by Christine Brett

Christine Brett is a freelance market access consultant and holds a Master’s degree in Economic Evaluation of Healthcare from City University in London. Her career spans 25 years in the pharmaceutical industry, with experience in sales, marketing and health economics. You can see her LinkedIn profile here.
Schools are due to open on June 1st for certain year groups after several weeks of lockdown (although this is looking increasingly unlikely). Anxiety and tensions are high. Parents and teachers are worried with unions calling for working conditions to be safe. There are a lot of opinions and data interpretations appearing in the media about children’s susceptibility to the virus. The noise around this topic is adding to the anxiety parents naturally feel about their children returning to school after a period of absence longer than the summer holidays. All across the mainstream media and social media, we are seeing horrifying pictures of children in playgrounds in France playing solo in a chalk circle or being sprayed down before entering school buildings in other countries. Headlines are screeching that children are super-spreaders of flu and other respiratory viruses, so naturally, they must be walking biohazards for Covid. On my Facebook feed, worried friends are sharing letters from headteachers emphasising their concern about children’s safety. But what are the risks really, and how do we rationally make sense of this?
In the interests of full disclosure, I fully understand the anxiety parents feel about their children. My first son was born with a congenital heart condition and spent the first ten days of his life on the cardiac intensive care unit at Great Ormond Street Hospital. He underwent 8 hours of open-heart surgery at three days old. He had his oxygen levels, and weight monitored weekly. He was rushed back into the hospital after having his first set of vaccines. Ultimately, my husband and I decided that since he had survived, we wanted him to live. Yes, I was nervous being around people with a cold, but I wheeled him down the street choked with traffic fumes to take him to baby groups – yoga, massage, singing. We travelled on trains, buses and even planes to visit friends and family.
He died at 19 weeks – the post-mortem showed evidence of cytomegalovirus (CMV) is his lungs. CMV is a common virus that is usually harmless. Most people don’t know they have CMV because it rarely causes problems in healthy people. However, for people with weakened immune systems, it is a cause for concern. For Matthew’s delicately balanced circulation, it was fatal. I always knew he didn’t have a long life ahead with his condition, but he lived a short, fun-filled life.
So I appreciate the fear that coronavirus holds for people. That fear is especially acute for those who are immune compromised be that through age, underlying health condition or generally poor health. And now having two healthy children, I understand the fear parents have about their children and their wellbeing. However, there are other consequences to fear beyond the coronavirus itself. Is it in our children’s best interests to be isolated from their friends? What will the impact be of lengthy social distancing and lack of access to education?
I’ve spent the last 25 years working in health economics – looking at the data about the costs and benefits of medicines and presenting this information to bodies such as the National Institute of Health & Care Excellence (NICE). Part of that work weighs up the likelihood of getting a condition and the risks and benefits of treating it or not. When we don’t know the answers to some of the questions, as with new drugs that haven’t been used widely, we take the information we have and try to predict what is going to happen. This approach is what we describe as modelling- effectively, it is making a best guess. But as time goes on, our knowledge increases. We accumulate actual data. And with that data in hand, we transform our original modelling into a much more accurate picture of the reality.
When coronavirus first hit we were all scared, we didn’t know what was going to happen. It looked like people were dying in droves, and we thought of the worst scenario. We hunkered down to protect our young and eventually schools were closed as the UK entered lockdown on March 23rd 2020. Sweden has been an outlier choosing to not lockdown, and schools have remained open throughout the pandemic.
Sweden didn’t lockdown and didn’t close schools so let’s look at what happens when we don’t lockdown and compare it to when we do as in the UK.
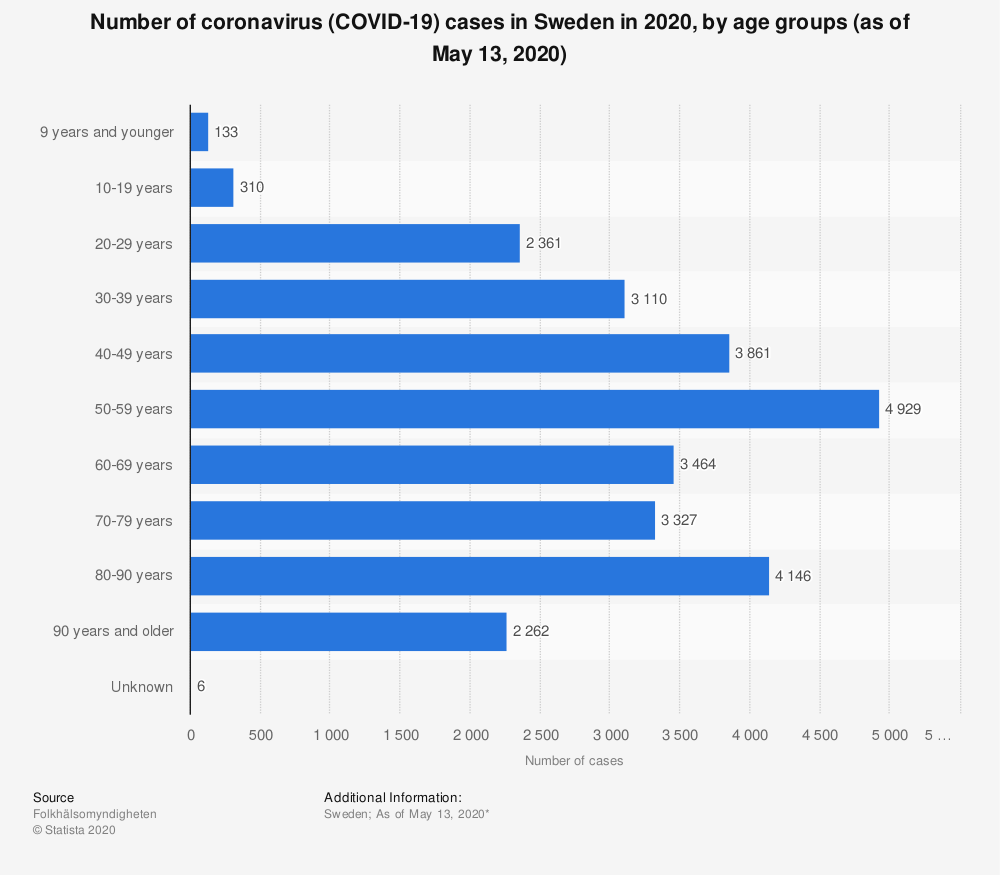
Figure 1 shows there were 27,903 cases reported of coronavirus in Sweden at 13 May 2020. The number of cases in children under 19 years old is 433 (1.5%).
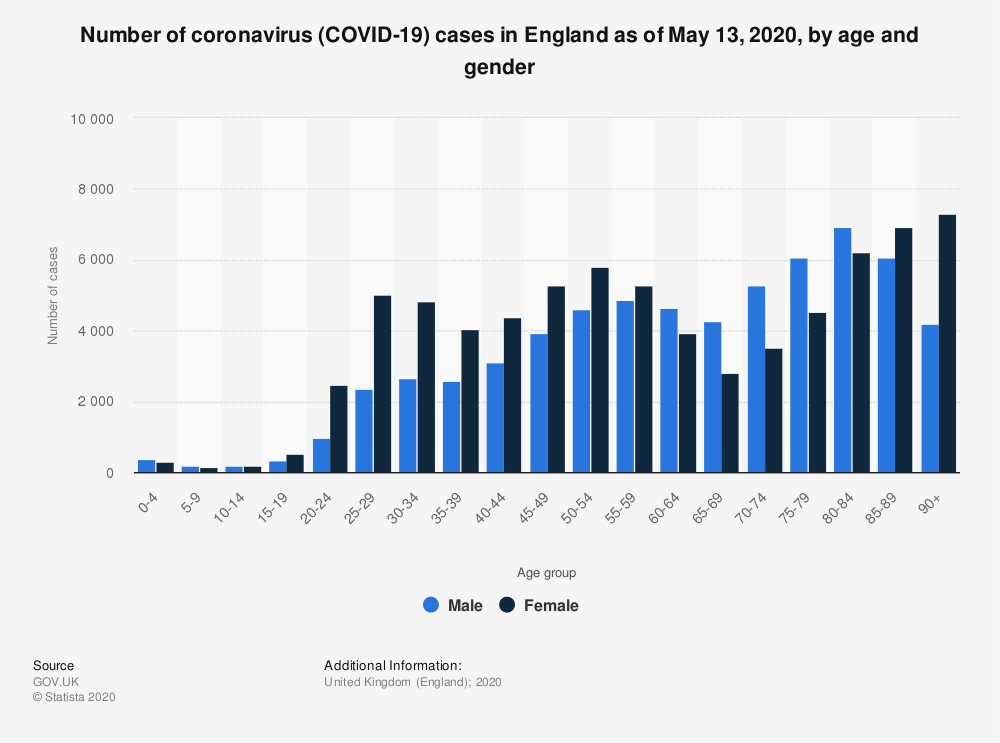
Let’s look at the picture in England. As of May 13th, there were 138,264 confirmed cases of coronavirus of which 2235 (1.6%) were children aged under 19 years. This is shown in Figure 2.
So there is the same proportion of cases in children in Sweden as there are in England. Therefore, despite being at school and not socially distancing and “being exposed” to the virus, more children in Sweden are not getting the virus anymore than the children are in England who are locked down.
However, I recognise there is some uncertainty about the number of cases and the amount of testing. So let’s look at the thing that scares us most – death. Before I explore this data, I must stress again that I know how devastating it is to lose a child. It’s our deepest most primitive fear – parents don’t expect to outlive their children. Every single death is a tragedy and the death of a child is unspeakable. Sadly though, these tragedies happen. During the course of the pandemic, many children have died of causes other than COVID-19. In the same time period that deaths from Covid have been reported from March 6th to May 1st (latest mortality data available other than for Covid), 722 children have died in England, but in nearly every case for conditions other than Covid.
Sweden has reported 3460 deaths in total from coronavirus of which one was of a child under the age of 19 – in an environment where children are attending school as normal up until the age of 15. In England there have been 23,953 Covid deaths, of which 12 have been of children under 19. These figures for both countries are shown in Figure 3.
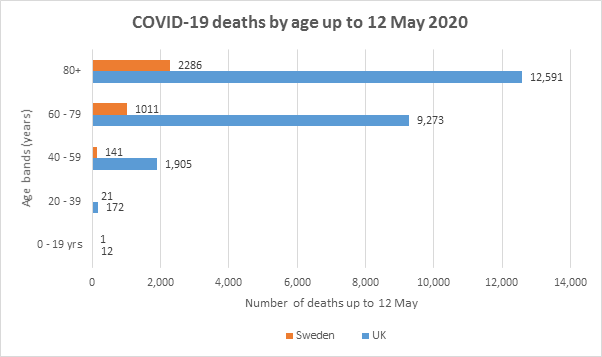
This means that out of the 433 children in Sweden who have confirmed cases of coronavirus (this obviously excludes asymptomatic or mild cases who were never tested), the mortality has been 0.2% and out of the 2235 children in England the mortality has been 0.5%. So over 99% of confirmed cases in both countries survive. The true infection fatality rate is likely to be even higher.
Therefore in the UK, we have had more deaths of children than Sweden although we of course have a larger population. If we take that larger population into account and examine the population of children, we can see that Sweden has had 1 Covid death in just under 2.4 million children and in England we’ve had 12 Covid deaths in just under 13.4 million children. This means that one child has died from coronavirus out of 1.1 million children in UK versus 2.4 million children in Sweden.
So why are we still scared about sending our children back to school? We can see if we look at the data from other countries that regardless of lockdown, children aren’t getting as many cases of coronavirus around the world. Table 1 shows the number of cases of coronavirus in a number of countries and the number of deaths and the picture is pretty consistent.
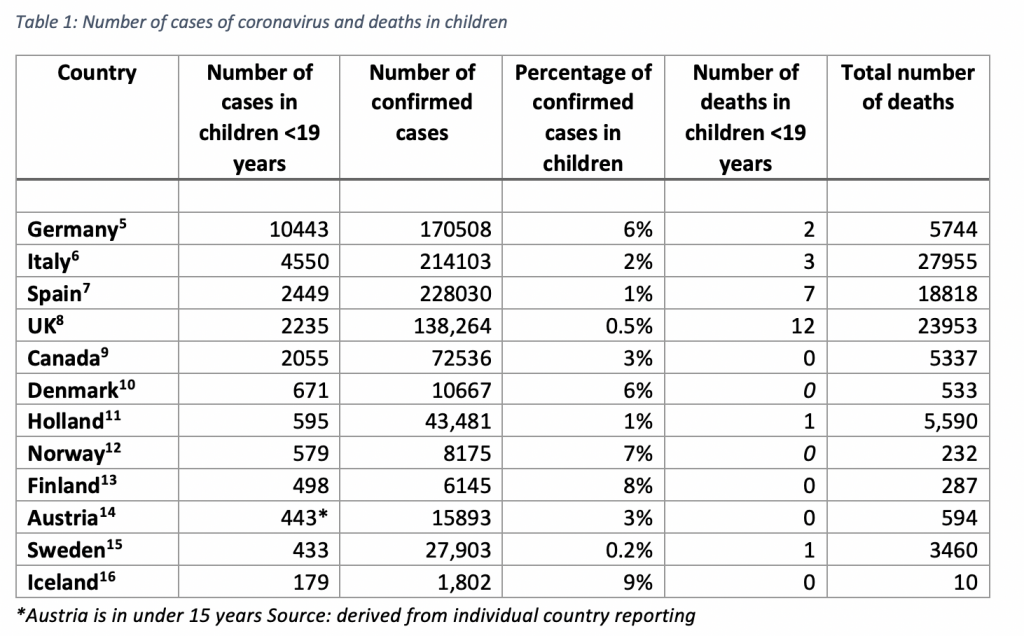
What’s striking is that in terms of number of cases in children, Sweden has the lowest and is the country where schools have remained opened so if children are such super-spreaders wouldn’t we have expected to see more cases there than elsewhere rather than fewer?
A number of reviews have been published on the role of children in community transmission of COVID-19. Munro and Faust looked at studies in China, South Korea, Iceland, Italy, Japan, France, the Netherlands and Australia and concluded that “these data so far have been consistent across regions and continue to push the evidence in one direction” which means that children do not appear to be significantly implicated in spreading coronavirus even to siblings and family members.
Viner et al performed a systematic review of studies on the effectiveness of school closures during the pandemic. They could find no evidence that closure of schools has contributed to the control of the epidemic.
This morning’s Times reported that the “children and adults have the same chance of getting ill” based on newly-published data from the Office of National Statistics (ONS). This survey was conducted on 10,705 people in the community in England and excluded anyone in hospital, care home or institution. Of the 33 individuals who tested positive from COVID-19 from 30 separate households there were as many children who tested positive as adults. However, what the data don’t say is how many of the 10,705 who were tested were actually children! The numbers are quite low to be able to draw any robust inference and we know that the majority of these infections take place in hospitals and care homes which house the population at risk – the elderly and those with other illnesses. If indeed there are as many children in the community who are testing positive and they are not presenting for treatment it must be more likely that they are asymptomatic. It will be interesting to find out as this survey continues whether there are children who are testing positive with no adults testing positive in the same household. Then we might be able to add more meaningfully to the evidence around transmission.
The fact remains that most of the available evidence so far points to the fact that children are not spreading coronavirus or suffering from it. Closing schools as the government deemed unnecessary initially was an emotional rather than a scientific response. The majority of cases are in adults and the vast proportion of deaths are also. Whilst there have been some cases of severe reactions in children lately, it is unclear whether this is related to their underlying co-morbidity and their immune response to the virus.
Having reviewed many submissions of new drugs and devices in my career, I think we have more data than most for making a decision. We have data available from lots of other countries as well as our own which is not always the case.
Given the volume of available data, the question must be asked – what further evidence is needed to make that decision and what is the cost of acquiring it? We never have all the desired information about a new drug before it is approved, and we make decisions to use it without testing it on every patient who is ultimately prescribed. There will never be perfect information that can guarantee 100% safety but we balance the risk of the drug having a side-effect with the need to relieve the symptom.
If we do not accept the data that is already out there, are we any more likely to believe it if we wait to see what happens when other countries open their schools?
As much as I understand a parent’s desire to protect their child, from the risk of illness, as I did with Matthew, we cannot do that at the expense of them living. Being isolated from their friends, washing their hands until they bleed and wearing masks which ultimately reduce the oxygen intake and suppress their immune system is likely to do more harm than if they catch coronavirus.
Liz Cole helped with the editing of this article.










To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
I think you mean the true case fatality rate will go LOWER. That would be the case as the true number of infections is determined.
BBC radio More or Less last night (20/5) https://www.bbc.co.uk/programmes/m000j949 had a very good piece on the risks around schools re-opening. (ie there are none!!)
I think more notice should be taken of this programme.. especially by the rest of the BBC. It is the only programme that actually looks into facts with any accuracy and without the usual BBC bias and prejudice. In fact a bit of an outlier.. Surprised that the management let them get away with it.
also last night’s programme had interesting piece about the german covid figures.
The behaviour of teachers in the COVID-19 crisis is actually very easy to understand, even if it’s infuriating to see the consequences. Most teachers exist in an environment where they are permanently terrified of being accused by anyone higher up the chain, or a parent, of falling short in any one of a myriad different ways. This includes anything to do with a student’s welfare or safety even where the allegations are ridiculous or even invented. Every trip, every activity is preceded by laborious risk assessment processes, and mountains of paperwork. However exemplary a teacher’s career record it can be destroyed in a few minutes by a single malicious or a mischievous allegation, or a genuine but innocent mistake however minor. I know of one instance where a teacher with an outstanding record stretching over decades inadvertently uploaded to the school website some confidential information. He realised his mistake almost instantly and removed the material straightaway. Nonetheless the school management, anxious to reduce its complement of expensive older teachers gave him the choice of resigning or facing a disciplinary investigation on the grounds that he had compromised safeguarding. He left teaching.
School hierarchies are byzantine too. I did work in one for nine years, and my wife taught for 35 years, so I know about all this from firsthand.
This has created a culture where initiative is stifled and where taking responsibility for anything is something not only many teachers try to avoid, but are also even told to by unions. As I recall unions discouraged anything to do with school trips on the basis that teachers were expected to take excessive responsibility. Of course many teachers do resist and go ahead but they still fall over themselves to cover their backs.
The net effect is that confronted with this crisis a lot of teachers are literally paralyzed with fear – not necessarily of the virus (which is how it’s being expressed) – but of being accused of anything. They already were paranoid. These primary schools packed with taped off areas and showcase COVID arrangements are just that: they’re there primarily to showcase the headteacher and teachers as being beyond reproach. The whole thing is designed to deflect allegations and accusations and just reflects an elaboration of what schools are like now anyway. In that sense it’s part of a culture of competitive virtue-signalling but now it’s taking schools into an environment where they will literally be unable to fulfil their remit by trying to operate these new zero-risk set-ups.
Such an accurate assessment!
The first comment I received from the staff at our pre-school was “What’s going to happen to us if a child gets sick? We are going to be blamed.”
Christine Brett’s article is reassuring and inspires confidence.