The latest Public Health England (PHE) Technical Briefing on the variants of concern is out, and it shows that the infectiousness of the Delta (Indian) variant has dropped again, so that it is now at the same level as the Alpha (British) variant was at the end of March.
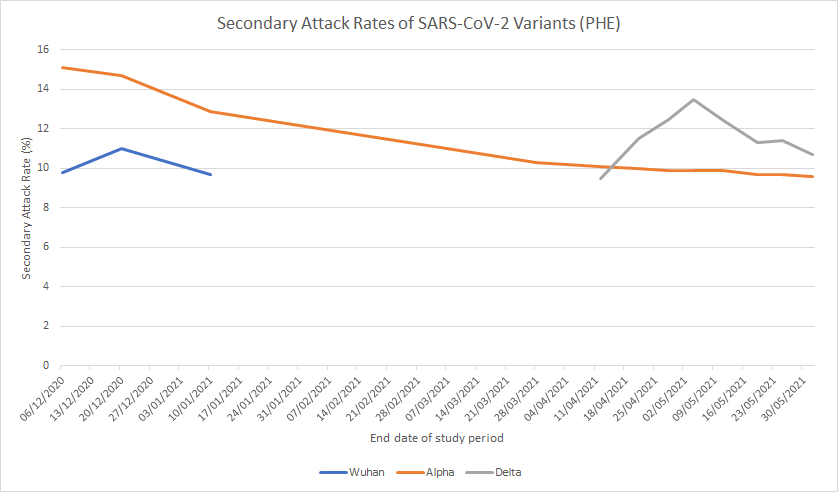
The Delta variant secondary attack rate (SAR – the proportion of contacts an infected person infects) is down to 10.7% this week, from 11.4% a week ago (see graph above). That means that around 90% of the close contacts of people infected with the Delta variant are not infected by them. Once again, this shows how claims that the Delta variant is “60% more transmissible” or similar fail to make clear that transmissibility changes and often declines over time, and that even if the Delta variant is currently more infectious than the Alpha variant it is still less infectious than the Alpha variant was when it first appeared on the scene.
You might be wondering, though, how a disease that only infects 10-15% of close contacts, even at the height of an epidemic wave, can be called highly infectious. And indeed, how such a disease can cause an explosive epidemic wave at all, and why those waves crash down as quickly as they arise despite not exhausting the pool of susceptible people.
If you do wonder that, you would not be alone. A famed epidemiologist called Robert Edgar Hope-Simpson spent his life observing the idiosyncrasies of seasonal influenza and summarised some of his thinking in a 1981 article entitled “The role of season in the epidemiology of influenza“. More recently, in 2008, a group of scientists took up Hope-Simpson’s investigations (which were inconclusive) and summarised seven conundrums of influenza that he identified, all of which apply equally to COVID-19:
1. Why is influenza both seasonal and ubiquitous and where is the virus between epidemics?
2. Why are the epidemics so explosive?
3. Why do epidemics end so abruptly?
4. What explains the frequent coincidental timing of epidemics in countries of similar latitudes?
5. Why is the serial interval [the time it takes for secondary cases to appear] obscure?
6. Why is the secondary attack rate so low?
7. Why did epidemics in previous ages spread so rapidly, despite the lack of modern transport?
The scientists add two more:
8. Why does experimental inoculation [infection] of seronegative [without antibodies] humans fail to cause illness in all the volunteers?
9. Why has influenza mortality of the aged not declined as their vaccination rates increased?
To explain these strange features, Hope-Simpson proposed the radical notion that, unlike other infectious diseases like measles and non-seasonal cold-causing viruses like rhinovirus, influenza is not primarily spread by transmission from the sick to the well (hence the low SAR). Rather it is spread by temporarily highly infectious and usually symptomless carriers in whom the virus has been latent but has now been triggered by a seasonal stimulus. Hope-Simpson was never able to identify the seasonal stimulus, though argued it must be ultimately dependent on variation in solar radiation, which is the driver of the seasons.
The scientists behind the 2008 article are not persuaded by the idea of latency of influenza, which they suggest has no evidence. Instead, they think the behaviour can be explained by seasonal variations in innate immunity, especially caused by the drop in vitamin D during winter months:
Significant seasonal and population variations in innate immunity make it unnecessary to postulate latency to explain the bizarre epidemiology of influenza… To make sense of influenza’s epidemiology, we revise Hope-Simpson theory, hypothesising marked variation in the infectivity of the infected (the good infectors demonstrated in rats by Schulman and Kilbourne in 1963) and that vitamin D deficiency is Hope-Simpson’s seasonal stimulus.
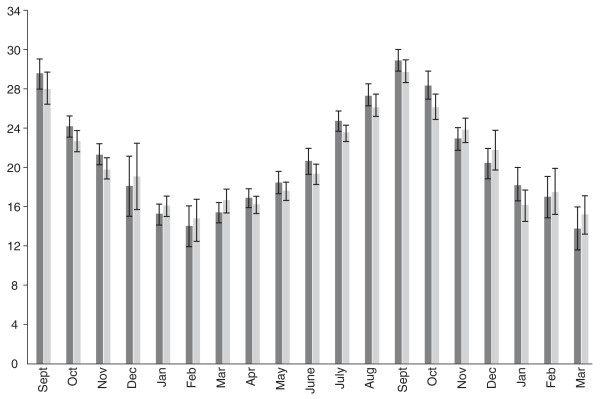
This theory leaves questions of its own, however, such as why a gently undulating vitamin D level would suddenly trigger a brief explosion in viral infectivity, and why the flu season typically starts in August and September, when vitamin D is at its peak (see figure below).
Recently there has been a lot of interest in the idea of “super spreaders“. This is the counterintuitive idea that with diseases like flu and COVID-19 the majority of infected people don’t pass on the virus at all and a small number (say 10-20%) are responsible for almost all transmission. In fact, this is now a widely accepted concept of epidemiology – which suggests Hope-Simpson was onto something.
The question remains though: what triggers the brief but deadly explosive outbreaks of seasonal viruses like flu and COVID-19, and what brings them just as abruptly to an end? Hope-Simpson’s observation, that it must have something to do with changes in solar radiation, since it is a seasonal phenomenon which occurs simultaneously in geographically remote places of the same latitude, remains pertinent.
The disappearance of flu in the last 18 months adds to the mystery (and ideas that flu has simply been re-badged as COVID-19 don’t stack up against the huge amount of genetic sequencing of variants that has been done).
Whatever the underlying cause of the strange behaviour, though, some facts are clear. SARS-CoV-2 is not, by any reasonable definition, a highly transmissible virus – infected people on average only infect 10-15% of their close contacts, even at the height of the winter surge (and that is an upper bound as it assumes that all subsequent infections were caused by the index case rather than being co-index cases). This compares to 57% for rhinovirus and 70% for measles – those are highly transmissible viruses. Rather, COVID-19 is subject to the same kind of mysterious and explosive seasonal triggering as influenza is. This probably helps to explain why lockdowns make no clear impact on transmission or mortality, and why the virus does not immediately rebound when restrictions are lifted, as all the models keep wrongly telling us is going to happen.
One lesson from this is we should stop imagining we can capture the behaviour of this strange disease in simple mathematical models and pay more attention to real-world data. Perhaps then we would see things much more in proportion, and cease redesigning our world around our exaggerated fear of it.













To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
Most fascinating, Will. I intend to investigate alternative explanations of disease and ill-health as we try to squeeze reality into a confined, conventional western scientific model.
The Delta variant of the Alpha variant, second cousin twice removed, is suspected of causing tickle coughs after prolonged abstinence from alcoholic beverages and as a consequence alcoholic face masks will be imposed on a 24 ‘ ish hour basis.
For those suffering from a feeling of alcohol overload tests will be prescribed but only with the intent of a confirmatory PCR test.
In line with government guidelines negative tests will not be permitted and recipients thereof will be mandated to self-isolate for a period not less than ten (10) days on pain of a £10,000 fine.
Or summary forfeiture of property to the value thereof.
The government of the United Kingdom remains committed to the principles of Open Liberal,Democracy and its benefits will be celebrated by those we choose to enjoy it.
These seasonality and vitamin D arguments are highly Eurocentric. Epidemics also occur in places that do not have winter. The notion that the rainy season has the same supposed effect as winter also makes no sense. The rains here don’t come like November in Britain with leaden skies from morning to night, but in intense storms that clear away and yield to hours of sunshine. The studies are interesting, but there needs to be comparison with other climates.
I was amazed to discover that Nigeria annualy has the world’s highest rate of influenza. I had always assumed it was a cold climate thing.
From Hope-Simpsons book
”How, then, can we visualize the epidemicity of influenza? If influenzal infection caused an illumination, the northern hemisphere above the tropics would be ringed with lights at night during each northern winter sometime between October and March. As these lights died out they would be replaced by a belt of lights in the tropics in March and April. Then, as north tropical and south tropical lights faded, the southern hemisphere south of 23.5°S would become similarly decorated at night between May and August. Subsequently, as they began to fade, the tropics would again be lit in September.”
“The question remains though: what triggers the brief but deadly explosive outbreaks of seasonal viruses like flu and COVID-19”
<sigh>
C-19 is not a virus.
It is a never ending list of symptoms which now includes the “Indian variant” ie: hayfever
These things matter if we are ever going to get out of this mess
It seems to me that the human respiratory system is never free of respiratory disease organisms, they are always there it is just that normally we can resist their worst impacts. For me, Hay fever this year has been very bad and bad hay fever always seems to go with a summer cold, as if the hay fever symptoms leave you vulnerable to the cold pathogens that are always hanging around. Hay fever is usually worse in younger people and so with this year being a bad hay fever season has lead to summer colds in young people. In my view this is what is fuelling the high number of so called covid cases in the UK, young people with hay fever – summer colds, which are showing up in covid tests.
Pollen allergies are not infections, rather over reactions to mostly harmless various things. You’re right that it’s different this year, on account of the weather pattern (grass pollen affects me most, not trees). Sometimes I have a look at this: https://www.worcester.ac.uk/about/academic-schools/school-of-science-and-the-environment/science-and-the-environment-research/national-pollen-and-aerobiology-research-unit/pollen-forecast.aspx
The other issue is that there was some commentary from a medic last year along the lines that being affected by pollen allergy could actually reduce one’s vulnerability to various viruses, as there is only so much surface area in our respiratory tract. If there are loads of cells attacking the pollen, they’re not available to anything else, apparently. Don’t know if this is true, but could be interesting.
Theoretically yes and no
An over-reactive (allergic) immune system might trigger an early response to invading viruses thus limiting any damage
However
It was the over-reaction of the immune system that made the Spanish flu so deadly
No-body really knows
Anti-histamines seem to be useful for C-19 symptoms
I am interested in the second part of question 1;
”Where is the virus between epidemics?”
Much of our actions on this virus assume it is either rampaging away causing mayhem or has gone away but perhaps it can just hang on in a benign way waiting for a critical moment? Could it be that this is partly what the current UK covid case numbers are telling us? A lot of these cases are dodgy test results but perhaps a number are just the virus doing its normal benign summer circulation around young people, in which case the more it does it early in the summer the better, getting it over and done before the winter.
In farming they have found that some intense livestock system keep stock too disease free and leave them vulnerable and they are experimenting with spraying some young stock with a faecal preparation to improve their disease resistance. Maybe all the current UK covid cases in young people is just nature doing the same sort of thing for the human population?
Maybe ‘vitamin’ D (a controlling hormone) allows the body to expel whatever it needs to periodically in a manner similar to the alternative view of other ‘viruses’ such as measles and mumps being seen as a part of the maturation process in children. (Dr Tom Cowan et al ‘Contagion Myth’). It would account for apparent spreading and geographical differences amongst other facets of disease. May sound ludicrous to those with entrenched classical ideas but worth thinking through.
The seasonality, I suspect, is down to when humans contain themselves in a poorly ventilated box.
Winter in northern latitudes and summer in areas where it gets hot and humid.
The environmental conditions change the way humans behave in a particular location, and it is that change in behaviour that encourages or discourages the viral transmission.
A lot of it is, combined with dietary changes and the reduced amount of ultra violet B from the Sun (used to manufacture vitamin D automatically, via our skin/liver/kidneys), and maybe other hormone variations around the seasons.
Nosocomial……seasonal, but not as you know it.
Covid 19 is an alien. Resistance is futile.
The motto of the NHS should be ‘Don’t go to the hospital or the Doctor in winter.’
Known about for years, which is why the hospital clearances of March 2020 were so lethal; arguably criminally negligent.
‘The prevalence and incidence of viral nosocomial influenza infections in healthcare settings are underestimated. Nosocomial influenza outbreaks are frequent’
‘Nosocomial influenza outbreaks occur in various healthcare settings, especially among the frail and elderly. The correct diagnosis is commonly missed because a substantial proportion of asymptomatic cases can transmit infections.’
https://journals.lww.com/co-infectiousdiseases/Abstract/2016/08000/Nosocomial_influenza__encouraging_insights_and.8.aspx Dated Aug. 2016
Asymptomatic? Droney baloney……..
Presymptomatic
‘…a recent modeling study by He et al.1 inferred that 44% of secondary cases were infected during presymptomatic stages of disease. Here, we raise questions regarding the approach and interpretation of the He et al. transmission model.’
‘other secondary transmission studies have shown that, although symptomatic cases transmitted COVID-19 to 16.2% (34/210) of household contacts, asymptomatic or presymptomatic spread to household contacts was not observed (0/15)
‘….studies on SARS, a related coronavirus with a similar reproductive number (R0) to COVID-1910, provide analogous results. Symptomatic SARS cases spread the disease to 15.1% (101/669) of close contacts, whereas 0% (0/363) of close contacts to SARS cases during the presymptomatic incubation period became infected.’
‘….it appears that asymptomatic/presymptomatic transmission measured by direct contact tracing studies is lower than that predicted by COVID-19 transmission models
https://www.nature.com/articles/s41591-020-1046-6
So, presymptomatic nosocomial…….and the lesson is that if you clear out your hospitals you will kill thousands of the elderly and infirm. If you lockdown millions and mandate masks, you will kill millions worldwide.
But apart from that, really well done……not……..
Drafting the script for a science fiction black comedy show? But yes, there are some old friends in hospitals, known as ‘norovirus’ which are quite common. Occasionally the odd ward is shut down, no visitors etc while they try to eradicate it each winter.
There was MRSA too, when did you last hear about that?
Yet another great article by Will Jones. As a GP I was always puzzled by the behaviour of influenza, and thought that latency seemed to fit what we saw.
on seasonality, Ivor Cumins posted a video where he interviews Prof Gordon Lauc. Haven’t watched it all but talks about seasonality and concludes that it may be driven by time spent indoors and the impact the dry heat has on our first line of defence, eg nose and throat. Very interesting and seems sensible
Here are Dr Naomi Wolf’s thoughts. Sounds plausible to me:
All Covid-19 vaccines are essentially USELESS against new mutant “Delta Variant”
As vaccine-induced deaths begin to accelerate around the world from the dirty Covid-19 jabs, the mainstream media narrative is shifting to cast blame away from the deadly, blood-clotting inoculations and onto a new, more virulent Covid virus mutation called the “Delta Variant.” This variant is just a cover story for actual vaccine deaths, and “there will be blood” on the hands of the vaccine industrial complex. One of the World Health Organization’s doctors (ring leader) is already warning of “reduced efficacy” (meaning it doesn’t work at all) regarding all these Covid-19 jabs, including mRNA and protein payload injections, being useless against the variants that the vaccines are actually creating and spreading.
Covid-19 vaccines make the vaccinated MORE susceptible to catching and dying from mutant “Delta” variant of the Covid-19 lab-made virus
“Delta” Covid is spreading like wildfire across Europe and the United States, and now the “first generation” of Covid vaccines are deemed virtually worthless against it. So how many “generations” of Covid and its variants will there be, and how often? Will Americans need a booster shot every three months, forever? They won’t like that news.
Run for your life… it’s the invasion of the mutants of Covid-19. All vaccinated humans should remain on lockdown, masked and quarantined in their own basement until further notice, as the vaccines have proven to make you weaker, more susceptible to mutant variants of Covid-19. Meanwhile, “Delta” picks up steam, like a hurricane, across the USA.
Covid vaccines suffering a “reduction in neutralization” against the Covid-19 “Delta” and “Beta” variants – Well, you can’t say natural health advocates didn’t warn you
Mutant strains of Covid-19 are immune to all Covid-19 vaccines, the WHO has all but admitted it already. The “Beta” variant is attacking the vaccinated in South Africa right now as you read this. The variants are simply a cover story for all the deaths and blood clots caused by the Covid-19 vaccines, and for the vaccinated sheeple who are STILL catching Covid-19, even after vaccination. It’s obvious, as the WHO scrambles to convince all the fence-riders and absolute non-vaxxers that the vaccines still work, they’re just not as effective as they had hoped. At what? Killing folks?
“The goal of Covax is that we need those who are most at risk to severe disease, and those who are most exposed, to receive those vaccines and to be protected,” a WHO (quack) doctor said. Well you can’t have it both ways. You can’t have all these people who are already fighting back cancer, diabetes, heart disease and Alzheimer’s get the Covid-19 vaccines that cause blood clots and heart inflammation; it will kill them. Then they just use fake Covid tests and say they died of Covid, or Delta, or Beta, or some other college fraternity name.
Corrupt WHO doctors say “Double” and “Triple” Covid mutants are on the way to America
Yes, double and triple mutants will further erode the “efficacy” of the whole first wave of dirty Covid-19 vaccines, if it’s possible to reach below zero efficacy. It seems that it is possible, since the mRNA and viral vector jabs make you MORE susceptible to catching and dying from these new, more virulent mutants. So now, Covid-19 vaccine efficacy is a negative percentage, due to risk of catching double and triple mutants.


 Read more
Read more


That may eventually be the case but it certainly isn’t at the moment.
“All Covid-19 vaccines are essentially USELESS against new mutant “Delta Variant”
Shhh … they’re practically useless against all imagined versions! ARR ~1%
This isn’t lockdown scepticism. It’s unhinged anti-vax paranoia. Naomi Wolf is no authority on anything other than feminist thought. Get real please.
Hmm. Of course the consensus is that the theory is complete rubbish. However, the great astronomers Hoyle & Wickramasinghe spent 20 years exploring the possibility and it does seem to explain most of the questions raised:
https://en.wikipedia.org/wiki/Diseases_from_Space
https://www.amazon.co.uk/Diseases-Space-Sir-Fred-Hoyle/dp/0722147546/ref=sr_1_1?crid=24UKXOH4KFW8J&dchild=1&keywords=diseases+from+space&qid=1624693567&sprefix=diseases+from+space%2Caps%2C173&sr=8-1
Great article! One possibility is that the SAR was higher during the first wave when nobody had any testing.
That wave was actually much bigger than the second if you look at a consistent metric like the ONS antibody survey (and ignore official “cases”/”deaths” etc. where the criteria for counting them completely changed between the two waves).
Agree.Will Jones articles always outstanding and worth reading.And nobody in the world can explain with modelling,transmissions dynamics etc the extraordinary graphs of simultaneously excess mortality of Spanish flu 1918 in New York,London,Paris and Berlin,during the autumn 1918 without any airtraffic etc. Impossible to explain with person to person transmission driven.
The Kent Variant was assessed for spread using one of the tests on that FDA removed list.
[https://www.medrxiv.org/content/10.1101/2021.01.13.21249721v1.full.pdf](https://www.medrxiv.org/content/10.1101/2021.01.13.21249721v1.full.pdf)
The Thermo Fisher Taq Path PCR test. Led to a conclusion that it was more dangerous.
[https://www.massdevice.com/fda-warns-on-false-results-for-thermo-fisher-taqpath-covid-19-testing-kit/](https://www.massdevice.com/fda-warns-on-false-results-for-thermo-fisher-taqpath-covid-19-testing-kit/)
Found to be heavy on the False Positives.
So the Kent Variant study was noisy. As is anything using PCR. Word to ATL. If you see PCR being used as a measure for anything, run a mile.
It’s interesting from theoretical point of view. But the problem is huuuge bias toward making c19 something much more than it is. Even when looking at data you have to be careful. PHE is the one that counted deaths as c19 deaths regardless how many days passed since positive PCR test results (this is even without considering problems with PCR testing). Then when prof. Henegen corrected them, they introduced 28 days since positive test to be a c19 death. This is when number of c19 deaths in UK was cut short by 10% about a year ago (remember).
Anyhow, the influenzas they were studying in this article were endemic. Erratic behavior of c19 in Q4, 2019 before it “took off” in spring 2020 (as seen on the React study plot) would suggest it was endemic by then already. As for “taking off” in spring 2020, it might be due to faulty React study. For sure they missed large numbers of people who had it in Q4, 2019 bcs c19 is mostly mild illness, most people don’t make a lot of antibodies (bcs it’s not necessary), and they fade away quickly (people remain immune – memory B&T cells). They also did their study in summer 2020 after panic set in and excess death peak was apparent, so this assumption what c19 apparently did guided their study and presentation of results. Or, as someone mentioned, if peak is assumed to be true, lockdown itself (especially policy towards elderly and nursing homes) caused a lot of people to have their lives shortened by several months by c19, but it would never have happened naturally (if nothing was done, there would be no peak in spring 2020).
These “variants” are not really relevant in any way (even if c19 itself was relevant somehow). I also call BS on the plot from India (a sharp peak after a mild and longer one after which India for sure had heard immunity). Just several links here:
“Rise in infections not caused by a variant.. We now are at a state of substantial herd immunity. Ecological succession of variants does not mean one is more transmissible/virulent. We should have always remained open. A tragedy” —Oxford Prof @SunetraGupta
https://twitter.com/dockaurG/status/1404429320114823176
Concerns about Indian variant continue to be unfounded
https://www.hartgroup.org/indian-variant-concerns-unfounded/
Indian variant over-hyped
https://www.hartgroup.org/indian-variant-over-hyped/
ps. remember that a lot of people are immune to the virus even if never exposed (either they were exposed in 2019, or cross-immunity from other 4 types of common cold coronaviruses, or other types of immunity mechanisms):
Covid-19: Do many people have pre-existing immunity?https://www.bmj.com/content/370/bmj.m3563
The cause is clear to me. he original estimates of transmissibility did not control for household size and the tendency is for immigrant communities from the India subcontinent to have considerably larger households than normal for UK, and they tend to span several generations as well.
Now that they have spread it amongst the wider community the figure inevitably drops. A little bit of real science would help these people (government), but they are quite happy to continue the scare tactics.
And possibly differences in other variables such as pre-existing cross-immunity and genetics (it is well-known that some communities have higher than average genetic similarities thanks to a tradition of cousin marriage). And the main cause is the usual one for all diseases: unreliable data at the start of something new.
Measles and chickenpox might be 90%, not 70%. And the low rates for Covid may reflect – at least partly – pre-existing cross-immunity. That raises the possibility that variants might be better at infecting those with cross-immunity.
As to latency, the obvious one is Freshers Flu. What’s interesting about that is that it is Freshers that get it (not second or third years) so it must be the same (or very similar) virus to previous Freshers Flu, yet where has it been living in between? Why does it take off? My bet is herds. Herd immunity is local and can be very local – if I mix with ten people, that’s my herd.
Ok so Freshers Flu is not an actual respiratory virus – it’s the term given to students who have burnt the candle at both ends for a whole week – partying, drinking, smoking, drugs, shagging, skinnydipping, takeaways, lack of sleep/water/nutrition… if anything more likely to be a dose of chlymidia or scurvy. Or at least it was when I was younger anyway! Poor little mites nowadays just get a swab up the nose and a quiet night in.
I’d like to propose a study that would help solve this “asymptomatic” myth. From what I understand about the PCR test – they run each cycle and then whatever bits of virus RNA come out can then be compared against (in this case) 1-3 SARS-COV2 “primers” – bits of the sequence that are unique to that virus.
This would seem to be purely a software algorithm? So why don’t they do a trial where they test ordinary healthy people for all viruses – I assume that there’s a database with all the virus sequences on so you just run it against the primers for all known human viruses.
Who knows? Maybe they will actually find that SARS-COV2 is truly unique in being asymptomatic (maybe that was the gain of function that the wuhan lab succeeded in?). Or maybe they’ll find that we’re all “cases” of many weird and wonderful viruses.
There are an estimated 10 0000000000 0000000000 0000000000 viral particles on the earth so I think it should be kinda obvious that finding one of these anywhere isn’t how to define an infection, but I’d be curious to find out how many different viruses people have!
The Article conflates SARS2 ( the virus) and covid ( the disease). There are no ‘genetic sequencing of variants’ of covid. They are supposedly of SARS2, but they all seem actually about the ‘spike’ protein. Covid appears now to cover almost all respiratory illness symptoms and quite a few non-respiratory ones in an ever expanding list. Certainly sufferers of hay fever are now included in its list.
Virus don’t ‘go’ anywhere, there are more virus in the earth’s lower atmosphere than there are suns in the universe; ie billions. We swim in a sea of virus continually, weather and atmospheric conditions can and does move this ‘soup’ around the globe and up and down the atmosphere.
Human behaviour is seasonal. It changes with weather conditions and it changes with lifestyle choices and opportunities. Certain times of year, say September/October in the northern hemisphere is a peak of movement as schools go back, people change jobs, houses get rented/sold. Natural local herd immunity to virus changes at these times, and it takes a few weeks before its recovered, hence spikes of infection.
For months we were told SARS2 was not like influenza, hence the reason for not following the agreed pandemic protocols for influenza. Now we are being told actually it exhibits a lot of the same behaviour as influenza and not common (coronavirus and other) colds. These studies/rresults are just used to support whatever the latest need is to keep this evil ‘spell’ alive. The evil black queen casting her ‘spell’ over her lands is happening in front of our eyes, the stuff of fairy tales is turned real. Vast swathes of the population is mesmorised.
This applies also to ATL articles. Its not unexpected that its very difficult to remember when writing about this or that latest study that anything that uses RT-PCR tests to justify any part of the resulting data is flawed. So apparently logical analysis has at its heart something not fit for purpose.
Perhaps its a sign of my age, but my preference in trying to understand what is going on, is to look backwards to analysis that used computers sparingly, before the time of Drosten influenced PCRs , when analysis tended to have to use brain power and seek wisdom from experience. I think it used to be known as the ‘scientific method’ before being replaced by ‘the science’.
Well said. Much of what you explain is just the workings of dynamic balance/equilibrium inherent in complex systems. Adapted over eons to ensure evolutionary success
Vitamin D is deficient in both Italy and Spain, where they have the lowest levels in Europe. The Nordic countries add vitamin D supplements to their food. Vitamin D is found in dairy products as it is fat soluble, the prevalence of zero fat or low fat foods for the past 50 years could explain the chronic vitamin D deficiency in the U.K. in all ethnicities but worse in those of South Asia, Africa and Caribbean ethnicity.
Also statins, which shut down the entire mevalonate pathway
Fascinating article, Will. Thank you.
Where there’s a Will (or two?)!
I wonder if the unseasonably cold weather in April and early May this year could have been a trigger for the current bout of covid? Last spring 2020 there was unseasonably warm weather (pretty much from mid March to early June was wall to wall sunshine), and the covid cases were low over the entire summer, despite there being free international travel, and the eat out to help out thing in August. This year however there was a frost pretty much throughout April and into early May, even in the south of the UK. Indeed April had the 3rd coldest average minimum temperatures on record, the coldest since 1922.
https://www.metoffice.gov.uk/about-us/press-office/news/weather-and-climate/2021/lowest-average-minimum-temperatures-since-1922-as-part-of-dry-april
Interesting conclusion in the referenced 2008 article:
6. Why is the secondary attack rate so low?
The studies we identified found a secondary attack rate of around 20%, impossibly low for a highly infectious virus spread from the sick to the well. If only a subpopulation of the infected, the good transmitters, are infective, this would explain the surprisingly low secondary attack rates. Current estimates of secondary attack rates assume the first case in the family is the index case and is spreading the disease. However, if only a subpopulation of infected persons transmit the disease, the true secondary attack rate could not be accurately determined until we identify the good infectors.
So…. A20% secondary attack rate is impossibly low for a highly infectious virus spread from the sick to the well.
Hmmmmm.
The Delta SAR is 10.7%, about half of a rate deemed “impossibly low”.
Great article and made me recall an article by Jeff Green a few months ago, in particular his reply to a question on Dec 22nd. Here, if anyone would like to read it……. https://virusesarenotcontagious.com/exosomes-vs-viruses/