The flu was substantially suppressed across much of the world for the first two years of the Covid pandemic.
Many, many people disagree with me on this point, more than ever before. While I’m generally happy to let ideas I think are wrong persist alongside my own point of view, this is an exception, because it touches on the phenomenon of viral interference, which is very real and very important.
Properly understood, viral interference calls into question the entire rationale for non-pharmaceutical interventions to slow the transmission of viruses, and suggests that mass vaccination against old endemic pathogens like influenza is a very bad idea – even in a fantasy world where those vaccines are absolutely safe, and especially if they’re in any way effective.
I want to be as clear about this as I can, so I’ll pull a Pueyo and tell you what I’m about to say before I say it:
- I’m going to explain how we know influenza infections were heavily suppressed, especially in the first year of the Covid pandemic, from data that have nothing – zero – to do with mass pandemic testing.
- I’m going to explain why viral interference is such a conceptual problem, and how it becomes easier to understand if we drop one of the core assumptions of epidemiology.
- Finally, I’m going to suggest that ordinary endemic viruses are an important defence against potentially dangerous novel pathogens.
This is not a post about mass PCR testing and its reliability. Even without mass testing data, we have good reason to conclude that Covid coincided with the widespread suppression of influenza.
That said, it’s very important to acknowledge that influenza testing changed drastically after March 2020. Equally important is the fact that influenza was never diagnosed via mass PCR testing, as Covid was, and this makes it easy to get lost in meaningless apples-to-oranges comparisons. Furthermore, there is no denying that the raw number of flu tests fell nearly to zero for the entire space of the pandemic period. Finally, there existed in most jurisdictions considerable financial incentives for diagnosing Covid infection in as many patients as possible, especially when those patients died.
These points raise grave questions about the integrity of our pandemic-era influenza data, but they don’t make a positive case in either direction. In what follows, and for the sake of argument, I’ll assume that ordinary diagnostic influenza testing ceased the world over on March 1st 2020. I’ll assume that the WHO FluNet statistics and CDC numbers are hopelessly confounded.
Evidence for influenza suppression after 2020
I’ve made my case for what happened to influenza during the pandemic multiple times, and I suspect that none of you want me to rehearse that in detail ever again. If you are, however, interested in links to the data and closer discussion, please see this piece on the ‘Mysterious Disappearance of Influenza‘ and this piece on the phenomenon of viral interference.
Here I’ll simply spell out the main points. There are four of them:
1. Various jurisdictions have small self-contained influenza surveillance programmes. Mass Covid PCR insanity did not affect these programmes. In Germany, participating sentinel clinics swab patients with respiratory symptoms and send these swabs to a testing centre. During the pandemic, they tested each of these swabs for each of seven viruses: rhinoviruses, ordinary human-infecting coronaviruses, influenza, RSV, parainfluenza, human metapneumovirus and SARS-2. They’ve been doing this for a long time, yielding a wealth of data going back years about the seasonal patterns of the endemic viruses we live with. And this is the key point: after March 2020, influenza disappears entirely from German sentinel clinic swabs. Other viruses are heavily suppressed but not totally gone; only rhinoviruses seem unaffected.
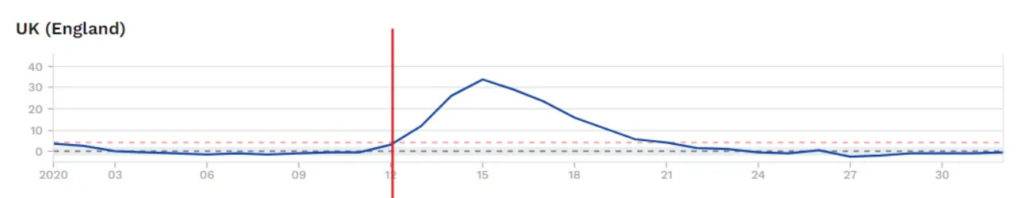
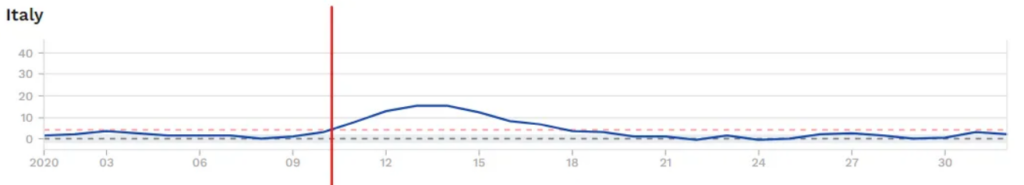
2. The behaviour of influenza, at the population-level, is seasonally distinct. In most places, flu infections peak in February or March. Rhinoviruses, by contrast, are most active in the autumn and the spring, and other respiratory viruses are most prevalent around the winter solstice in late December. If influenza were merely rebranded as Covid or overlooked by the pandemic-era testing regime, we’d expect fever gauges like Grippe Web to show the usual double-peak of virus respiratory systems, with one peak for the solstice viruses in December and another peak for flu after January. We don’t see that. For the crucial 2020/21 season, the post-January influenza peak is totally missing, and the solstice peak is anomalously low, in fact barely perceptible. These data are independent of all virus testing.

3. Very much in contrast to Covid and the other common respiratory viruses save RSV, influenza causes a small yet nontrivial number of hospitalisations and deaths in very young children. If flu were overlooked or rebranded as Covid during the pandemic, we’d expect to see the usual flu-related February and March hospitalisations and deaths in this age cohort, but we don’t. They’re totally missing. This is another data point totally independent of mass testing.
4. Viral interference is very real, and it has been observed for a long time. Some of the most convincing data emerge from studies of the 2009 Swine Flu. In this over-hyped ‘pandemic’, a new H1N1 flu strain spread across the globe, causing mild symptoms in almost everyone. For humans, it was a nothingburger, but for the world of viruses, it was very disruptive, because viruses don’t have to be extra special or especially dangerous to upset the viral ecosystem. Ordinary human-infecting coronaviruses were heavily suppressed across the entire 2009-10 season. Almost nobody locked down for the Swine Flu, there was no mass PCR insanity, and yet multiple studies attest to a clear interference effect.
How viral interference probably works and why standard epidemiological assumptions are wrong
Viral interference does not – cannot – involve the direct competition of viruses within the same host. Only a small minority of the population (generally 2-10%) suffers symptomatic respiratory virus infection at any given time. Many influenza-shedding hosts will never encounter a single SARS-2-shedding host for the duration of their symptoms. And yet, viral interference happens.
What is going on?
Here it will help to consider all the other phenomena we’ve been treated to since 2020 that the virus ‘understanders’ are equally powerless to explain:
- How is it that waves of infection generally collapse of their own accord, well before burning through the entire population?
- Why were non-pharmaceutical interventions, especially lockdowns, so powerless to do anything about Covid mortality?
- And, above all, why were the virus models so invariably, irretrievably wrong all the time?
We are labouring under a serious error, and that error is to be sought somewhere in the SIR model of virus transmission. In the deceptively logical, simple world of SIR (which underpins not merely virus computer modelling but much epidemiological thought) immunologically naïve people are held to be Susceptible until they encounter the virus. They are then Infected, after which they either die or Recover and are immune.
This model is particularly attractive to the vaccinators of the world, who believe that they can snatch people out of the Susceptible pool by jabbing them, and drop them into the Recovered/Vaccinated column, thereby skipping the dreaded Infected part.
Well, dear readers, we have endured an unprecedented exercise in mass vaccination. It had many effects on virus transmission, but none of it looked like SIR told us it would. Many theories are possible, but anyone who seriously attempts to understand how viruses actually behave must sooner or later throw SIR into the trash.
R. Edgar Hope Simpson, in trying to account for the many oddities of influenza transmission, effectively located the error of SIR in its overly simplistic conception of what it means to be Infected and Recovered.
As for Covid, SIR looks to be entirely too simplistic in its conception of the Susceptible. An ordinary population not subject to a multi-year Chinese hygiene regime has substantial resistance to viral infection in general. Scroll up and look at the German fever-gauge data once more. Note how, across the entire German population, symptomatic infections seem to have serious trouble breaching the 10% threshold. Whenever they scrape it, a collapse is imminent.
Here’s how I read that: innate immune defences are powerful, and they make a solid majority of everybody invulnerable to respiratory virus infection at any given time. Viruses don’t have free run of the entire uninfected population; only a small minority of respiratory tracts are open to them. That Susceptible minority waxes and wanes with the seasons. In the summer, it’s very small indeed, and many viruses drop to nearly undetectable levels. In the winter, the number of Susceptible increases substantially.
We have a good explanation of viral interference, if we posit that prior infection with one respiratory virus knocks the recovered person out of the Susceptible column for many other viruses. Interferon is one likely mechanism here, but there are probably others. If you’re in the minority 5% susceptible and you get influenza, you’re most likely invulnerable to Covid for a while afterwards, and vice versa.
Once we revise our conception of who is susceptible, a lot of things come into focus. We wasted much effort locking down and vaccinating people who were invulnerable to infection in any case. This was entirely useless if not actively harmful, because Covid vaccination, it turns out, does not necessarily take you out of the susceptible column. On the contrary, it has bizarre and unexpected effects on virus susceptibility, often increasing it both in the near- and longer-term. Infection waves collapse well before they burn through the whole population because only a minority of people are susceptible at any given time. Models are wrong because they drastically overestimate susceptibility.
SIR, on closer consideration, is not an empirical attempt to understand virus transmission at all. Instead, it’s a heavily politicised paradigm, useful for exaggerating the threat of respiratory pathogens and justifying technocratic public health interventions like mass vaccination. It persists not because it’s right, but because it’s useful.
Ordinary endemic viruses are a defence against novel pathogens and lockdowns are very bad
The problem isn’t that lockdowns do nothing. It’s that they’re just effective enough to be dangerous. Endemic viruses that have been around forever face the standard constraints of seasonality and the drastic limitations our innate immune systems place on susceptibility, but they’re also boxed in by adaptive immunity. They face antibodies everywhere because they’ve been infecting billions of people since childhood. A newer pathogen, like SARS-2, faces fewer adaptive immune constraints.
When you lock down and put hand sanitiser on every corner, it’s the old endemic viruses that take the hit first. In preventing these infections, you effectively reserve precious susceptible respiratory tracts for the somewhat faster novel virus. We know that SARS-2 was circulating widely as early as autumn 2019, and yet it only coincided with serious mortality as influenza infections collapsed in the course of February and March.
The chronology suggests that influenza, already at the end of its season, was being out-competed in many places by Covid as early as February. Lockdowns are far from the only factor in play here, but everywhere the story is the same: collapsing influenza is a precondition for pandemic mortality.

Influenza is far from the only virus with which SARS-2 competes. It’s almost surely no accident that SARS-2 was at its deadliest in heavily restricted care home environments. These were spaces in which a draconian hygiene interventions spared SARS-2 all competition. Compare the case of the Diamond Princess, where Covid also had access to a lot of old people but could rack up very few deaths, no doubt because of endemic virus competition.
Mass vaccination initiatives to reduce the prevalence of endemic respiratory viruses, including vastly milder Omicron-era Covid, are a very bad idea for the same reason that lockdowns are. Even if they’re totally safe and effective, the risk is that they’ll end up reserving hosts for other, newer pathogens and the unknown risks that these pose.
At the end, a side matter: influenza suppression in the absence of Covid
A common objection is that flu appeared to vanish in many regions that also had very few Covid infections in 2020, such as Eastern Europe and Taiwan. Thus, it is said, we must be dealing with artefacts of testing or behavioural changes rather than a real biological phenomenon.
The problem with this view is that influenza has many unique characteristics that set it apart from other viruses. In some respects, it seems to behave like one pan-regional viral super-organism, evading human immunity via constant mutation and reassortment in millions of hosts. When it’s denied these substantial reservoirs, it suddenly faces significant disadvantages everywhere.
In the past, I’ve written of the ‘disappearance’ of influenza, but here I’ve tried to speak more precisely of its suppression. Mass flu testing in 2020 would have undoubtedly uncovered cases across the world, and perhaps it would have even uncovered somewhat more cases in places where Covid was less prevalent. However that may be, it’s important to emphasise that influenza merely seemed to disappear, because it was not prevalent enough for our (often rather crude) flu surveillance programs to detect. (Some combination of Covid competition and pandemic restrictions does seem to have wiped out the Yamagata strain of Influenza B forever, though.)
This article originally appeared on Eugyppius’s Substack newsletter. You can subscribe here.









To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
Let me help. Flu was relabelled Rona. So too were cancer deaths, dementia, pneumonia, fibrosis, car accidents and dying from being fat. The only change to the death rate was from the March to May murders of some 30K and the dead post stabbinations. Flu was indeed suppressed as were other categories of death.
Indeed you are right Ferd. But your point is not really relevant to Eugyppius’s article, which is a welcome postulation of how the epidemiology may actually work, and shows up the consequences of not trying to reach a better understanding of the mechansim.
I’m glad you followed epidemiology with ‘may’.. because of course it ‘may not’.. 😉
Indeed, i doubt that collectively we know much about our immune systems, or ‘viruses’ real or imagined. But they are handy to invoke aren’t they as the quack Jenner did (what a joke he was). I doubt we have a clue about how ‘viral’ infections spread or even what they are, or what causes the related illnesses. The cure is always a drug and shooting gunk into your bloodstream.
Not sure what his point is and not sure what he means in his painful discourse by ‘suppression’ or the nonsense about ‘competition’. Both need to be defined.
If he means that flu deaths were suppressed yes, we all knew this back in 2020.
If he is invoking in his long painful analysis some darwinian god of suppression/competition/survival of the fittest, than no, that is horseshit. There are 300.000 Rona viruses if you believe in them and whilst differences may exist they would be hard to categorise, as the author admits. This is where the fake test fraud comes marching in.
Some competing ideas in this article.
“ If flu were overlooked or rebranded as Covid during the pandemic, we’d expect to see the usual flu-related February and March hospitalisations and deaths in this age cohort, but we don’t.”
Well if they are being rebranded Covid… we wouldn’t.
Was ‘flu knocked back by competition from the CoV 2 or because of the lockdowns? Would ‘flu not have disappeared in the absence of lockdowns?
We can’t use Sweden as a control as apparently there is some cosmic influence at work that affects influenza around the globe irrespective of local conditions:- “The problem with this view is that influenza has many unique characteristics that set it apart from other viruses. In some respects, it seems to behave like one pan-regional viral super-organism…”
If ‘flu disappeared everywhere, 2022/2023 it was back with a vengeance – where did it come from?
And since we have a plethora of ‘novel’ CoV 2 variants, why aren’t they suppressing ‘flu.
Here’s the problem. The theory of viral competition is sound, but so much data is corrupt, so many lies associated with the whole Covid pantomime, I just don’t think it is possible to support any conclusions based on official data, even the allegedly trustworthy ‘flu surveillance services.
Correct.. the data was and is corrupt. Not one country where FOI requests have been made requiring proof of this so called virus answered. None have responded with data to prove covid19 was real and isolated.. not one. That should tell you if it existed or not.
The flu-gone AWOL argument although well penned and articulate, adds up to doodly-squat in the cold light of day. Just like the desperation to push the lab leak theory.. anything to keep the hoax alive.. Oh its real.. it escaped from a Chinese lab.. B0110CK$
Ha, I didn’t read you comment until after I posted mine. Seems we’re on the same page there. 🙂 Something else I’d add as well is that, flu or no flu, it’s the impact these non-sterilizing death jabs are having on future circulating viruses and the impact on the jabbee’s immune system in being able to effectively fight off future lurgies, or anything else we need our immune systems for, come to that, such as destroying cancer cells before they morph into actual disease. ”Health is wealth”, after all, and I know several people who’s general health has been shafted good and proper and they’re all jabberwockies. 🙁
Good points, but note that the cohort referenced in your first paragraph was clearly stated to be ‘very young children’ – for whom there would be sensibly zero Covid deaths.
You ask “If ‘flu disappeared . . . where did it come from?” Well, I don’t think Eugyppius is suggesting that it was 100% exterminated. It would come back from whatever reservoirs maintained it.
I agree with you about the data corruption, but we have to make the best assessment of what data is available. Otherwise we bury our heads in the sand and are no better than the sheep.
If the data available is corrupted, unreliable, it shouldn’t be used, no matter how eloquent the massaging of it is..
According to this site ‘flu did not disappear.
https://www.worldlifeexpectancy.com/selected-deaths-vs-covid-19-united-kingdom
You can look at other Countries by selecting from the drop-down menu.
I think Eugyppius is rather wedded to his hypothesis. I’m going to be bad and comment despite not having read the article but I would argue that this is all quite the moot point now anyway. On a par with debating if covid was a deliberate/accidental lab leak or not. I think the important thing, which is indisputable, is the evidence that ‘Covid deaths’ ( and ”cases”, come to that ) were massively inflated, with deaths from many other causes misattributed to Covid, all because of the ever-changing definitions and protocols, heavily reliant on the fraudulent mass testing. The testing, which was exclusively for Covid, ( so what do you know? You’ll then find sh*tloads of ‘Covid’! ) resulted in driving the fear porn which TPTB used to abuse us by imposing restrictions, which they did not see fit to adhere to themselves.
And I’m still waiting to see what evidence there was for the ”a death within 28 days of a positive PCR gets ‘Covid’ put on the cert”. And I think it was even 60 days to begin with wasn’t it? Arbitrary numbers plucked from thin air with no scientific rationale. So you can see that that rule alone will capture a hell of a lot of deaths and contribute to those scary-looking stats they couldn’t get enough of reporting to us daily, just to keep us afraid and easier to control, which is what a psycho would wish to do to their victim, and make them more amenable to abuse. Fraud, abuse, mass murder ( via iatrogenesis and toxic injections ) all happened on a humongous scale and the docile, gullible masses must never let themselves be hoodwinked or put in the role of victim again.
I shared it the other day but if you didn’t catch it I’m with Jessica Rose in her latest analysis;
I have said this before and it warrants repeating, this was a pandemic of testing. If this testing insanity had not been ‘a thing’, then diagnoses would not have been dependent on it and death certificates wouldn’t have been alterable using this as a distinguishing feature and there would not have been a way to masquerade pneumonia deaths as COVID-19 deaths.”
https://jessicar.substack.com/p/what-is-a-covid-19-death
Totally agree with you on the testing scamdemic and the fraud of the MCCD. Once the free fake tests were removed, than magically all of the ‘cases’ and hysteria died, and so did the death data fraud. No longer could they call a heart attack death, Rona. We can note that the PCR Test for Sars II was patented by the Rothschilds in 2015 – when Sars II did not exist apparently. https://jdfor2024.com/2021/01/us-patent-2020279585-pcr-test-submitted-by-richard-rothschild/
Removed of course and the farcecheckers saying it is a fraud. I wonder who pays them.
Kary Mullis was murdered most likely and he invented the thing and said it had 0 to do with ‘virus’ testing.
I’d forgotten about Rottenchild and his PCR test.. good post.
Agreed..
On the face of it this is off-topic and possibly annoying, but has anyone else noticed how people are saying “quite the” (as in Mogwai’s “quite the moot point”) where the normal usage is “quite a”, with “quite the” reserved for likening to archetypes or famous instances (e.g. “quite the little Napoleon”)?
I often wonder how these things spread (the rash of semi-colons is particularly puzzling). Or is it just that, as with certain haulage companies’ lorries, once you’ve seen one you keep noticing them?
The FOIs issued around the globe by Christine Massey regarding an isolated & purified sample of SARS-CoV-2 resulting in zero samples tells us that it doesn’t exist outside of a computer model as we have been lead to understand.
Dr Parks explains the route for shedding from the “vaccinated” (in my book they’ve been injected with a toxic by design bioweapon. Lied to, coerced, threatened with job loss & downright bullied into a having medical intervention which they did not need & was anything but safe or effective).
This is why we all need to keep detoxing
https://twitter.com/drCParks1/status/1648332294849953793
What was the mode of transmission or commonality between those who were diagnosed with covid prior to the covid bioweapon injection being made available if we accept that a wild SARS-CoV-2 ‘virus’ doesn’t exist?
There was research carried out on the US military during the 2017-2018 flu season looking at rates of viral interference within the ranks & the rate of infection was higher amongst the cohort who had received the annual flu jab. https://www.sciencedirect.com/science/article/pii/S0264410X19313647
Did they put something into this jab? If they did, then what Dr Parks suggests makes sense as a mode of stimulating an illness in an individual who had the flu jab & also as a mode of transmission to those who did not. Was this a trial run for the 2019 flu jabs? Bear in mind that covid infections were occurring in Autumn 2019 during & after the flu jab campaign before there was an official label for it.
Another piece of evidence that there was no wild virus of SARS-CoV-2 is that no primates ‘caught’ covid. Thanks for this to a primate expert specialising in orangutans for this nugget.
Thank you for this very succinct summary – I would just like to mention the mysterious vaping illness/disease of summer 2019. What on earth are in those vapes?
I’d completely forgotten about that vaping thing.
A very good question! A load of synthetic crap, I do know that much. I also know someone who has carried out live & dried blood analysis, using all 5 fields of blood analysis rather than just the 1 used by the NHS or the 2 used by most researchers, who has found that blood of someone who has vaped is seriously trashed whereas blood from someone who rolls their own pure tobacco & doesn’t use filters doesn’t change…. Interesting eh?
It’s almost certainly true that the knowledge of how our immune systems actually work is a bit weak. While I agree with the assessment of the risks associated with the so-called “vaccines” against infection by SARS-Cov-2, the other issue is that they appear not to be capable of preventing infection. At best, it might be capable of mitigating the effect of infection – but also has it’s own health risks in a variety of ways.
Maybe tweaking the definition of “vaccine” to be able to use the term is a significant outbreak of fraud, to the extent that they have not explained why. Marketing a novel product might have something to do with it, assisted by selling a “something must be done” tactic to simplistic politicians, perhaps.
At the end of the day, the whole concept of “Lockdown” should be shown to have been a bad idea, and should never be repeated.
As to the validity of some of the information available, the old term “Garbage in, garbage out” floated through my conscience; not sure why.
I’m not qualified to comment much but it seems to me that whoever is right we are interfering in things we have little understanding of and step 1 is to leave well alone.
Well said. This is what the Precautionary principle used to mean before it was corrupted, by the EU I think.
It’s far from clear to me that eliminating respiratory viruses completely with vaccination, assuming that were possible, is a desirable goal.
Then you will find the following video thought provoking and I hope informative:
https://www.youtube.com/watch?v=o_nKoybyMGg
Danish professor: mRNA vaccine study sends ‘danger signals’
In this video Professor Christine Stabell-Benn talks about how a live Measles vaccine had a significant benefit compared to a dead Measles vaccine. The live vaccine appeared to not only provide protection against Measles but other pathogens. Perhaps because the live vaccine had given natural immune systems a good work out?
Irrespective, whether live or dead vaccine, or natural infection, it will always be the natural immunity that will do all the work – vaccines are not a ‘disinfectant’.
Thanks
Interesting
Effects of a “vaccine” on all cause mortality are not habitually studied in “vaccine” trials
The “covid vaccine” trials’ control groups were given the vaccine after 4 months
“Public health”. Folly and evil.
Fascinating article. Lots of food for thought.
I’ve have 2 branches to my professional interest. Medicine and medieval history (don’t ask- complicated) . What I’ve learned over my careers is that Viruses love us. Without us they die. Rather like head lice- we’ve thrown the medical kitchen sink at them, but hey ho – they thrive to this day.
Fact is immunologically is incredibly complex and we only understand a fraction, and it is always evolving. We will never kill all viruses or even control them, they are very good at finding people and always have been.
What kills people with all of them and always has is pre existing conditions and those with chronic/ terminal illness- without being brutal they finish people off.
We won’t ever ‘win’ and we just have to live with our visitors.
Forgot to add- in some viruses do envoke a huge inflammatory response which can kill, but again usually those with something going on under the surface.
land finally, for Models and modellers read astrology and astrologists.
I agree with your second point: “Many, many people disagree with me on this point.”
How much of this was due to inaccurate diagnosis? It seemed for a time that all flue-like symptoms were claimed to be covid, and not all instances were properly diagnosed. The effect of this would have influenced the data suggesting there were more covid infections than there actually were. Sometimes data was fiddled to be closer to that of the crazy models. In the end, they couldn’t get close to those ridiculous values