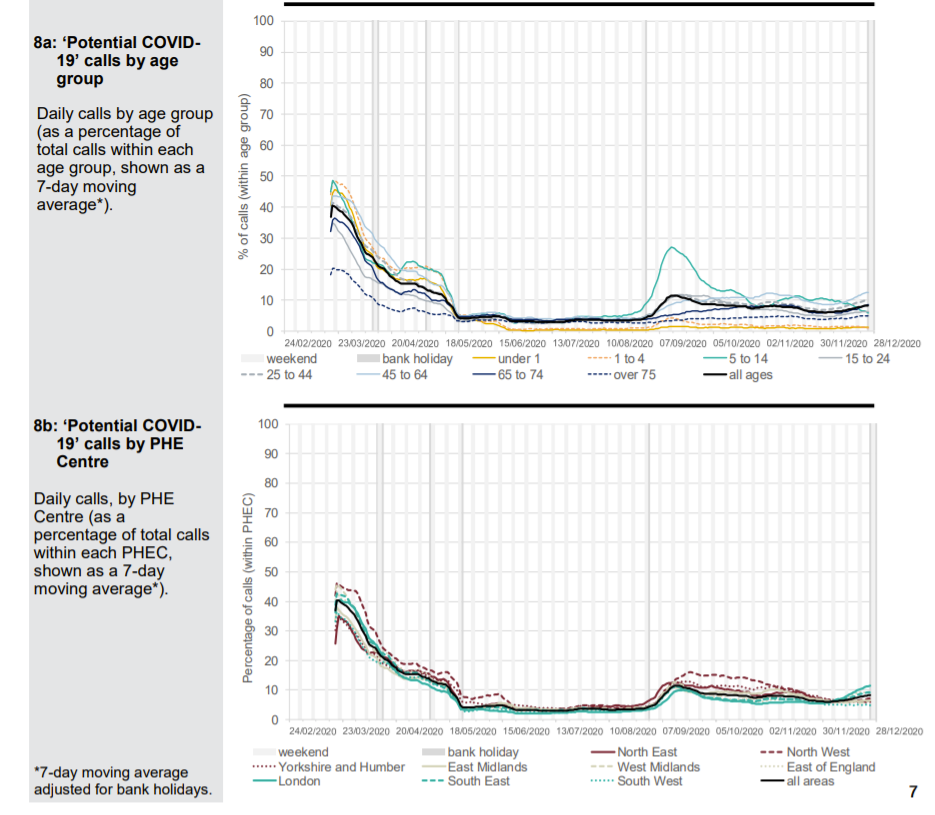
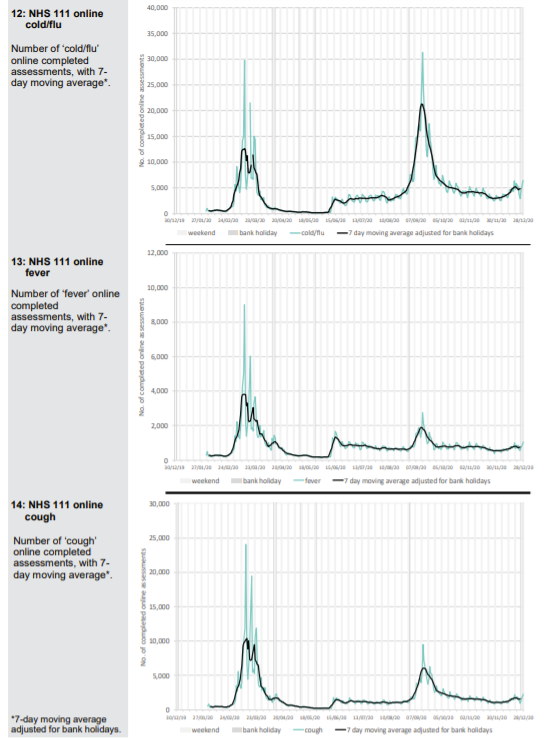
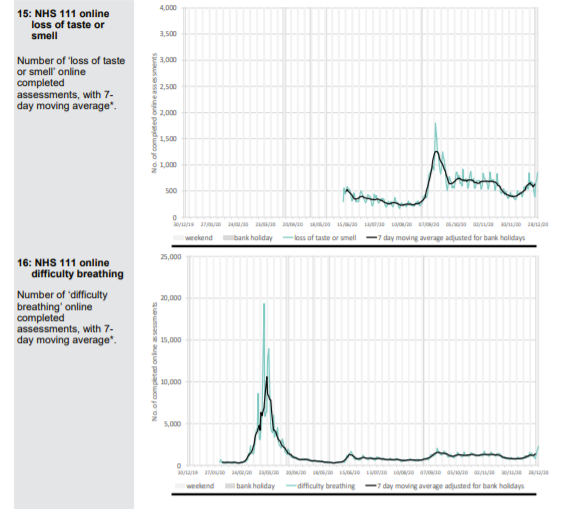
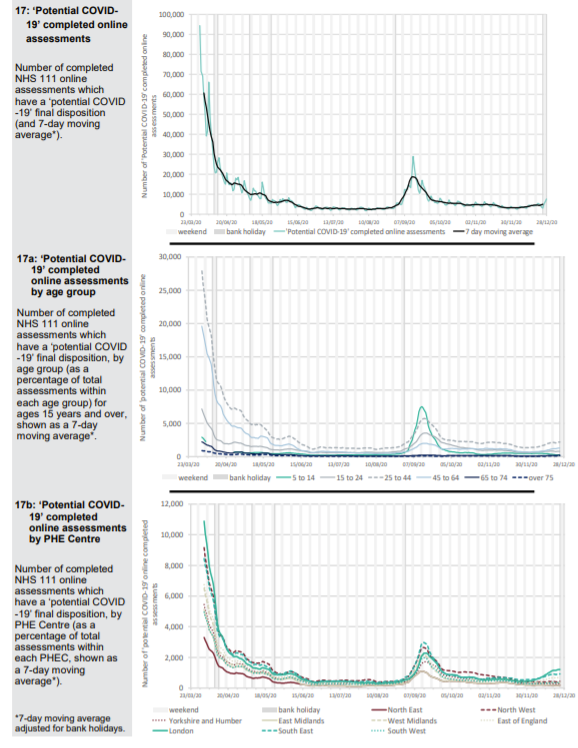
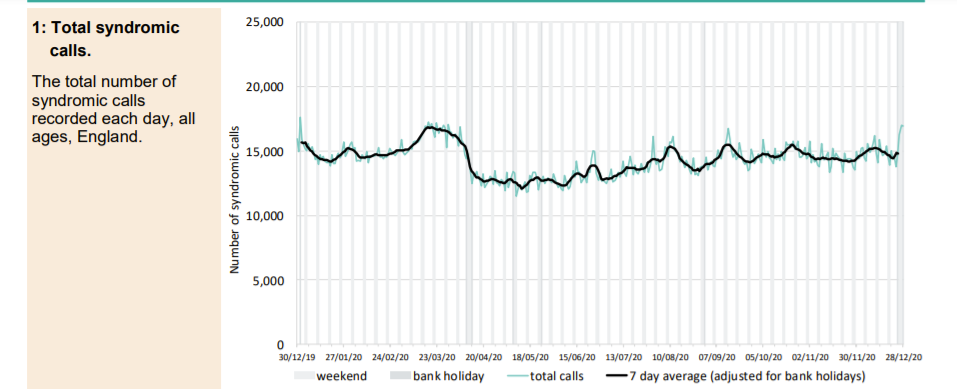
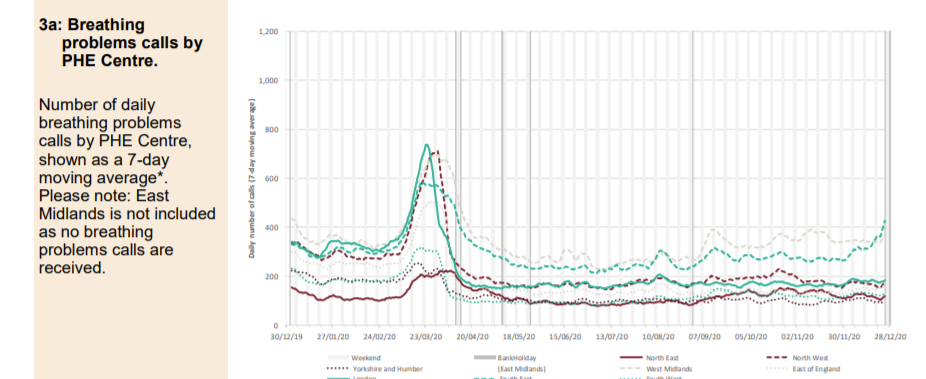
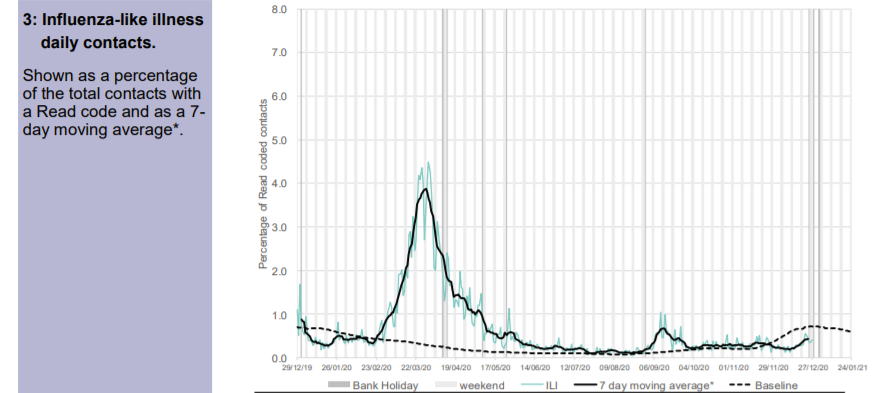
Patients phoning NHS 111 or visiting online are classified according to their symptoms. A Spring pandemic can easily be identified with a spike in presentations of patients with cold/flu symptoms; cough, fever and difficulty breathing. In September, when schools returned, there were epidemic levels of common cold symptoms and cough but not difficulty in breathing. A few of these were classified as Covid and there were regions of the country, which had been affected last and least in Spring, where excess deaths were seen. An Autumn second ripple, which was effectively the tail of the first wave is therefore identifiable.
A small uptick in Covid-like calls in London can be seen in December but otherwise there is nothing to suggest anything untoward in the NHS 111 data except that calls for cough and breathing difficulty are well below normal levels.
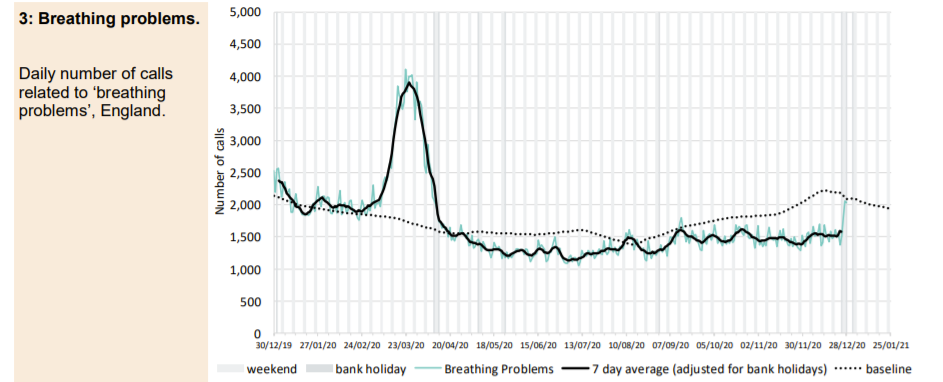
The Spring spike in ambulance calls was followed by a low but has returned to baseline with the usual post-Christmas variation around a mean. Ambulance call outs for breathing problems clearly show the Spring epidemic but the Autumn second ripple does not feature and current levels remain below baseline. A small increase in callouts in the South East more recently is apparent which may be significant.
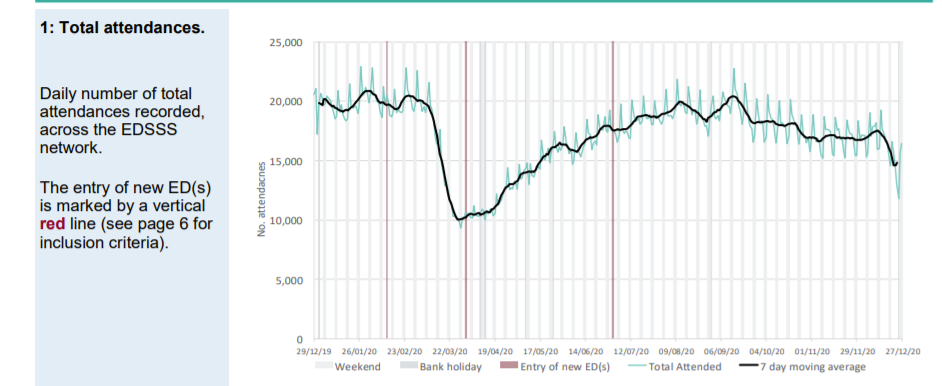
Accident and Emergency attendance plummeted from 28th February when people were told to self-isolate if they had a cough or fever. Current attendance is well below normal levels.
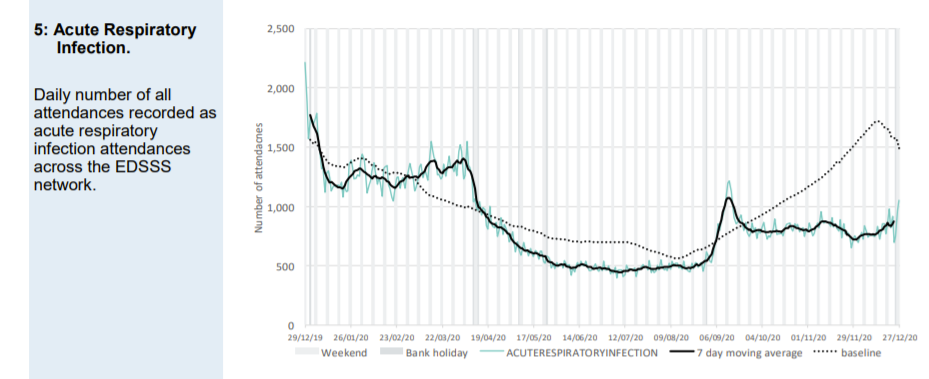
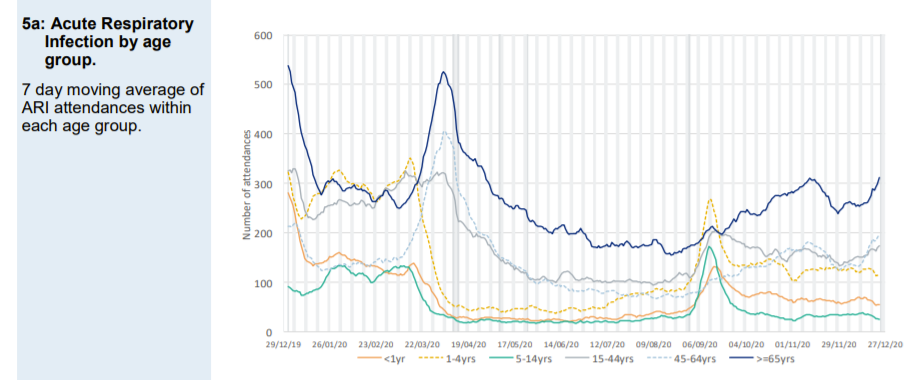
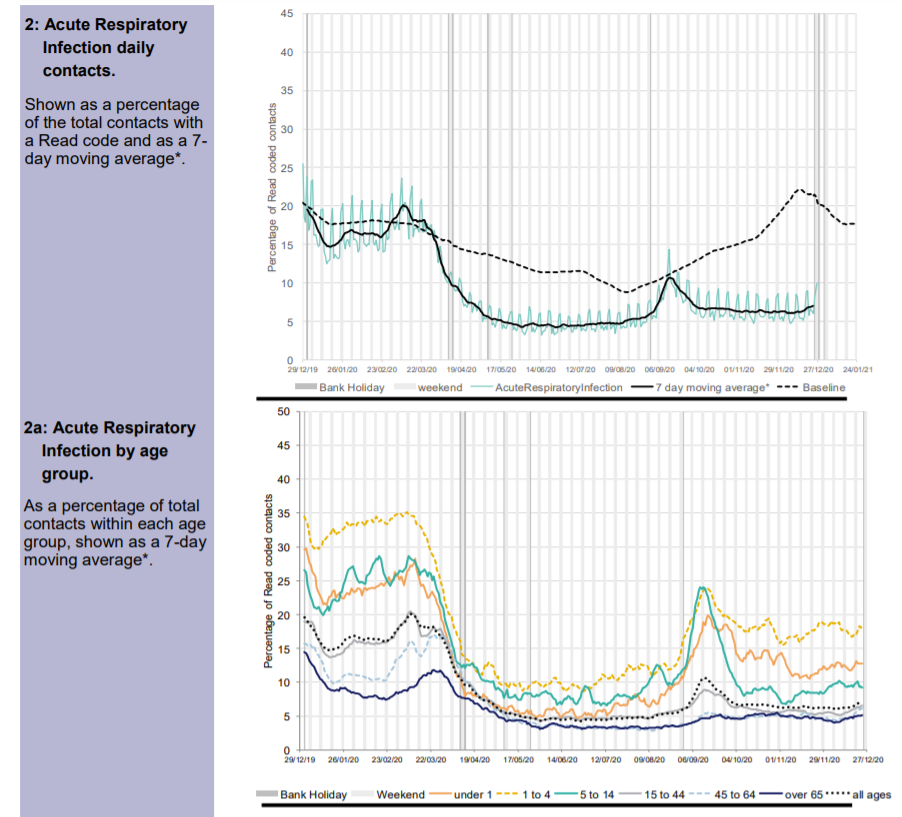
Attendances classified as acute respiratory infections (which include Covid-like) are well below normal levels. But the September spike can be seen. The September spike was seen in children and did not affect the elderly.
A new category of Covid-like attendance does not show the September spike seen in 111 data. This suggests that doctors reclassified these cases on arrival at A&E as other acute respiratory tract infections in the young.
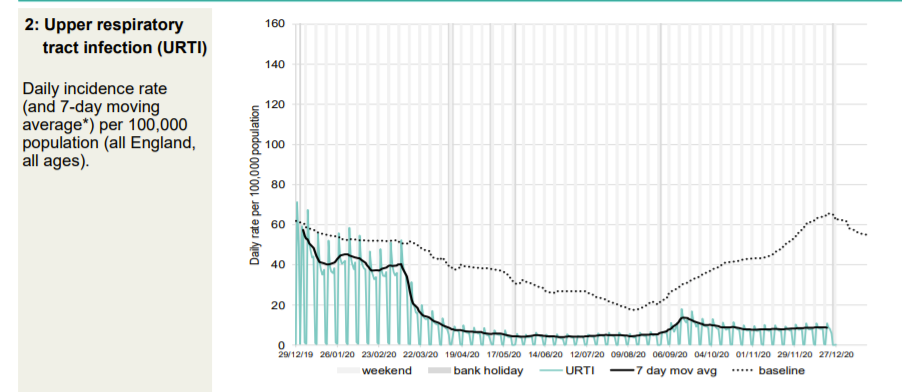
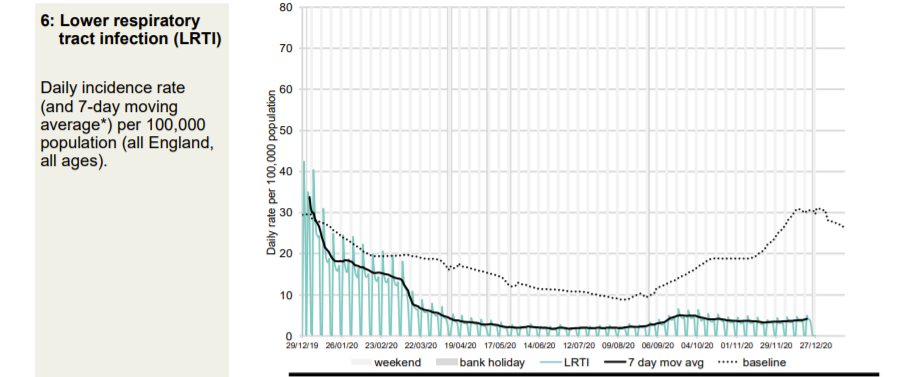
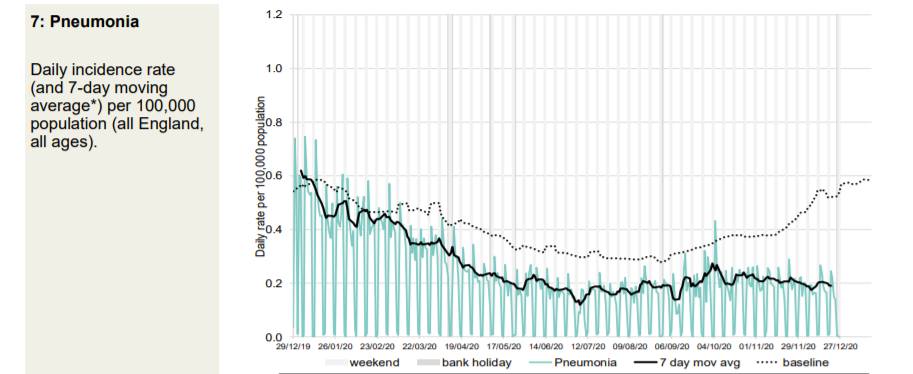
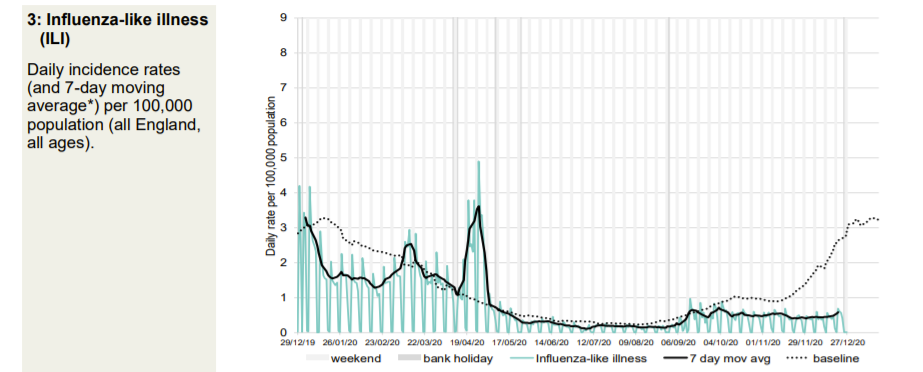
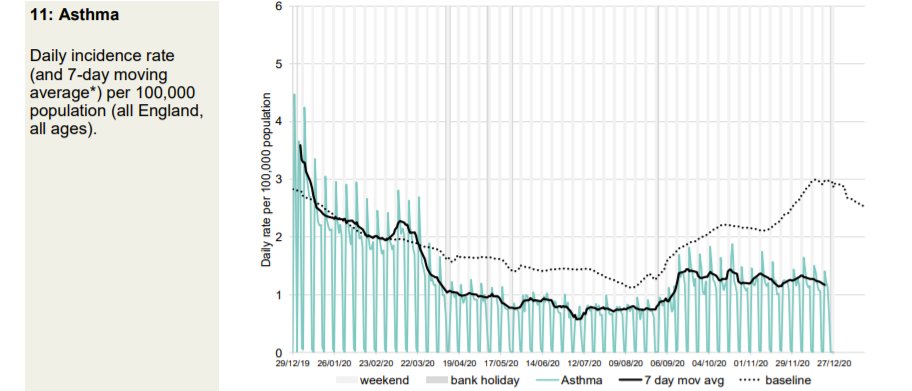
Every kind of respiratory presentation to a GP is significantly below normal for the time of year. However, patients are advised to get a Covid test if there is a suspicion of Covid. This will impact this data.
Thg GP out-of-hours data also shows that the September spike was due to non-Covid acute respiratory infections in the young. Patients calling GP out of hours with Covid symptoms “are advised to initially access a COVID-19 test” so the data will be distorted by this.
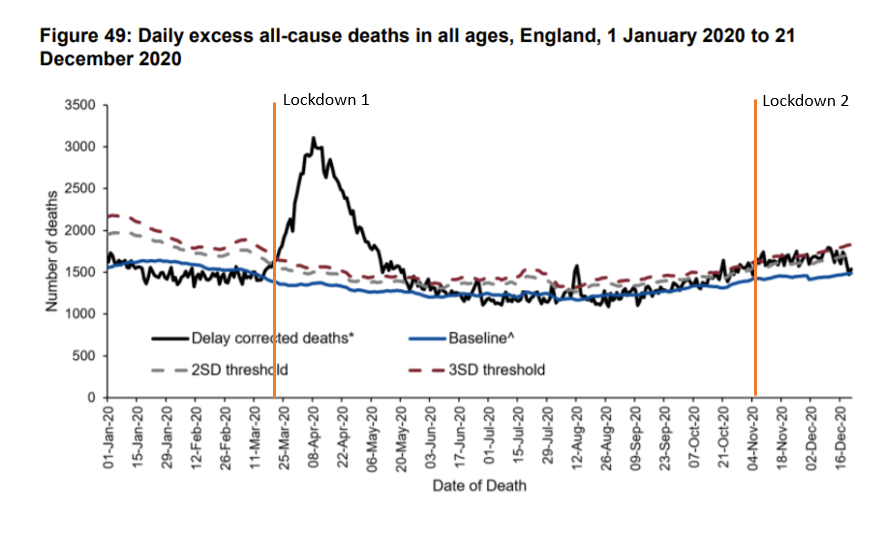
Although PCR testing has led to significant Covid-labelled deaths, these have not been reflected in excess deaths. The latest excess death data is back to baseline levels for the time of year. Those suggesting that this is due to intervention have forgotten how excess deaths climbed despite interventions in Spring.










Donate
We depend on your donations to keep this site going. Please give what you can.
Donate TodayComment on this Article
You’ll need to set up an account to comment if you don’t already have one. We ask for a minimum donation of £5 if you'd like to make a comment or post in our Forums.
Sign UpLatest News
Next PostCovid Cynicism