There follows a guest post by an NHS Emergency Department doctor on what, from his frontline vantage point, is behind the current hospital blockages and ambulance delays. This article first appeared on the website of the Health Advisory and Recovery Team (HART), a group of experts offering a second opinion on COVID-19 policy. Sign up for updates here.
As Emergency Department doctors, we were always going to be on the frontline. In spring 2020, we were taken to one side and it was suggested we might have to say goodbye to our relatives for the foreseeable future. Few realise the fear generated in hospitals in 2020. As Emergency Department consultants we were put on 24/7 emergency shift rotas and provided with vacant hotel rooms to live away from our families for their protection. Many of our colleagues left us to it and, soon after, patients arrived showing us signs that had been put up on their GP’s door saying “closed due to the pandemic”.
Spring 2020 saw a combination of assessing and treating sick patients who had unusual and characteristic presentations of Covid in an otherwise quiet Emergency Department. The less-sick patients queued in their cars for assessment in the rapidly delivered ‘Covid-pod’. Huge hospital Covid signage was hastily erected. Doctors were redeployed to work in the Emergency Department from other specialties that were literally cancelled or scaled back hugely. I had one come to me at midnight asking why there were twice as many doctors in the place as patients; that he was bored and hadn’t seen a patient for three hours. Pre-lockdowns we were seeing over 300 patients each day. During the lockdown madness this dropped to less than 100 on some days. Many patients were petrified at the idea of coming to hospital. Others were instructed to stay away from the hospital unless extremely ill. This went on for months. Then the patients gradually came back, some with essentially no other access to healthcare. The department has not been quiet for some time now.
For many years now, my department (as with others throughout the U.K.) has been used as an overflow ward when beds cannot be found in the main hospital. Currently this is happening to an extent I have never previously experienced. A shortage of beds has been an issue for at least two of the three decades I have practised emergency medicine. It gets worse every year. The causes are multifactorial, but can be related to reduced numbers of beds or staff, decreasing access to community care, increasing waits for specialist referral and an elderly population whose primary (sometimes only) source of medical care is an emergency department. There is a major problem at the community discharge interface with patients waiting on packages of care, step-down wards, community beds and nursing homes. This exacerbates the bed cuts over the years and the centralisation of specialist services. I have heard of a hospital where one man will likely see his third Christmas as an inpatient. Patients are staying longer, and a lot are dying in hospital. These problems have just been exacerbated by ‘Covid Rules’, segregating the ‘Covid exposed’ from the ‘Covid recovered’ from the ‘Covid test positive’ from the ‘Covid test negative’ patients.
Emergency Department clinicians battle this with increasing frustration as the result is people essentially living in the department. Our department is back to seeing over 300 new patients per day and on one day last week we had over seventy patients living here awaiting hospital bed placement. Deaths in the department are increasing because sick people are remaining in the department for increasing lengths of time. The hardest bit is those needing end of life palliative care that get it delivered in the mayhem of an emergency department. It is very distressing for patients, staff and relatives.
Emergency departments operate as an outpatient interface between hospital and community. In the U.K., about the turn of the century (2000), most acute hospitals changed their admission arrangements from a GP referring to a specialty bed to a ‘single portal of entry’ arrangement. It was shrouded in the ‘safe and effective’ argument, but was a disaster on many levels. GPs no longer decided on admission; they decided on sending to the Emergency Department to decide on admission. The emergency departments were pulverised with a ‘four hour target’ for admission (under Blair’s Reforming Emergency Care). The media blamed emergency departments for ‘failing’ to meet the four hour target when, in effect, they were looking after the patients needing beds as well as serving emergencies.
The proper work of an emergency department is that of unscheduled care – people sourcing help in an emergency. The greater volume of work now is ‘processing’ admissions for inpatient specialties that don’t have beds for them. The Emergency Department is then expected to look after them, providing ward-level care (and sometimes intensive care) in corridors and rooms until a bed is available or they have been discharged (or left for heaven) from their Emergency Department trolley. (We have beds with hospital specialist mattresses for pressure sores in our corridors because of the long stays.)
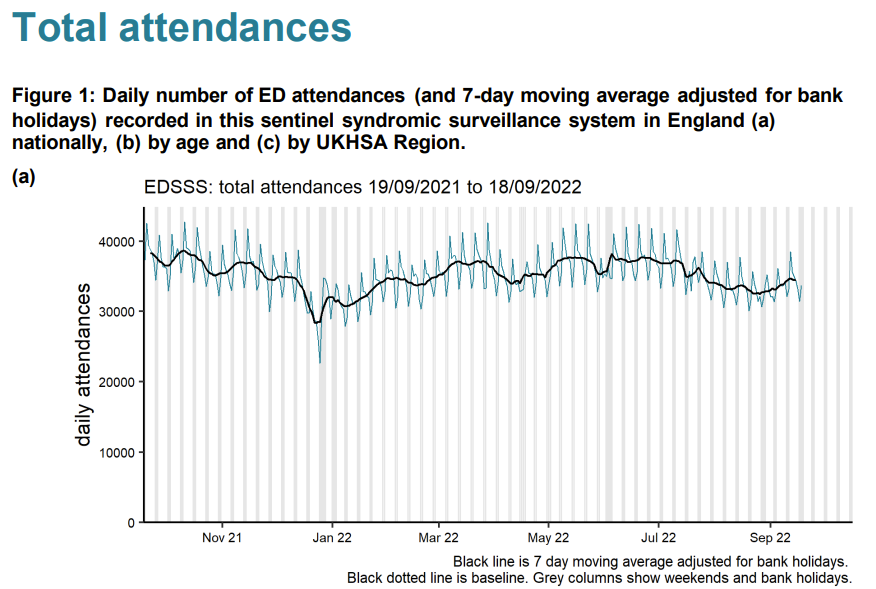
So, to say the numbers of admissions to emergency departments are lower than they were in the summer (as they currently are) gives no picture of the real congestion in emergency departments. You need to look at the number of patients waiting for beds. We are used to winter pressures with peaks and troughs. In 2021 we averaged 25 waiting in the department at a time (for at least a day) with no summer let-up. This year, for the same period, it is 45, with the worst summer ever. Emergency attendances are down – but admitted patients living in the department for days are more than doubled.
That aside, we have robust triage systems (stretched to the limit) where conditions that must be treated promptly are picked up within a target of 15 minutes of arrival (heart attacks, strokes, sepsis, haemorrhage etc.). The system is not perfect, but essentially these patients are identified as ‘time dependent conditions’ and brought to the Resuscitation Room for immediate assessment. Some are flagged by the Ambulance Service as ‘stand-by’ calls and sometimes paramedics take patients directly to where they can have, for example, urgent cardiology treatment to minimise damage from a heart attack. On the other hand, I am well aware of the recent problems with extensive delays in ambulance response times for some patients and occasions where the prioritisation has gone wrong.
Time-dependent conditions are being managed in the same way we always have and therefore perceived delays in managing them cannot be assumed to be contributing to the recent uptick in excess mortality. It is clear from experience that the incidences of heart attacks and strokes have increased significantly, although it will take time to demonstrate this with data.
I have thought about what could be causing the excess mortality we have been seeing. With regard to ambulances in particular, there are many factors involved and it is difficult to quantify which is the greatest as the data are simply not available.
1. Ambulance staffing
Ambulance staffing has been an issue over the last two years. Paramedics have taken massive ‘Covid’ leave over the last couple years. As with hospital staff, any persistent cough (pre-testing), any positive test or even a contact with someone who had tested positive and you were expected to take 10-14 days off too. Any paramedic deemed ‘vulnerable’ would stay off too. The net effect of this was fewer paramedic ambulances on the road. We had private ‘ambulances’ including St. John and Red Cross supplementing patient hospital transport. That was a major factor, but is becoming less so now as there are fewer infections, and ‘Covid’ leave becomes sick leave again.
2. Hospital Chaos
A fear of accusations that hospitals had been responsible for spread of disease meant there were over-zealous systems of separation put in place. Patients were cohorted in the Emergency Department awaiting classification: PCR-positive, PCR-negative, Covid-recovered, Covid-exposed, clinical-Covid without a test result etc. These patients could only be admitted to a ward bed if there was one available in their category. This problem was compounded with ward beds being closed for ‘social distancing.’ Covid rules meant if a patient needed resuscitation it was done in the only (tiny) negative pressure room in the department.
Patients were kept in ambulances until a separate room in the Emergency Department could be found because the whole department became organised around one disease. It was not uncommon in certain trusts to have your first 24 hours of hospital treatment in the back of an ambulance. Some hospitals would not count the time in the ambulance as part of the patient’s hours in the department, meaning there was a perverse incentive to keep patients in ambulances.
3. Community Chaos
For those that haven’t noticed, for many, general practice now consists of a telephone triage service and a ‘vaccination’ service. For a lot of people that means their only source of healthcare is the Emergency Department and their only way of getting there is an ambulance. Where previously a nursing home may have had GP visits, now problems are dealt with by calling 999.
Despite this, there have been fewer patients overall attending the Emergency Department in 2022 than the equivalent period in 2021 (which was massively up on the empty departments of the lockdowns). Unfortunately, the patients are much sicker, older or simply can’t endure having formal investigation of a complex problem postponed further. Each of these patients requires more time and stays longer. We have the same amount of staff to deal with the 300 new presentations whether the department is empty or has over 70 living there. Our Emergency Department had it as a ‘never event’ to keep a patient in an ambulance, but recently we have been overruled by the pervasive ‘Infection Control’ who now dictate who can come in. An ambulance being used as a holding bay is an ambulance that can’t be turned around for another emergency.
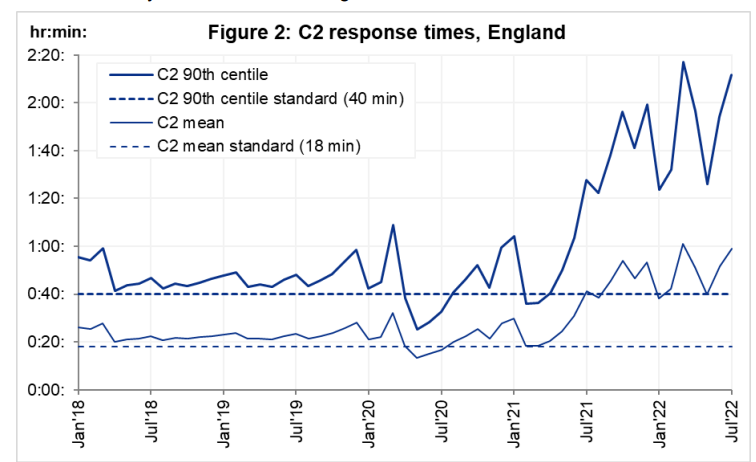
Ambulance wait times started rising from July 2021. This was when ‘Freedom Day’ from the winter Covid restrictions finally arrived and at that point patients had had enough. There was a massive upswing of hospital presentations (accompanied by perhaps a little guilt at how the elderly had been managed) and in came the patients. A proportion of these patients were victims of having not had healthcare in lockdown. For example, I recently saw a patient who had a dangerously swollen abdominal aorta – an aneurysm – which had reached a size where surgery was needed to prevent rupture and death. Surgery was cancelled twice resulting in a re-attendance at my department after it catastrophically and fatally burst.
However, it has been many years since I have seen this number of patients with heart attacks and strokes. The timing of the uptick has coincided with the vaccination programmes. Correlation is not causation (unless it fits the narrative of course). Yesterday, I saw a superbly fit young man with no cardiovascular risk factors who had had two previous vaccinations. Despite healthy kidneys he had a cardiac cell death test result through the roof (troponin of over 800) after having chest pain while exercising. I worry that the spike protein or other factors have caused damage to the blood vessel lining cells such that exercise is precipitating spasm or rupture of plaques in coronary arteries leading to heart attacks. There are too many professional and amateur athletes now getting acute myocardial damage post-inoculation for it to be a complete coincidence. And it seems to be an effect unfortunately that can persist for many months after the injection. We are allowed to talk openly about the consequences of lockdown on health but not about potential consequences of the vaccines.
The pressures on emergency departments are therefore multifactorial. They stem from changes in how patients are referred to specialty care, the role departments have taken on as an overflow ward, and the additional constraints brought in with Covid rules. However, on top of these issues, the sicker patients we have seen, even in summer, have caused catastrophic pressure on the system. The knock-on effect is ambulances unable to drop off their patients and not being available for calls such that ambulance waiting times have rocketed. There is only so much we can do as emergency physicians. What is really needed is a sustainable fix for these underlying problems.












To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
Unlike co2 and climate where non existent correlation on a geologic timeframe between co2 and temperature definitely means causation, whereas for Jabs and heart attacks clear correlation definitely doesn’t equal causation. See how it works, in both cases the “scientific conclusions” are driven by .
.
We need to be honest with ourselves, Britain is rapidly diminishing as a first world country. If we are indeed seeing another black swan event brewing in the financial markets, will we ever recover our status?
In the long term we are far too resourceful not to recover, but in the short term – the next couple of decades at least – I can see an almost total financial and economic collapse coming. A great reset indeed.
Quite so, but my worry is that the “we” in “we are far too resourceful” are not the same “we” as “we” used to be.
On the off-chance the author or any other doctors are reading: if someone was worried about their heart’s health post-vaccine, say from experiencing similar pains or other strange/novel symptoms, what tests might they seek privately to find out whether or not their heart might give out suddenly? Lockdown made me horribly unfit and I want to fix that, but I do have concerns that something might be amiss after two Pfizer jabs and suffering completely alien dizzy spells and strong palpitations after mild exercise. I anticipate a level of scoffing at this query by some doctors, so would like to be armed with specifics.
I know someone who got an ECG Monitor, it will pick up any signs of irregular heartbeat, that’s often an early warning sign.
I’m not a doc, but a retired Reg Gen Nurse with varied experience. Not all GP’s have shut up shop, and many are now getting back to a sort of normal, so it would be worth a chat with the receptionist explaining how concerned you are in the hope you will get an appointment to be seen for review. It shouldn’t happen, given the symptoms you describe, but if unsuccessful with your own GP, search on local private GP services, unless you already know of one. Phone for an appointment, based on your concerns, which should elicit a thorough examination, which would ideally include a range of blood tests, including clotting studies and ECG. You really shouldn’t need to walk in with conclusive evidence you have obtained independently. Be aware that an ECG might not necessarily pick up a heart irregularity unless you’re having palpitations at the time, so the blood tests might be more significant.
Most GPs must be aware now of the heart possibilities in relation to the vaccine and Covid, and they would have to be crazy to dismiss you with verbal reassurance that it’s just anxiety. Explain your aims to return to fitness, your symptoms and your concerns. If you don’t get a response you are happy with, say so diplomatically and ask for a second opinion. Ultimately, as a last resort, present at A&E, which is what the writer describes is now happening.
Some GP services have been “disappointing” according to my ex-colleagues working in the community, while others have struggled on short-staffed. I hadn’t considered it, but one of the things which has slowed the number of face to face appointments has been the need to adhere to the thorough cleansing of surfaces etc., between each patient. A necessary, but tiresome process.
Finally, I had what I consider was a painful neurological reaction following my second vaccine dose which severely affected my mobility for some months. One year on it has now settled completely, but left me supremely unfit.
Good luck and best wishes.
I had similar symptoms to those you describe so I went straight to a cardiologist (privately of course) where they did an ECG which showed my heart’s electrics are buggered. Probably cause at my age? Myocarditis. Pacemaker being installed this Monday. More fool me for believing the vax hype last year. Hope you come out well.
I see patients in Community Ophthalmology. I worked all the way through,tried to see as many patients as allowed face to face, and lied frequently to pretend something might be an emergency. I admit the lies were partly to get me into clinics. Often I would be the only one there in the health centre.
I never had to use the Yellow Card system before. Bell’s Palsy became so common after vaccinations began that I had one 19y old who diagnosed herself because her friend from the same street had it!
I have seen strokes, retinal haemorrhages, Ramsay-Hunt cases and central retinal artery occlusions. Some will have been by chance, but I have seen more Bell’s cases within days or weeks of vaccination than in the previous decade.
One of the Ramsay-Hunt cases told me her husband who was vaccinated on the same day died 4 days afterwards from a massive pulmonary embolism. Doctors told her categorically, without a post-mortem that this was not linked to the vaccine. That was a blatant lie. They could not know.
Patients became so fearful in some cases that they refused to attend for regular reviews and suffered permanent damage to their sight.
Now I am seeing people who have lost sight from glaucoma (that is permanent) because of lack of follow up or hospitals being overwhelmed and not seeing patients. Cataract surgery is hugely delayed and I have seen cases where people have tripped and broken hips necessitating emergency surgery. One lady broke both hips separately while waiting for cataract surgery.
Finally, my wife’s cousin is a lodger. In early 2020 her GP surgery refused to see her for a ‘wart’ on her back. When it started bleeding I had a look. Melanoma was the diagnosis Grade 3c with under 50% chance of 5y survival. She has had neurosurgery to remove a cerebral secondary, but the headaches and nosebleeds are back.
My anger at colleagues who refused to do their job, at public health officials, government and the media is enormous.
I will keep working the extra hours but it is pretty thankless and depressing.
Well, I think it is great that there are still medical professionals who want to go all out to help people who need it, so I thank you – and I also thank you for sharing your experience.
I have fortunately not had to be anywhere near a hospital or GP for a long time, so I have no idea what is going on inside medical institutions. It is great to hear firsthand experiences such as yours. I hope you and other medical professionals, such as the A&E doctor who wrote this article, write down their experiences, I think as much information as possible must be recorded for the future. The tide is turning, a wider group of people is finally starting to question, investigations are starting. It is people like yourself who have very valuable information.
It may be depressing to see so many people suffering worse than need have been the case due to delays, etc., but you must surely also have helped plenty of people during this time.
Thankyou. What annoys me most is that we as doctors are paid well above average, and sometimes we have to take small personal risks.
That is nothing compared to my Great Uncle who was an ANZAC doctor in Gallipoli. Too many were ready to run away from Covid.
The scales fell from my eyes about Covid when I was fearful but volunteered for ICU work. I was blocked after a long exchange of emails about various box ticking exercises. In fact I was up to date. I said I was happy to wipe bums if that was what was needed for Anaesthetists and ICU nurses to get on with their jobs. I was told that I was not needed. At that point I realised that there was no health emergency, just a public health system that had lost touch with reality.
I know personally of 2 nurses here in NL who had volunteered in the first wave – one was registered in the official HCW register, the other had been retired for 1 year and could easily have reinstated her registration. They were both told they weren’t needed, even though every day on the telly the story was that there was such a desperate shortage of HCW.
Now they’re trying to dial up the fear again, saying we’re in the middle of the autumn wave. If you look at the Dutch government’s own corona dashboard even a fool can see that the hospital/icu admissions have not only plateaued, they are on a downward trajectory. Yet we have idiots screaming we need to bring masks back, a rent-a-virologist who’s saying criticism of the government’s measures undermines support – so in other words, do not criticise, do not look for what works and what does not, agreement is more important than effective policy.
Having said that, NL never went as crazy as the UK, GPs were limited during the March 2020 wave, after that I think it was pretty much as normal, dentists and opticians the same. Care homes refused to lock out visitors again as it had caused so much harm to the elderly relatives.
There’s a doctor here in NL facing a disciplinary board right now for prescribing HCQ and ivermectin and for insisting that his patients give informed consent before he would vaxx them. You and he and anyone else who continued to do what was right for people rather than the government and $cientists can hold your heads up high and know you did your best. Many of your colleagues will be spending the next few decades saying “wir haben es nicht gewusst”.
Respectfully you didnt need to go to an ICU ward, the diamond Princess cruise ship data was so utterly clear that this disease flu like. This was known in March 20 therefore the whole thing was an exercise in the pharmaceutical establishment monetising a flu like disease with an unfamiliar name. I still believe if we behaved so irrationally every flu season (throwing the sick in to care homes) we could engineer massive excess mortality every year.
True, but I started the process at that time and learned about ICU nursing via an online American ICU nursing course. I carried on with the process as I was being prevented from seeing most patients face to face and wanted to do something useful.
The emailing only ended in May.
Funny how most people have forgotten the Diamond Princess.
We live in a world of goldfish overseen by sharks.
Too true!
I most definitely did not bang pots for the NHS but I don’t hesitate to take my hat off to you. Thank you.
You’re spot on re “public health system that has lost touch with reality”. It’s a disgrace yet we are made to dance to its tune.
Thanks for posting and God bless you.
How sad that we medical practitioners have to largely remain anonymous in our comments. Like you, I refuse to be silenced but have to always tread a fine line.
I also have made more adverse drug notifications to Covid “vaccinations” than I have made previously in a 40 year career.
God Bless you. I have completely lost faith in the medical profession over the past 2 years. But it is comforting to know that there ARE doctors out there who are honest and doing their best under extreme pressure. The problem we have is identifying them.
‘The causes (of these pressures on the NHS) are . . . an elderly population . . .’
And what about an ever-increasing population due to massive uncontrolled immigration?
The great lie is this is all new. It isn’t. It may have gotten worse, but I worked in the NHS in the early 70s, then on the supply side until 2001 and the above problems are chronic. The notion of Matron and a golden age of the NHS just are not true.
My experiences as a patient over the years suggest to me the NHS would not be able to function at all without immigrants.
Are other European health systems, especially those that perform much better than the NHS, similarly dependant on Third Worlders?
How on Earth did we manage when the population was almost entirely indigenous?
In don’t know, but I wasn’t just referring to immigrants from Third World countries.
I don’t know what you mean by indigenous population. You can’t mean Anglo-saxons because they came here from mainland Europe. Perhaps, the Iron Age people or the Stone Age? You lost me I’m afraid.
Chris – I’m sorry, this is pretty pathetic! You know perfectly well what Nearhorburian means, and so do I and so does everyone else.
No, genuinely I don’t. Is it a code?
Three words explain it all: National Health Service.
What it proves beyond doubt, is because of all the demands on the public purse, responsive, consumer driven medical care is unaffordable as a State funded and provided service free at the point of delivery.
Just two factors (but there are more): absent revenue stream and profit, the entity cannot grow organically by self-financing; absent a price structure the only rationing available is making people wait, there is no user restraint for anything that is free. The solution, a medical care system of insurance and provision in a competitive, private market. (There’s no point in free access to medical care, if none is available when you need/want it.)
As for GPs, the solution – see above – but meanwhile: pay per consultation rather than per capita for those on their list, and patients not tied to a particular practice This will be an incentive to see patients quickly and increase throughout and competition between practices will ensure a quality service.
Every Winter there are Cold & ‘flu epidemics, some worse than others. We used to have isolation hospitals reserved for infectious disease – interestingly these were all closed or repurposed by 2000.
Isolation hospitals require nothing special just standard medical/nursing care, but would require accommodation for staff who would isolate too. These could be mothballed in Summer perhaps, or maybe provided by the private sector.
This would free up resources in general hospitals to deal with normal throughput.
There would be a cost, of course, but isn’t there a bigger cost not having them?
Great post.
Sadly all common sense has gone up in smoke and the dark ages are returning.
There is definitely currently a correlation between excess deaths and the jabs. Areas of England with higher uptake of the vaccines are seeing higher levels of excess deaths. This pattern has persisted since Easter.
The obvious is blamed on Long Rona or Bacon Syndrome. The Quacks are paid to push the narrative. I have zero respect for the National Death Service. I did not bang pots. I don’t view them as heroic. I don’t care for their Tik Tok dance vids. They are paid for every single Rona event. Not a tithe of them have the intelligence or honesty, or morality to declare opposition to the Rona fascism. Not a jot of them know that the quacksines are derived from murdered babies (but no need to take a knee for the murdered babies). They are in essence the glittering scum of a diseased system of sewage.
Indeed, but we have to fight baseless claims with data and hard evidence.
If long Covid was to blame then I would expect to see a correlation between total Covid cases and excess deaths in each LTLA region. But I don’t. In fact there is absolutely no correlation whatsoever:
Can ask what the different colours mean? Just curious.
There are 3 x more dead from the Stabs (close to 50k), than from the terrifying Rona, real dead count about 17K over 2 years, with an IFR of 0.03% (once you strip out the data fraud, murdered wrinklies assigned to Rona etc etc all paid and compensated). Dr. Baffled is confused. Nurse Stabbit is perplexed. Hospital Climate-thingy is yet again in chaos. SADS means bacon and eggs syndrome or playing video game syndrome. Or like the bald headed idiot on Steyn’s show, simply that the crinklies are kicking off, nothing to see here. I remember when aspirin was withdrawn after 7 dead in the US……
I’m pretty sure Aspirin is safe and effective though. The comparison I find compelling is with the Swine Flu vaccine in the US in 1976, which was stopped after less than 50 deaths from Guillaine Barre syndrome.
The Public Health Bureaucrats and Health Trust Management who are responsible for this chaos and malfeasance should be sacked and, if possible, prosecuted.
In other words, the jabs plus the massive backlog and collateral damage from the lockdowns did the exact opposite of “save the NHS”. Who woulda thunk it?
I’m rapidly coming to the conclusion that I would like a knock-me-dead-definitely-and-without-pain pill, to take the next time I feel a bit off colour and contemplate a visit to my doctor / hospital. I’m 70, without debts or dependents, retired. I feel that way I can make space for whoever is next in the queue and feels the need to continue with their sojourn here.
Two thoughts. Why are these experimental biologicals not stopped with immediate affect? Pfizer has admitted they did not test for transmissibility before selling millions of their product. Drs. Peter McCullough, Bhakdi, Ryan Cole, Marik, Pierre Kory have been crystal clear that the covid injections are causing severe adverse events including cardiac events. VAERS, Eurovigilance, MHRA yellow card same. Denmark, Sweden, Norway and most recently via the state’s Surgeon General, Florida has recommended these injections be halted for certain age groups. Exactly how much more evidence is needed to stop killing people?
Secondly, why isn’t a nurse practitioner assigned to every nursing/care home in the country to triage, assess, order early treatments for ill patients, rather than sending these poor people to a hospital?
Finally, why are doctors ignoring ALL the data on early treatment for Covid. Much of it from Dr. Tess Lawrie. How many covid patients would have had better outcomes. Midazolam, remdesivir, ventilation, seriously injured or killed it’s victims. Meanwhile ivermectin and HCQ and other repurposed drugs did a stellar job in improving the condition of covid patients.
I am sorry doctors have been suppressed, banned from doing what they thought was right for their patients, and forced to take experimental biologicals, but it is now way past time for doctors to organise, represent themselves and practice medicine with authority.