Already by the last week of October 2022, continuing through November and early December, local Rhode Island media were amplifying clinician and public health official warnings about a paediatric respiratory illness ‘tripledemic’. The ‘tripledemic’ that prompted this tocsin of looming calamity in children was an alleged convergence of COVID-19, influenza and respiratory syncytial virus (RSV).
Serious paediatric illness is best gauged by the actual number of children hospitalised, as opposed to ‘respiratory virus test positivity’. The latter is especially misleading because of the unique, ongoing phenomenon of continued mass COVID-19 testing for minimal symptoms. Curiously, almost two months later, I could find no local media follow-up coverage elucidating the feared paediatric ‘tripledemic’ by this most germane metric: a direct comparison of children hospitalised for COVID-19, influenza or RSV.
With the cooperation of Rhode Island Department of Health (RIDOH) spokesman Joseph Wendelken, and an academic paediatrician at Hasbro Children’s Hospital, I can now present those hospitalisation data, per the table below. Given time lags in compilation and transmission, the hospitalisation record only covers all of October, and November 2022.
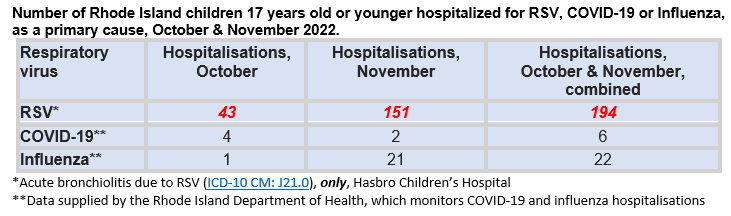
Despite the anguished media declarations, there was no Rhode Island paediatric ‘tripledemic’, at least through October and November. RSV, alone, accounted for around 90% (194 ÷ 222 = 87.4%) of so-called ‘tripledemic’ hospitalisations among Rhode Island children, and the rate of RSV hospitalisations (97 per month), was around seven-fold the rate of COVID-19 and influenza hospitalisations combined (14 per month). Moreover, the surrogate for RSV hospitalisations, a single International Classification of Diseases (ICD) RSV code (bronchiolitis, an inflammation of the smaller lung airways) omits RSV pneumonia and bronchitis coded hospitalisations. Certainly, omitting these ICD codes underestimates true paediatric RSV admissions.
The rate of primary (or ‘suspected‘ primary) COVID-19 pediatric hospitalisations mirrored what I discovered about the receding ‘Omicron wave’ from February to early June 2022. After weeks of wrangling, requiring an Access to Public Records Act submission to the Rhode Island Department of Health (RIDOH), supported by two state legislators, my query on paediatric COVID-19 hospitalisations in the first half of 2022 was answered on August 5th 2022. These data revealed that during the 16-week period from February 13th 2022 through June 4th 2022 there were a total of only 15 primary COVID-19 paediatric hospitalisations (for ages 0 to 17 years-old), as determined by RIDOH criteria. Notwithstanding this clinically insignificant, low ebb trickle of COVID-19 paediatric hospitalisations, RIDOH issued two memos recommending Rhode Island public schools re-institute compulsory masking (see RIDOH memos dated May 19th 2022 and May 20th 2022) for all school children in so-called “high COVID-19 transmission” districts.
Present ‘tripledemic’ nonoccurrence aside, the overwhelmingly RSV-driven rate of increased paediatric respiratory illness hospitalisations in Rhode Island during October and November should decline significantly in December and January as RSV infection rates peaked in early November and declined precipitously through early December (see data from RIDOH, plotted below).
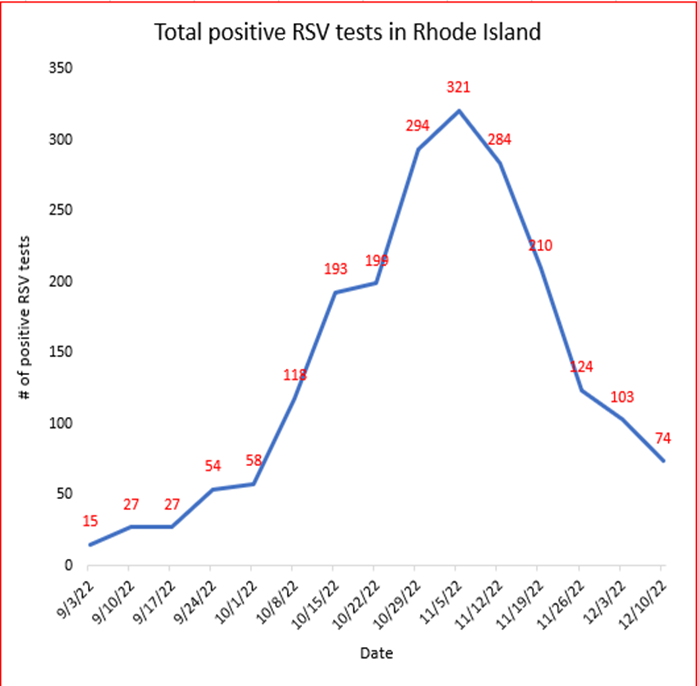
Additional reassuring national data from the Centers for Disease Control and Prevention (CDC) indicate the early influenza spike this year may be peaking in the U.S. overall as well, albeit not yet in New England. The third leg of the non-‘tripledemic’, COVID-19 paediatric infections, are not spiking in Rhode Island above rates observed since the summer and early autumn, while primary COVID-19 hospitalisation rates in children (see earlier table) remain exceedingly low.
Predictably, those Rhode Island medical thought leaders ginning up unwarranted concerns about the ‘tripledemic’ are once again, ad nauseum, pushing non-evidence-based masking and vaccination in children.
They ignore uniformly negative randomised controlled trials (RCTs) on community masking for the prevention of either influenza (12 RCTs; 10 here; also here and here) or COVID-19 (two RCTs; here, here), complemented by a small RCT in healthcare workers which demonstrated masks also failed to prevent RSV. While acknowledging the absence of a viable vaccine for RSV (but failing to mention the catastrophic failure of historical RSV ‘immunisation’), such thought leaders also ignore the absence of RCT data demonstrating either influenza or COVID-19 vaccines prevent hospitalisation from these respiratory illnesses in children.
The high rate of paediatric RSV hospitalisations alone in October-November should not be shrilly exploited by the media or so-called medical authorities to make counterfactual claims of an RSV, COVID-19 and influenza ‘tripledemic’. Instead, RSV, and now influenza, far more than COVID-19, should be accepted for what they are, i.e., part of the natural cycle of paediatric respiratory infections, and treated calmly, and with caring.
Dr. Andrew Bostom is a physician currently affiliated with the Brown University Center for Primary Care and Prevention, and was an Associate Professor of Medicine and Family Medicine at the Warren Alpert Medical School of Brown University from 1997 until June 2021. As a clinical trialist and epidemiologist he designed and completed the largest randomised controlled trial conducted in chronic kidney transplant recipients.











To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.