About 15 years ago, one of the runners in our training group announced that he was going on a carbohydrate free diet. I thought he was mad. Initially, I thought he was just giving up sugar, but when questioned he said he was also giving up rice, potatoes, pasta, bread – basically all carbohydrate. This simply didn’t make any sense; it was crazy. Where was he going to get his energy from? How would he be able to run?
Skip forward about seven years, and I started to hear a lot more about low-carb, high-fat diets. It seemed that quite a lot of athletes were adopting this, particularly those in the ultra-running community. Perhaps it wasn’t so crazy after all. After doing a bit of research, I came to the conclusion that there may well be benefits, not just for weight loss (which I wasn’t interested in) but for improving the immune system and, better still, helping my running. I was keen both to boost my immune system, as repeated coughs and colds had jeopardised training over the years, and keen to avoid hitting the wall in marathons. So, with this in mind, I stuck to a low-carb, high-fat diet for about a year, just to see how things went and how easy or difficult it was. This happened to coincide with a period of plantar fasciitis, which meant I wasn’t able to run much, perhaps a good thing as it was quite difficult to stick to the diet even without the complication of competitive training. What I did find was that I was not troubled by coughs or colds for most of that year, and when I did catch a bug at the start of my summer holiday, I recovered much more quickly than normal and was able to do some light running by the end of the week.
In all my research and during my own travels into the world of the low-carb, high-fat diet, the fact that this type of diet might also help those with mental illness had fallen below my radar. So, I was interested to read a case report in the Frontiers of Nutrition this month about three people who had achieved full remission of major depression and generalised anxiety disorder on adopting this diet (ketogenic metabolic therapy).
Psychiatric conditions such as schizophrenia, depression, bipolar disorder and binge eating disorder, are neurometabolic diseases involving glucose hypometabolism, neurotransmitter imbalances, oxidative stress and inflammation. These disturbances can be modified by use of ketogenic metabolic therapy (KMT), otherwise known as a low-carb, high-fat diet. So, what you eat can directly affect how you feel. I think that, at heart, we all know this even if just from eating too many travel sweets on a long car journey and feeling a bit rubbish for the rest of the day.
Insulin resistance in the brain results in glucose hypometabolism and a vicious cycle of unmet energy needs. Unmet energy needs in the brain manifest themselves in cognitive impairment (mental fatigue, memory problems, confusion), emotional symptoms (irritability, anxiety, depression) and physical symptoms (headaches, dizziness, weakness). Although the brain primarily uses glucose for its energy needs, it can adapt to using ketones as an alternative fuel.
In a low-carb, moderate protein, high-fat diet, there is a shift from using glucose to using ketone bodies as the primary fuel source. The ketones provide the brain with a more efficient energy source than glucose and may be exerting other beneficial effects on the brain. Studies have shown that a ketogenic diet improves mitrochondrial metabolism, neurotransmitter function and oxidative stress/inflammation, while also increasing neural network stability and cognitive function.
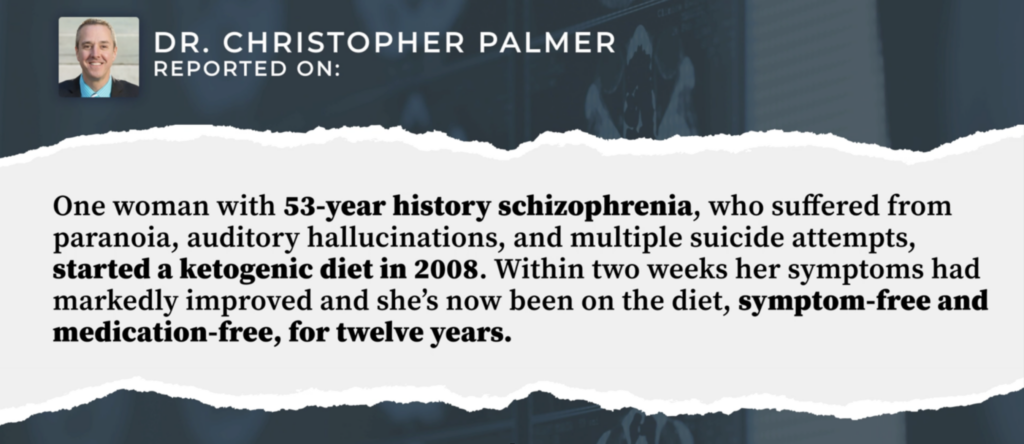
low-carb, high-fat diets can be very strict, with the fat to non-fat ratio as high as 4:1. Interestingly, these diets have been shown to have some usefulness in paediatric epilepsy, and reports of this go back as far as the 1920s. But lower fat-to-non-fat ratio diets, which provide more variety, have also been shown to alleviate many mental disorders. There is evidence that they may be effective in schizophrenia, anxiety, autism spectrum disorder, major depressive disorder, binge eating disorder, ADHD and obesity.
Slide from summary of the Norwitz paper
All three cases in the current study involved complex presentations, including major depression, generalised anxiety, other anxiety disorders, and comorbid psychiatric conditions. The subjects underwent a personalised, whole food, animal-based, low-carb, high-fat diet (KMT) for 12-16 weeks. The treatment plan included twice-weekly visits with a dietician, daily photo journaling and regular blood tests. Additionally, they received support through virtual groups and family and friends. The regimen was complemented by nature walks several times a week, as well as community-building activities.
It is difficult to evaluate how much the added extras in the treatment plan contributed to the results – perhaps if people had more time with family and friends, and spent a bit more time out in the countryside, they would feel a lot better too. The effects of exercise on mental wellbeing can’t be underestimated. In his book Spark: The Revolutionary New Science of Exercise and the Brain, John Ratley details several case studies involving anxiety, depression, attention deficit disorder and addiction, demonstrating the effectiveness of exercise in these cases. So, the walks in nature are a definite plus in this case. However, this can only partly explain the results, which were quite startling.
In case one, the subject reported “increased mental focus, increase energy, renewed confidence and motivation to return to work. Within four weeks of initiating KMT, he secured a demanding full-time position exceeding his previous experience; after eight weeks, he was given additional responsibilities, handled them well and began three online college courses.”
The second case reported “increased mental focus, more patience with co-workers and family and stated he no longer felt a general pull of anger all the time”. While, for the third case, complete remission of depression occurred. After a total of eight weeks of consistent nutritional ketosis, she said: “I don’t have it anymore. I’ve just noticed, I’m happy all the time, which is funny.”
In this study, the participants were very heavily supported, e.g. they got more than a 5-10 min appointment with their GP and a prescription for anti-depressants. However, the time invested was well spent. When I worked as a community pharmacist, I was shocked by how many anti-depressant prescriptions I was fulfilling. On one occasion, hearing that the price of a popular anti-depressant was about to rise dramatically, I purchased the wholesaler’s entire stock. I didn’t need to worry that I would end up with out-of-date stock; those hundreds of packets of anti-depressants weren’t on the storeroom shelf for long. I felt that there must be something wrong if I was dispensing repeat prescriptions for these drugs; either they work or they don’t. The repeat nature of the prescriptions suggested to me that they didn’t work. But at the time, I didn’t know what the answer was; could something as simple as a change in diet be the solution?
Adopting a low-carb, high-fat diet is not easy. If you go down to the shops on the ground floor of our hospital, you will be hard-pressed to find anything that you can buy for lunch if you are on this kind of diet – perhaps a packet of cheese from M&S, but you can’t eat that every day. I found that you had to be super organised (possibly not something that comes naturally to most of us, especially while depressed) and you have to be quite determined, even stubborn, to stick to it in the face of colleagues birthdays (“come on, have a piece of cake”), restaurant visits (“so you want the burger but you not the bun or the fries?”) and family meals (the kids don’t want to eat that kind of food). It was also more expensive than a normal diet and I found it a little difficult to find the variety of things that I wanted to eat. Maybe I should have done what my husband does and just eat more cheese and nuts, but at that time I was the only member of my family adopting this diet, so I found it quite challenging. If there were a bit more support, as the people in the case studies had, then I think it would be a lot easier for people to stick to the diet and see the benefits. It was notable that at times the subjects of the study required some supplements, e.g. acetyl-L-carnitine, vitamin D and magnesium glycinate, and these additions would not be something everybody would necessarily consider if they adopted this diet without support.
This might not be the solution for everybody. As the authors note: “this case series is limited by describing only three patients, which limits the generalisability of our results as well as the inherent selection bias, as they were interested in KMT after failing standard therapies.” Certainly, without support and without the desire to see change, it will be a non-starter. But for those who are determined to beat their mental disorders, it provides a relatively simple, drug free solution.
The “Patient Perspectives” in this paper are well worth reading if you want any encouragement that this can be an effective approach to treating these mental disorders.
Wouldn’t it be better for the NHS to invest in good nutrition rather than investing in drugs that clearly aren’t working? Major depressive disorder and anxiety are neurometabolic disorders. Doesn’t it make sense, then, to treat them with nutrition rather than medication? The NHS might like to start by changing the Eatwell Guidance, where fats are a tiny slither on the chart, instead of >50% of the dietary intake that they probably need to be.
Dr. Maggie Cooper is a pharmacist and research scientist.












To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
An astonishing article!
Is the author unaware that our new government is utilising the very latest in management techniques: ‘Mission Oriented Management’.
Me neither.
Here’s a handy guide:
https://www.forbes.com/sites/brettsteenbarger/2015/07/19/mission-based-management-the-leadership-of-purpose/
They are going to end sticking plaster politics:
https://labour.org.uk/wp-content/uploads/2023/02/5-Missions-for-a-Better-Britain.pdf
Great! I mean, what could possibly go wrong?
It’s easy. Look:
https://labour.org.uk/change/mission-driven-government/
‘We trained hard—but it seemed that every time we were beginning to form up into teams we were reorganized. I was to learn later in life that we tend to meet any new situation by reorganizing, and what a wonderful method it can be for creating the illusion of progress while actually producing confusion, inefficiency, and demoralization.’
(Apparently some disgruntled soldier of a literary bent, whether commissioned or noncommissioned I do not know, pinned this ‘quotation” to a bulletin board in one of the camps of the armies occupying Germany sometime after 1945 (the style suggests a British occupying force). Since the sentiment is impeccable, whether applied to military, governmental, or academic administration, it has enjoyed a cachet borrowed from Petronius (60 AD) ever since.)
In different words: ‘We are comprehensively fecked!’
Also attributed to a Roman soldier. So probably one of those things that has been a truism from time immemorial
I look at this Parliament as the second innings of brown and Blair, even if they are only in the background. Starmer is a puppet and his legal background means he is only capable of taking instructions. No moral integrity.
Look at those beady eyes. Him and that cretin Miliband can hardly believe their luck that the Tories turned into Labour lite and threw away an 80 set majority. They are rubbing their hands with glee. Miliband cannot wait to rip out your gas central heating
The Tories did not throw away an 80 seat majority, they engaged in controlled destruction as they had been ordered to.
As mentioned in the book by Nadine Dorries.
Interesting theory. ——–I won’t disagree with you, but maybe I would put it differently. I have no evidence for “controlled destruction”.—– I have always been of the opinion the extraordinary claims need extraordinary evidence and I do not have any for “controlled destruction”, but ofcourse it depends how you choose to define that. ——-I certainly think the Political Class are up to no good and are selling us out to globalists.
Actually upon further consideration “controlled destruction” is probably a good term for all of the things that are going on.
Nails it.
You couldn’t make it up, but they did.
GB News is showing all the new parasites moving into 10 Downing Street. Parris 1940 comes to mind.
Yep, the front bench is looking very, what’s the word…? ‘Diverse’. And here’s the new Justice Secretary;
https://x.com/DaveAtherton20/status/1809517291656101951
Sweet Jesus!
That’s a cracking start. Well at least the nations of the world know which side we are on. That’s what I would call nailing your colours to the mast.
Excellent article. Could not agree more about the competence and excellence crisis we are in. Mediocrity abounds, and many young people seem to think that trying hard is good enough. They are Minnows compared to the generations of the 1900s to 1960s.
A good theory that the left are mostly incompetent, university mis-educated, 2:1 achieving, fools, who have a high regard for their rather poor intellect.
Shades of Kamala Harris in that Mission Statement.
I would rather have the Raving Monster Loonies than this rabble of squirming eco fundamentalist mass immigration parasites.
Is it not also that English is being replaced by a sort of pidgin language, enshittified English?
Good point.
I have always regarded the deplorable use of written English as the fault of a failing education system. I think I am only partly correct. If this country is to be dismantled, and it is, then it makes sense that our beautiful language must also be dismantled.
English as a language that we love is to be bastardised and turned into some crude, lowest common denominator amalgamation of ghetto gutturals. How often on here do we remind ourselves of the need to protect the language?
Innit?
True dat, Blud!
Fanks for that Bruvva.
And yet another incompetent. Valance apponted Science Minister! I am just waiting for Neil Fergusson to be put in charge of implementing IT in the NHS.
Our computer models predict that half a million people will die in the UK over the next 12 months.
Panic!
On a serious note I do believe excess deaths will rage ever upwards under this Government and not just as a result of the injections. If misery and despair take hold as I fear they will our mortality rate must increase. Increasing living costs, loss of freedoms, hunger and cold will inevitably take a toll.
“people of the profoundest mediocrity.”
To describe any Labour people as “people of the profoundest mediocrity” is decidedly a gross exaggeration of their abilities.
Delusions of adequacy.
Aspiring to mediocrity?
I am amused that today the BBC weather presenter said that “temperatures this week will be lower than average”. This is an ideal example of the above, in that temperatures above average are “climate change” and ones lower are below “average”. The lack of mathematical understanding of the word average is astounding, instant knowledge-less mediocracy!
If we want a new Britain we need to end the welfare state and redistribution of wealth (Ha!) via the tax system as we are become a Nation of parasites each demanding to live off the other.
Back to property rights, autonomy, self-reliance, self-responsibility, self-sufficiency.
… while each western government is expecting to import Energy from its neighbour when the Wind doesn’t blow and the Sun doesn’t shine?
Good article. Although I disagree with the premise that malevolence and stupidity are mutually exclusive. I think what we’re observing culturally is because the exact opposite is true – they are joined at the hip.
New Britain is an island in Papua New Guinea. Perhaps this document indicates that the UK is to be refashioned into its lookalike.
Papua has over 800 known languages. Which must make the London Borough of Tower Hamlets look very non-vibrant. The regions of the UK are perhaps to become like the viable units of Papuan communities. The palm trees are already there in Torquay and Eastbourne.
Well those PCR tests are a bit like the initiation rites carried out there.
Is the country house like Miss Haversham’s? A coal from the fire slips out of the grate.
Unfortunately, though large sections of HS2 were cancelled, it left people without their property that had been compulsorily purchased, and others with the possibility that the scheme could be revived, rendering their property unsaleable.
The ancient woodland that had been destroyed and replaced with new ancient woodland (as if the flora and fauna of the old knew where to relocate to the new) obviously could not be regained. Quite accidentally the whole project became a giant archaeological dig.
I read an article in The Telegraph about this and,apparently, it is included in the Manifesto which means The Lords cannot prevent it. I couldn’t spot it, according to the article it is a vague reference to “implement S…”. As one expects with Labourious, there is no detail whatsoever. They did not want anyone to know what they intended, did they?
I’ve mentioned it to a few people and what it means but just get a sort of vague, shutters down, reaction. It’s as though taking away democracy is far too much like Astrophysics for them. The Sheeples who voted Labour are now horribly akin to the Jews who thought getting on a train was a good idea when they listened to the last lot of Antisemites to rule completely.
McGrogan for PM! The effect of socialism and communism has always been levelling down, not up. Excellence is unrewarded, conformity is a virtue. We needs goats,not sheep. As for the appointment of Patrick Vallance to direct science from the House of Lords… one can only hope that another old saw comes to pass – those whom the Gods wish to destroy they first drive mad.
Unlike the author, I believe this crackpot bunch of lefty loons will implement this. Look at their manifesto and, more importantly, listen to them attempt to speak. When asked to define “a working person”, Kiernocchio and his laughable Chancellor (who looks uncannily like Matt Lucas) could not agree. Yet their “Manifesto” states those unidentifiable Persons will not face NI, Income Tax and VAT rises.
They believe there is little point in details, it’s the soundbite that matters. Judean Peoples Front writ large, or is it The Peoples Front of Judea? Who cares, implement it! I’m wondering which one of the non-entities is Wolfy “Foxy” Smith?
I am wondering which of them is more of a comedian than John Cleese! There is enormous competition.
Starmer’s father was a toolmaker, in case you hadn’t heard.
Do you think he may have made one?
Here is something to think about. The travellers arrived here (like they do like clockwork, every summer) on Friday and parked their motor homes in the council car park, on the seafront, Exmouth, Devon. The council have to take out some sort of order to get them moved, but cannot do this over a weekend as the travellers know.
The police are actually scared of them, and won’t go near them. So far they have parked illegally, taking up 12 parking spaces, did not pay to park, tossed all their rubbish out in the car park and use the area behind their motor homes as a toilet. One of the men harrassed two of our lady bowlers, following them into our bowls club. The traveller children wondered into our club on a fact finding mission. They were shown the door. I dare anyone else to come park in this car park for three days without paying for your parking. You will be ticketed multiple times by the traffic warden.
So you see, the police are scared of a few travellers and refuse to protect our rights to a safe environment. When a young aggressive man harasses old ladies, things have gone too far. If and when the general public have had enough of the incompetence of government, can you imagine how scared the police will be. Public disorder is not something any country wants.
I suspect that public disorder is not very far away. There comes a time when even Britains may follow the French example of retaliation. Labour have no proper mandate, and Reform have a huge mandate but only 5 seats. Starmer should consider that very carefully.
“ French example of retaliation”. There remains 121 Conservative MPs (mostly Wets) which may demonstrate that there are still an awful lot of people of a Right wing outlook still look to that party rather than Reform to turn the rotten ship of state around. In our solid blue constituency with a Remainer MP we formed a Reform group and could hardly muster sufficient activists to leaflet the constituency. Most of our Reform members were just too timid to become activists. Not an ounce of rebellion in 95% of them. The Remainer MP just scraped in with Labour second and Reform third. When the Right start to match the activism of the Left then things will change but sadly most on the Right are presently just too timid.
What, in any event, does one say about the future of a country like this? The image that increasingly comes to mind when I dwell on these issues is one of an attic in a dilapidated country house, dusty and mildewed, with many old spider webs strung between the rafters. Brittle and frail, these strands of gossamer still somehow cling to the physical realm and to physical existence because the still, stale air does not contain quite enough movement to dispel them into nothingness. But all it will take is one decent breath of wind, one strong draft from a suddenly opened window somewhere else in the house, for them to be swept away forever.
Best paragraph I’ve read for a long time. Worth memorizing.
Hi David
I think you have gone off track a bit here and it sounds more than a bit snobby. Yes excellence matters, but the truth and coherence matters more.
A well written plan on how to spin and lie and manipulate is not better than a poorly written and misspelt attempt at the truth.
The problem is not that the political class can’t write a manifesto well, its that they do not believe in anything more than trying to justify themselves in power; which you were finally able to succinctly summarise well and usefully for us in your references to Machiavelli and the Prince and the Republic.
I don’t however think that such a lack of belief necessarily leads to a lack of penmanship, and it does not help to try to make the link. Although I would not dispute that all virtues in the end must enhance each other.
The problem is a lack of belief in that man is made in the image of God, and that this necessarily must entail the gift of freedom and responsibility. Such freedom and responsibility is only enabled in a republic type format of government whether you can spell or not. Of course you can leave the God bit out and instead say that human flourishing properly understood entails freedom and responsibility, not dependency and nannying, and therefore requires a republic form of governing.
The reason why the conservatives lost is that they only believe in power and not individual people and we have now had enough of their 14 years of growing incoherence for the individual man in the street. Unfortunately the population as a whole has now given Labour a chance to play the same (what change?) game whether they can spell it right or not. The next 5 years will therefore be even more incoherence for the individual, but this time on steroids.
Did Kamala Harris write this?
Were the authors inspired by Kamala Harris’s gnomic style, I wonder? There is an uncanny resemblance between the particularly awful sentence McGrogan invites us to read out loud and the following remarks by the Vice President at the 2022 U.S.-ASEAN Special Summit:
In the best collectivizing spirit, Kamala squeezes in not three but four ‘togethers’!