There follows a guest post by our in-house doctor, a former senior NHS medic, who says the latest ‘perfect storm’ causing pressure on the health service in parts of the country is more a self-induced squall.
In the middle of last week, several NHS Trusts issued warnings about the acute strain their services were under. The South Central Ambulance Service went so far as to declare a critical incident – normally reserved for a situation in which demands on the service exceed the capacity to manage those demands. I was surprised that so many NHS bodies spread over a wide geographical area issued public warnings about their failure to cope at the same time. Statements referred to high demand on services (hardly news) and lacked any specific detail about critical capacity constraints. Accordingly, the Daily Sceptic asked me to interrogate the available data to work out the extent to which a Covid resurgence might be responsible for the latest ‘perfect storm’ to hit the NHS.
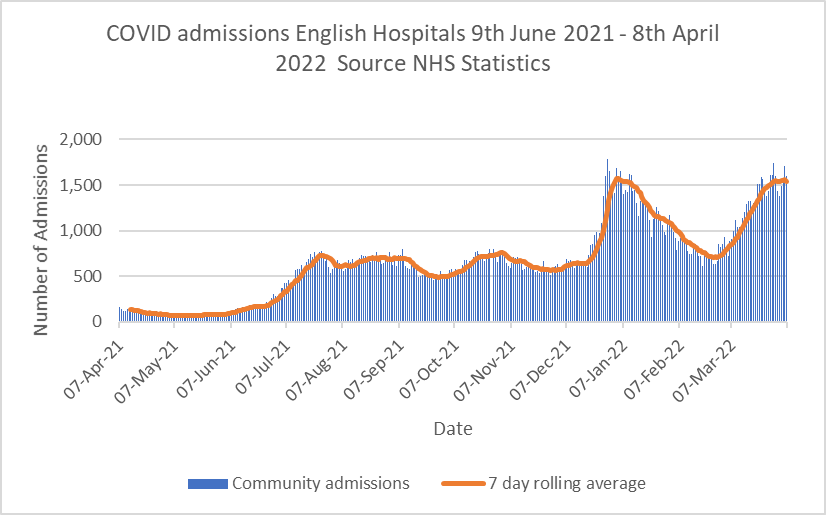
Graph 1 shows daily admissions of Covid positive patients from the community. Admissions have risen in the last few weeks, but seem to be tailing off. Data from Graph 1 have been the subject of hysterical articles in the mainstream press implying the latest Omicron BA.2 subvariant may be triggering a new wave of acute Covid infections. It’s not sensible to interpret Graph 1 as a stand-alone figure without considering contextual information from other datasets.
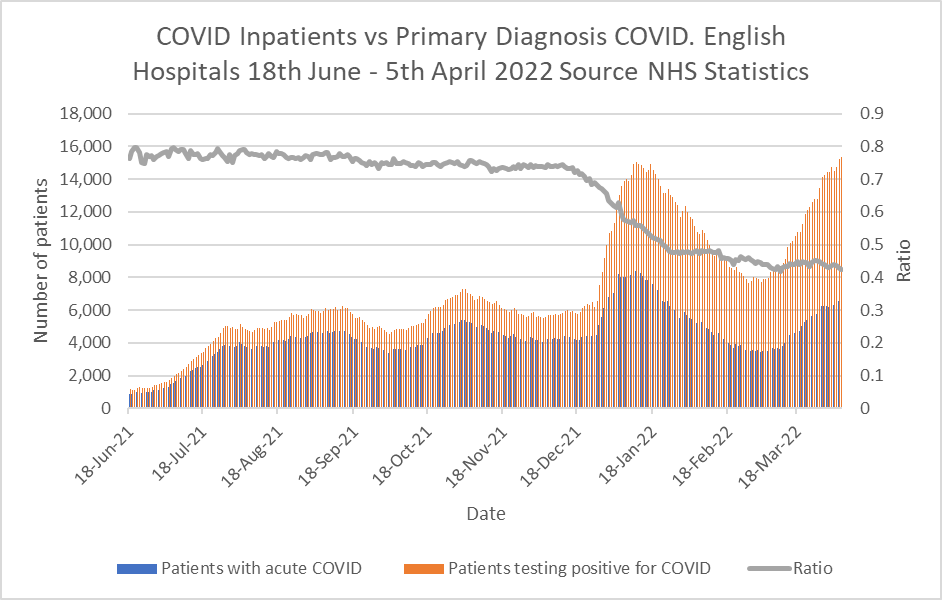
Graph 2 for example shows information from the Primary Diagnosis dataset. Regular readers will recall this set shows the numbers of patients admitted suffering from acute Covid compared to the patients testing positive for Covid but admitted for another condition. The grey line shows the ratio is gradually falling – in other words the headline figures in Graph 1 are misleading, because nearly 60% of those patients are not actually ill with Covid but admitted for other reasons.
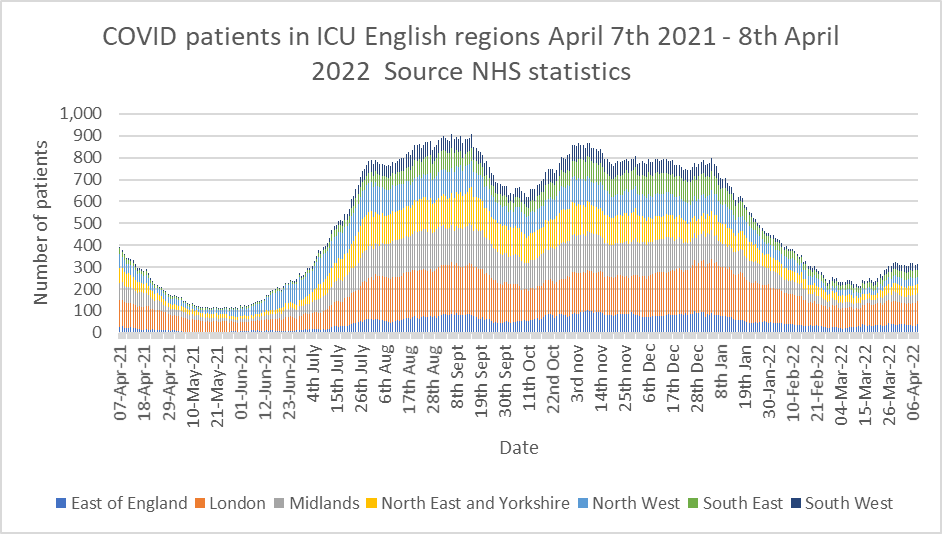
Graph 3 shows the numbers of patients testing positive for Covid in intensive care departments. The rise in cases seen in Graph 1 since the beginning of March 2022 is absent – so although there are more hospital inpatients testing positive for Covid than at the end of February, they are not ending up in critical care. Further, the data from the most recent ICNARC report reveal that the latest tranche of Covid ICU patients have lower oxygen requirements and better respiratory ratios than the cohort from this time last year – in other words, they are not as acutely ill.
Graph 4 is very instructive. It shows the average length of stays of Covid patients up to the end of December 2021. This data was released in March and unfortunately is only complete up to the end of 2021, but it is reasonable to infer that current length of stay is unlikely to be worse now than in December of 2021, due to increased availability of new monoclonal antibody drugs which reduce disease severity for the highest risk patients. Graph 4 expresses average length of stay as the mean average (blue bars) and the median average (orange bars). Both these averages are steadily reducing with the median length of stay being down to four days by the end of December 2021. For the information of statistically curious readers, the median average in this case is probably more representative of the situation as the mean average can easily be skewed to the upside by a small number of very long-stay patients.
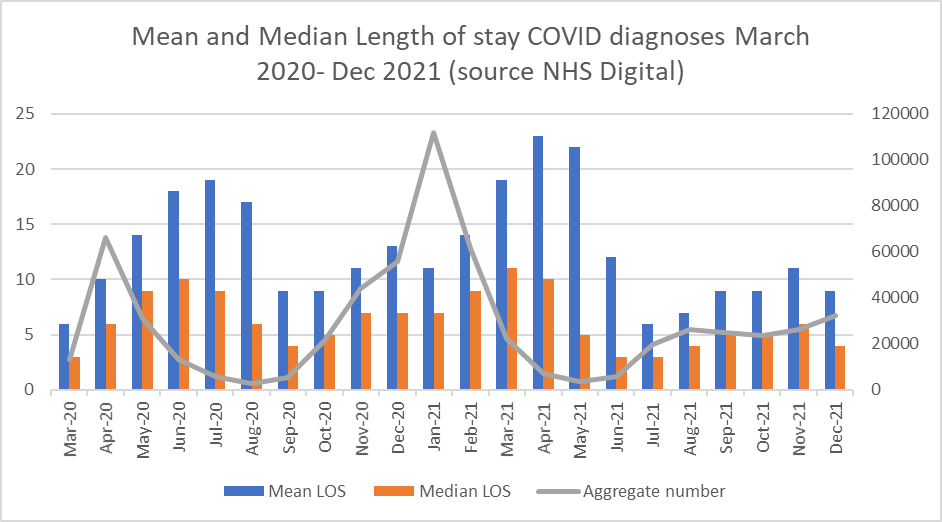
Overall, from the available Covid-specific patient data, we see a rise in total positive Covid tests on admission from the community, but fewer than half of these patients are symptomatic for Covid. Very few patients are ill enough to need ICU care and the length of stay for acutely ill Covid patients continues to fall. The vast majority require a few days of supplementary oxygen, intravenous steroids and monoclonal antibody infusion (or other adjunctive therapies) before being fit to discharge. So where is the problem?
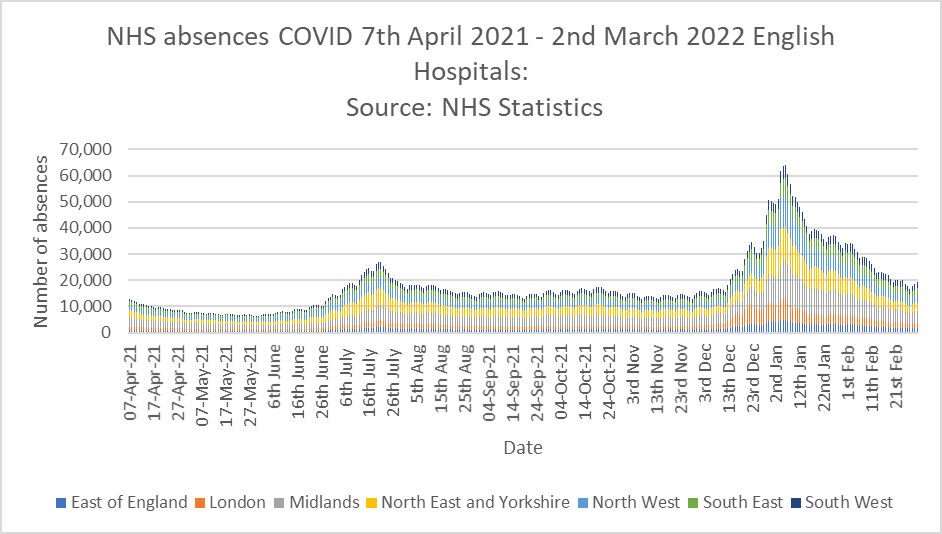
Last week Saffron Cordery, deputy CEO of NHS providers, commented that staff absences played a part in the current crisis. Graph 5 shows the data for Covid related staff absences up to March 2nd (the latest figures released) – they don’t seem to have changed much lately and were on a downward trend since the turn of the year. It’s possible they may have started to increase again, but the figures are not yet released for public scrutiny.
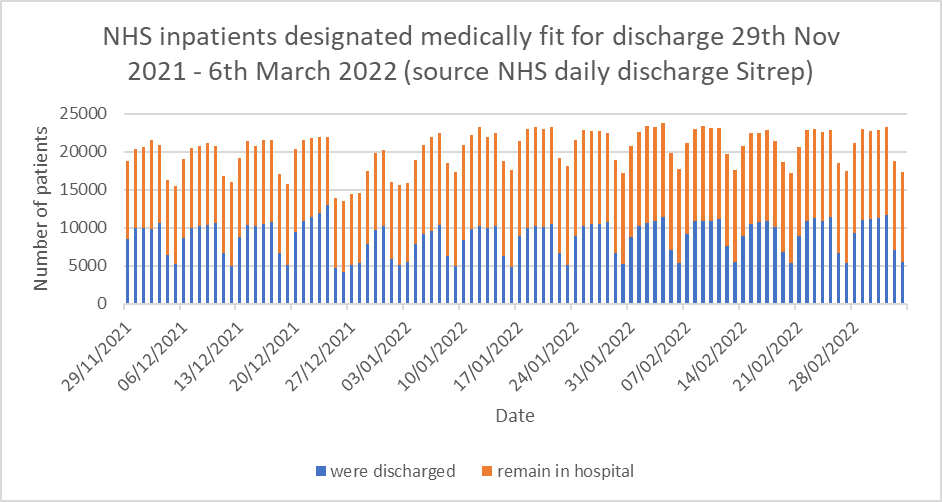
My personal suspicion is that Graph 6 shows the main issue causing trouble in hospitals. Graph 6 shows the number of patients in hospitals deemed medically fit for discharge. It is shown as a stacked bar chart, so the blue bar represents the patients who actually were discharged and the orange bar shows patients who were fit for discharge but had to remain in hospital for administrative reasons (often referred to as ‘bed blocking’). Readers will readily notice the ‘weekend effect’ in the figures, and that about 11,000 patients per day are in hospital when they are fit to be discharged – about 10% of the total NHS bed stock.
Over two years into the pandemic, the NHS does not yet seem to have solved fundamental administrative problems in relation to patient flow through the system. I am also aware from personal communication with colleagues that most NHS trusts are still imposing unnecessary Covid protocols which add to the time taken to complete basic episodes of care such as routine operations. This reduces efficiency still further in a healthcare system not renowned for operational efficiency in the first place.
Speaking about the latest crisis, Mark Ainsworth, Director of Operations at the South Central Ambulance Service, said declaring a critical incident meant it could focus its resources on the neediest patients.
Discharging medically fit patients from hospital and exercising a modicum of common sense when compiling Standard Operating procedures might achieve the same effect.












To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
And what about the Police taking the knee for BLM
The UK police officers are considered servants of the Crown and holders of the Office of Constable, not employees. This means they are not employed by the police force, but rather appointed by the Crown. The uniform, while standardized, can vary slightly by force and is subject to local policies. Crown-related symbolism, like the Tudor Crown, is also incorporated into police crests and insignia. The Police wear the Crown and they submitted the Crown to a Marxist mob that rioted and also desecrated the Cenotaph.
What about Starmer and Rayner taking the knee for a known criminal, our politicians are detestable.
Yes. That was treason.
An individual belonging to a protected category victim-group complaining about police impartiality surrounding a different protected category victim-group. The system will uphold the complaint. It has successfully dismantled the old normal and now works towards dismantling the new normal. The introduction of a new society requires complete destruction of the old society, which requires division – the more division the quicker the new society will be installed.
METROPOLITAN POLICE FOR THE NEXT CASE PLEASE
This is undoubtedly excellent news, not just for Linzi personally, but for all of the decent LGB community who wish to rightly distance themselves from the toxic, degenerate mental illness ideology that the TQ+ lot represent, for women standing up for their sex-based rights and for free speech in general. Only the biggest cynics wouldn’t see this for the win that it is. Now this needs to be implemented across ALL police forces in the country because none of them should be participating or showing support for this dangerous and perverse child mutilation cult which provably harbours sex pests and paedos;
”High Court Rules Northumbria Police BANNED from Pride Festivals!
Huge congratulations to We Are Fair Cop and @RightNUFC for their tireless efforts in pushing for this change!
In a landmark decision, the High Court has ruled that Northumbria Police can no longer participate in Pride festivals, citing concerns over the politicisation of law enforcement.
This is a MAJOR win for police neutrality!
For too long, police involvement in Pride events has sparked debate. While some see it as a gesture of inclusivity, others argue Pride’s political undertones compromise police impartiality. The court agrees: law enforcement must stay neutral, avoiding alignment with any social or political cause.
This ruling prohibits Northumbria Police from marching in Pride parades, displaying Pride symbols on uniforms/vehicles, or officially endorsing these events. It’s a clear message: police should focus on public safety, not activism.
Their campaign highlights the importance of keeping our police force impartial and accountable.
What’s next? This could set a precedent for other UK police forces, prompting a rethink of how they engage with community events. The decision may spark broader discussions about the role of Pride and the balance between celebration and politics.”
https://x.com/GerryKeogh_/status/1945498589368873359
I’m surprised so many gay and lesbian people still seem to associate with pride now it’s almost exclusively focused on transgender rights which are often anti gay/lesbian. One example is the fact that quite a few gay/lesbian young people go through a phase of thinking they might be trans as they realise and come to accept that they’re same sex attracted. The trans activists rush to confirm these youngsters temporary trans beliefs and push them onto a path to puberty blockers, surgical mutilation, loss of pleasure in sex etc. rather than letting then grow out of their trans beliefs and become happy same sex attracted adults.
All reasonable gays/lesbians should abandon pride and join the LGB Alliance.
Do you know what the best thing would be? And it’d be a test to see who’s really bothered about attending this crapfest because they’re bound to whinge the loudest, and I can take a confident stab at who that’d be…
Do a Viktor Orban and ban the entire thing. I’d gladly see the back of it.
But I think we can safely say that’ll never happen in this part of Europe, and we all know why. This lot ( much like the Muslims ) wield too much power now and must be appeased and pandered to, no matter what. This toxic ideology has got it’s feet firmly under the table and isn’t going anywhere. I doubt even Farage would have the balls to do a Trump or Orban and risk upsetting the transmafia.
Just a bit of supporting evidence to my above post;
“Keir Starmer has hosted a ‘Pride Reception’ in Downing Street.
Speakers included men in dresses identifying as women.
He committed to hosting a ‘LGBTQIA+ Roundtable’.
One attendee said that Starmer has “real understanding of the challenges queer people face”.
Worrying.”
https://x.com/JamesEsses/status/1945391679957012826
I’m sure the Muslim Party will sort it out when they hold the reins of power.
A great win. And now let us have who made the decision to take part either fired or demoted to a PC.
It was the chief constable who ordered her force to take part. She writes articles about how proud she is to be a lez. Thank goodness there are sensible homosexusls to rein in the exhibitionists.