To recap what we have written so far. We have seen that good data do not support the idea that there is only one viral respiratory agent around, that its name is influenza (A or B) and that influenza causes mayhem around winter time every year.
In our Riddles series, we reported on the multiple logical gaps in germ theory. We often cite the failure to infect volunteers during challenge studies at the MRC Common Cold Unit when conditions are ideal for such an infection. A proportion of quarantined volunteers with no history or laboratory evidence of recent influenza illness were not infected by squirting viruses up their nostrils.
Other modes of transmission have not been studied with modern molecular diagnostics, so we are left with the evidence from the kissing and poker games studies to try and understand precisely how these bugs infect or activate (wake up).
There are several problems with understanding precisely what is going on. First, the clinical similarity between influenza-like illness (ILI, a syndrome caused by 200-odd known and X unknown microorganisms) and influenza (caused by influenza A and B) makes it easy to play on the F word “flu”. According to the media and politicians, everything is “flu”, but what do they mean by this term? You cannot identify a particular pathogen by its symptoms, as they are all the same.
In any year, relatively few cases of influenza-like illness are caused by influenza viruses and, as such, would be amenable to prevention by specific vaccines. The two – influenza and non-influenza ILI – are not clinically distinguishable, and even periods of known higher influenza virus circulation are not predictive, as other organisms (such as rhinoviruses, RSV and parainfluenza viruses) are co-circulating.
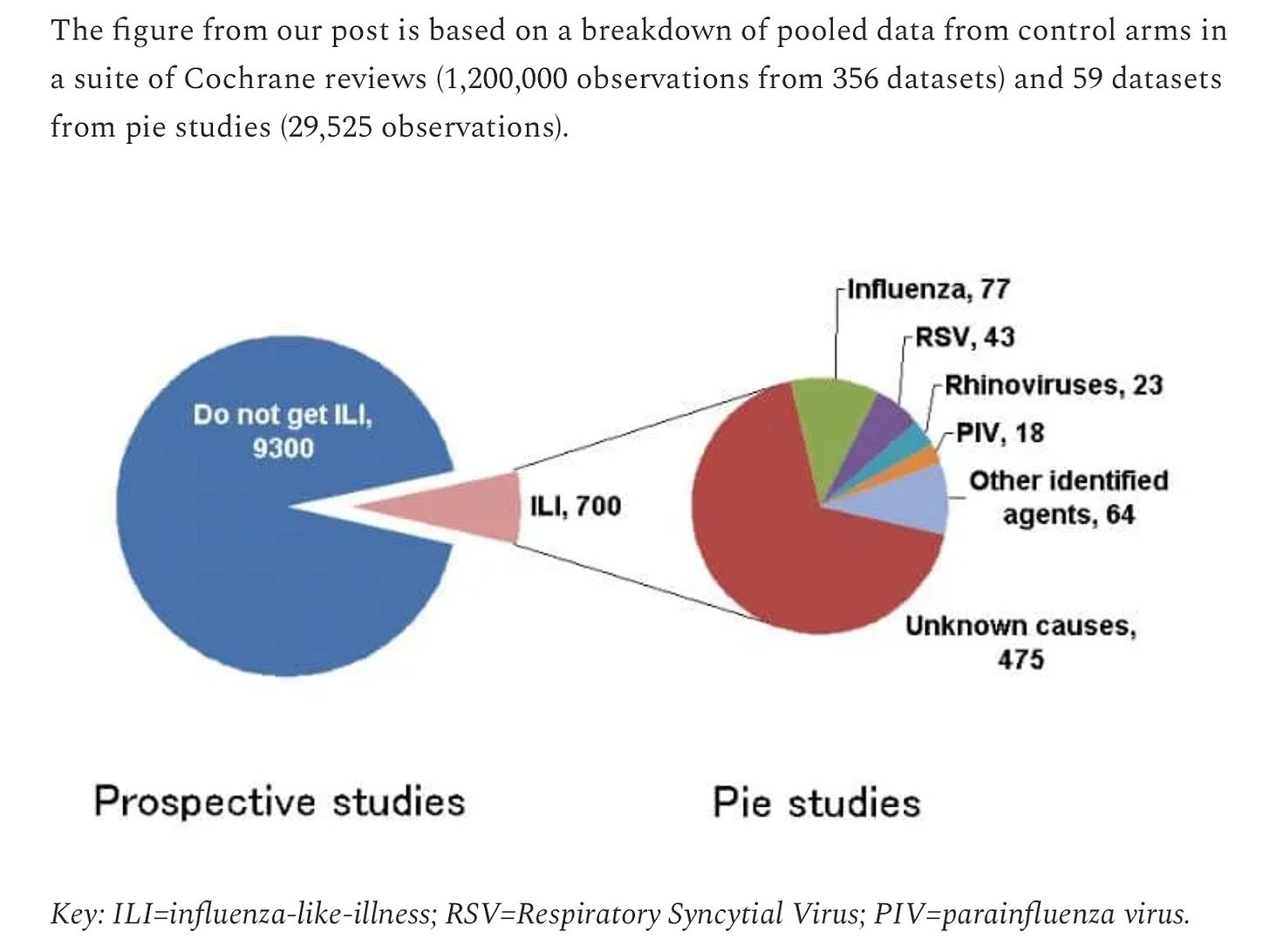
To understand the microbiology of all this, consider ILI cases (the F word) as a yearly pie, which shows just 11% (77 of 700) of ILI cases actually being caused by the influenza virus.
We explained this in one of our earliest posts.
Data from the control arms of studies in our Cochrane review and proportional epidemiology studies (PIE) are likely to yield reliable data because they are designed to follow those up with symptoms and test them. You can also check the comings and goings of these agents in our Week in Numbers series, which shows that most of those tested with symptoms are not due to influenza.
The second problem is that no one knows the precise burden of influenza morbidity or mortality, as no surveillance system is capable of routinely distinguishing influenza and influenza-like illness, and no one carries out routine autopsies to identify a microbiological cause of death. So, guesswork rules. This explains, in part, the wildly inflated CDC estimates, which not even Dr. Fauci believed.
These simple biology facts are seldom mentioned by physicians and the media, who are instead told that current measures (e.g. vaccination) are sufficient to control the problem, although no one quite knows the size of the problem, and few understand its multiagent nature.
Add the fact that influenza viruses mutate continuously, and by vaccinating, you are essentially chasing a moving target: you begin to understand why auntie, who had been vaccinated against the F word, still gets the F word.
For politicians, the value of this ignorance and confusion is great. By referring to “flu” and their yearly prevention programme with “flu vaccines”, they are seen to have acted and fixed the problem, especially if they can bolster their nonsense with a dollop of extra cash for health services. The cash, as you well know, does not come from their pockets.
It remains to be seen whether the public will smell a rat as they are suddenly pressed into influenza, Covid and RSV vaccines: “Wait, was there not just a single agent five years ago? Where have the other two come from? Are there others? What? There are? Does it mean everyone will be vaccinated against 60 more bugs in a few years?”
A critical evaluation of vaccine effects is complex as systematic reviews show the studies are often of poor quality. There is a lack of randomised controlled trials of sufficient duration and too small a sample size to detect an effect on serious outcomes (such as hospitalisation and death). That is the observation which fits the evidence: a small sample size means they are comparatively rare events.
As a consequence of the poor evidence base there is an over-reliance on non-randomised studies and models, which, as you know, can be made to tell you just about anything you want. For example, some widely referenced non-randomised studies in people aged 65 years or older systematically report an implausible sequence of effects, with trivalent influenza vaccines apparently effective for the prevention of non-specific outcomes, such as death from all causes, but not for the prevention of influenza or death caused by pneumonia and influenza.
The bulk of evidence (hundreds of thousands of observations) comes from poor quality, large, retrospective, data-linked cohorts in which data had been collected for other purposes (usually reimbursement). Twenty-two out of 40 retrospective cohort studies published up to 2006 failed to report either vaccine content, degree of antigen matching, or both, making generalising from these datasets an arduous task.
So how do we know about these problems? Because, unlike the media, politicians, lobbyists and influencers, we read and assessed these studies before deciding that they were simply not worth the effort. We kept them on in our updated Cochrane reviews as legacy appendices.
To finish off we now come to another set of questions.
- In a similar situation, how are decision makers justifying pushing the yearly mammoth undertaking of influenza vaccination?
- Why have influenza vaccines played such a prominent role in the last two decades?
- Does this dubious and costly enterprise apply to Covid vaccines?
In the next installments, we will see the justification CDC and friends gave for their actions and provide evidence that everything is not going well – we are being fleeced.
This post was written by an old geezer who’s been working on this for three decades and hopes that the content of posts like these will be his legacy. The other old geezer just shakes his head.
Dr. Carl Heneghan is the Oxford Professor of Evidence Based Medicine and Dr. Tom Jefferson is an epidemiologist based in Rome who works with Professor Heneghan on the Cochrane Collaboration. This article was first published on their Substack, Trust The Evidence, which you can subscribe to here.














To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
The fallacy that the planet and its climate exists for our sake, and that its current state is ‘optimal’ and deserving of our efforts to maintain it as such, demonstrates the height of human arrogance.
Do you mean the height of human ignorance
Both, I’d say.
.I find it odd that a bunch of committed environmentalists, who want to save trees, should aim at dropping CO2 to the ‘pre-industrial level’ of 280ppm.
Which will put a major strain on all plant life…
How major a strain?
Quote some facts on this.
Oh, about this much he said, holding his hands apart.
Never wondered why people pump co2 into their greenhouses/aquariums?
anyway, here you go:
There’s at least one tree on here suffering from a lack of CO2.
Don’t tell climate Genius Al Gore – it might be an ‘inconvenient truth’.
Apart from the ones that can no longer grow, due to drought etc.
And evidence please? Obviously you’ve got your deserts, semi-deserts, artic regions.
We all await an evidenced response.
Wrong as usual.
As CO2 levels rise trees require less water due to the stomata have to stay open for shorter periods so less water is lost.
I’m sure he’d be happy to, just following you posting your first fact ever on this site.
This site seems to be an inappropriate place for facts.
This site? I think you mean your brain.
With regard to climate science, it seems you wouldn’t recognise a fact if it bit you on your snout.
Plants consume CO2 when photosynthesising to generate energy to grow.
CO2 is plant food.
before life on earth the atmosphere was overwhelmingly composed of CO2, algae, plants and anything else that can photosynthesise changed the atmospheric composition over billions of years to the tiny amounts of co2 we have now.
you can google “early earth atmospheric composition” and find out for yourself.
I learnt about photosynthesis in infant school.
id consider knowledge of how plants make their energy to be elementary science, in the same league as adding water to something makes it wet.
not knowing that co2 is plant food is probably why the young are all get up about this.
”Fake invisible catastrophes and threats of doom” by Dr Patrick Moore.
There – have a read. That should inform you.
Twelve Teslas Queued Up For A Charge
https://rumble.com/vy6wei-twelve-teslas-queued-up-for-a-charge.html?
tonyheller
Saturday 26th March 1pm to 3pm
Yellow Boards LONDON
Junction Victoria St/Bressenden Pl
London SW1E 5NA
Stand in the Park Sundays from 10am – make friends & keep sane
Wokingham Howard Palmer Gardens
(Cockpit Path car park free on Sunday)
Sturges Rd RG40 2HD
Telegram http://t.me/astandintheparkbracknell
It’s pretty obvious from the charts, that 250,000 years ago and every 100 thousand odd years before that, humans existed with a vast industrial polluting civilisation that caused their manmade climate warming and caused catastrophic events that wiped any traces of their existence off the face of the planet.
Any parent knows that ‘because I say its so’ is the mark of a lost argument.
Also if I might be so bold, can I mention that there is no money in telling the truth on this or many other subjects.
Off subject
Under the terms of the Online Safety Bill you are not allowed to tell anyone about the below article
‘Incredible’ teenager died from blood clot after receiving AstraZeneca Covid jab – North Wales Live (dailypost.co.uk)
I would like to know why her life doesn’t matter; why charges have not been brought.
I’m not even sure I believe there’s such a thing as ‘the climate’
There isn’t. It was a convenient term to describe regional weather variations to schoolchildren.
What alarmists mean when they refer to climate is temperature change, they are just too stupid to realise that.
They are ‘just too stupid’ – period. And they are not alone in this sad crowded little Island.
No CO2 connection – no need for net zero. Keep chipping away, Mr Morrison.
No point in chipping away… he’s only talking to a handful of deniers.
They are already on his side and there is no cogent argument put forward to deny the reality of climate change. Good enough for you lot, but not for sensible folks.
Which reality is that? the one represented by the first assessment by the IPCC, or the second, or the third …….. We are now on the sixth now and they still haven’t got it right. Good to know the science is settled.
Hello tree. CO2 is your food. More CO2, deserts shrink, record crops, fewer starve. Try https://notrickszone.com/2022/03/19/higher-co2-concentrations-mean-better-plant-water-use-enhanced-photosynthesis-expanding-sahel/
plenty more where that came from.
You’ve ended up on the wrong website again. Try http://www.bbc.co.uk – you’ll find all sorts of interesting news and lifestyle articles that will satisfy your need for establishment viewpoints. Wonderful recipes too, happy browsing!
Still waiting for one of you to make a cogent argument. Looks like it will be a long wait.
It’s http://www.bbc.co.uk; there’s a menu bar at the top where you can access all the main stories and the recipes are under Food. There’s Have Your Say too if you’re interested, you can share ideas with like-minded members of the public who I think will really enjoy your commentary.
Your hypothesis, it’s on you to provide evidence. That’s called science, by the way.
No one’s denying the reality of climate change we’re just questioning the claim that a) the anthropogenic signature has been detected b) that increased CO2 is the cause of global warming c) that a warming of the planet will end life as we know it. So Mr. Tree, what evidence have you got that you can share?
I don’t know a single person who denies the climate, or even that it’s changing.
Running round with your hair on fire screaming ‘we’re all doomed’ isn’t science.
Bring something meaningful to the conversation.
Is there anyone quite so blind and obtuse as this person “Tree” who will not acknowledge that there have been periods of much more intense warming and cooling long before man-made emissions? Carbon dioxide may play some small part today but current warming is nothing like we have had in the past. I have looked down from the hills above Harlech in North Wales and seen the remnants of terraces where vines grew freely during the Roman warm period. And, trudging through a rank and miserable bog above Machynlleth, I was amazed to be told by an archaeologist in our hiking party that we were standing in part of a pre-Roman kingdom, where digs had shown it was once a land flowing in milk and honey whose people created dazzling artefacts. “Tree”? He or she is barking up the wrong one. More to be pitied for blind ignorance than laughed at.for sheer folly.
Was anyone around to witness any of these very warm periods of time?
Were they trying to grow crops to feed billions of people.
Using excessive timeframe trends to argue against real trends now seems to be standard denier tactics. Doesn’t stop it being stupid.
You have confirmed to me that no one should take you seriously. You ask did anyone witness these warm periods of time. The vine terraces speak for themselves to anyone with half an ounce of common sense. It was t hot enough for people to grow grapes, for goodness sake. And of course I explained that archaeological digs have attested to the bogs above Machynlleth once having been rich agricultural land capable of supporting a vibrant culture. With people like your good self around it is no wonder we have had two years of dreadful collateral damage from the Covid lockdowns. The warming psychosis echoes the similar Covid fear, panic and blindness.
http://www.bbc.co.uk
I’m sure someone must have around in those days, though I’ve never met one. Should I then conclude that they didn’t exist?
Meanwhile, focussing obsessively on ridiculously short timeframe trends with no historical context seems to be standard alarmist tactics. Doesn’t stop it being stupid, though.
Take a look at the wholly unrealistic and clearly stupid temperature projection used by Al Gore.
Using miniscule timeframes is standard climate panicker tactics. Doesn’t stop it being stupid
You’ll find all sorts of sensible folks in the Have Your Say section on the BBC website. With your way with words, you’ll get tonnes of

 Good luck!
Good luck!
Use of the word ‘denier’ betrays your ignorance of both science and reality.
Climate Change ….
Another attempt to deny the undeniable.
DS keeps doing coming up with this selective garbage and the readers just buy it.
They are duty bound to oppose anything that is an accepted truth.
So just publish a dodgy article and let their ignorance and preconceptions to the rest.
If you tilt the graph it can agree with your version of reality. It’s all the rage with the modelling community these days.
Your epistemological and psychoanalytical sense making is too advanced for us, tree . What are we buying?
. What are we buying?
Try coming up with something yourself to convince us all the planet is warming catastrophically.
You see.. making things up isn’t for me.
You are pushing a large gas-bag of CO2 uphill!
Where are your objective facts and how do you differentiate them from your hysteria??
Look there are 30 such idiots with their downward thumbs.
The BBC has an excellent Climate Crisis section I think you’d really enjoy. Up to date reporting of the myriad impacts extreme weather is having around the world. Sobering stuff ..
Do you think you are funny?
You clearly think you’re clever, but I’ve seen no empirical evidence of that either.
Deny the undeniable.
Accepted truth.
I think the ignorance and preconconceptions are clearly yours.
Look up up logical fallacies, first formalised by Aristotle 2500 years ago.
Though I haven’t met him either, so he probably didn’t exist.
“don’t worry the next ice age in 50000 years should cool us down”
You know what they say, make hay while the sun shines.
Gates wants to block out the sun – the giver of life. – with dust
That fugures.
Gates: a truly evil being.
And this is why it’s vital that Nigel Farage and other leading figures opposing the carbon madness stop giving credence to the man-made CO2 threat.
AGW is the great deception employed by the Reset Gang to crush working and middle class oiks.
Agreed. Farage and Tice hit the easy target of Net Zero, but back away from disputing the “settled” science around CO2. Politics, eh.
Defeat NetZero and ‘climate change’ is defeated.
Get Johnson out of Number Ten and this increasingly rotten Tory Party is defeated!
Surprised that you would prefer Labour.
There is no such thing as ‘settled science’ or else the sun would still be going around the earth as a matter of “scientific fact”
F=MA
P=V^2/R
What’s wrong with these.
Got it in one!
I’m getting a strong feeling of deja vu with these climate articles. Even when preaching to the choir you might want to mix up the parables a bit.
Have you listened to the BBC or read the Guardian lately?
What politicians say: it’s vital that we massively reduce emissions.
What politicians do: spend 25 years rapidly increasing the population through mass immigration of people from countries where per capita emissions are much, often very, very much, lower. With Channel -crossers, people from Hong Kong, Ukrainians and “Ukrainians”, the current government seems determined to achieve new records.
British passport holders from Hong Kong, of which there are many, by definition, are British and entitled to come here.
BBC, 1 February 2021
“British National Overseas (BNO) citizenship is a type of British nationality created in 1985 that people in Hong Kong could apply for before the 1997 handover to China to retain a link with the UK.
The lifelong status, which cannot be passed down to family members, did not give holders any special rights.
It meant only they could visit the UK for six months without a visa.
But the new system, in place from 31 January 2021, allows these BNO citizens and their close family to apply for two periods of five years to live and work in the UK.
After the first five years, they are able to choose to apply for indefinite leave to remain, which means an individual can live and work without applying for a visa.
And after one year of this status, individuals are able to apply for British citizenship.”
That’s just your racism talking.
That’s just your drooling imbecility talking.
Bad News, everyone.
I remember watching this lawyer testify to Reiner Fuellmich’s Coronavirus Committee.
She has been arrested
One of the attorneys assisting Reiner Fuelmich in proving world leaders have committed crimes against humanity in the name of Covid-19, has been arrested in France on suspicion of terrorism and treason.
Virginie de Araujo Recchia, a French attorney living in France who is participating in the work of the Citizen Jury with Reiner Fuellmich, was arrested in her home at dawn on March 22nd in front of her children. The arrest comes three weeks before ahead of the French presidential elections.
Fuellmich’s team have allegedly been informed the charges involve counterterrorism and possibly treason
https://dailyexpose.uk/2022/03/24/fuelmich-lawyer-arrested-treason-for-exposing-covid-fraud/
https://www.conspiracywatch.info/virginie-de-araujo-recchia
https://archive.ph/Ed8es
An interesting article, thank you. It’s such a shame our cloth-eared, brain-dead political leaders ignore facts and science and make policy on the advice of soothsayers.
A sigh of Relief At last British joins lists are being red pilled and finding the courage ( the balls ) to write the truth about this climate fraud , the likes of pierce Corbyn, Vernon Coleman & Tony Heller has been saying this for donkeys ( forgive the spelling ) .
Yet another dismissal of the climate change scam. However, one of the main benefits to the globalists and their minions, such as Boris, is to impoverish normal people whilst building their own wealth and exercising a truly Orwellian level of control over us. We are at war with them and we simply have to win, whatever it takes, for the benefit of our descendants. Of course “climate change” is only one of their weapons…
Those four glacials/interglacials. Turning points top and bottom roughly align. Some sort of natural governor at work. Overlay CO2, and it peaked at, what, 280ppm? Not much doom-loop runaway catastrophic global warming climate change. And now CO2 is over 400ppm, shouldn’t temperature be off the scale?
It’s logical that there is a natural relationship between the two, in as much as when it’s really frozen, the number of plants that extract CO2 is bound to be lower. Apart from the temperature and lack of available water, low carbon levels in the air would also inhibit the growth of plants. A bit like turning down the heat and slowing the clock, as it were.
Chris, excellent acerbic piece, with a great counter-riposte at the end.
There are plots of (estimated) temperature going back 500m years, also showing CO2, proving that rises and CO2 are never tethered, the latter mechanistically driving the former – as we are currently forced to believe.
I was very depressed to watch Steve Baker on a video saying that the chance to counter the narrative that “carbon” is responsible for rising temperature, and that a minute rise in one inevitably meant a rise in the other, was lost. That train has left the station he said.
Thank for your generous comment. It’s the same with Farage and Tice. They want a Net Zero referendum but seem to accept that we need to reduce CO2 emissions. You can’t have both, since Net Zero is a logical solution if you think the planet faces an existential threat from CO2. It’s just politicians playing their usual games.