Approximately one year ago, I wrote about the Bangladesh mask study – the only randomised control trial of community masking since the start of the pandemic. (The well-known Danish study examined the effect of masking on the wearer; not the effect of community masking on community-level outcomes.)
While the Bangladesh study did find significant differences between the treatment and control arms, I described it as a “missed opportunity”. That’s because it wasn’t an RCT of mask-wearing per se, but rather of mask promotion campaigns. And the latter may influence transmission through mechanisms other than mask-wearing – such as by changing people’s behaviour.
Now there’s a new critique out claiming the study’s original conclusions may be wrong. It’s a bit technical – let me explain.
In a typical RCT: 100 patients get the drug, another 100 get a placebo, and you compare how many in each group get sick. But the Bangladesh study had a much more complex design – as shown in the figure below.
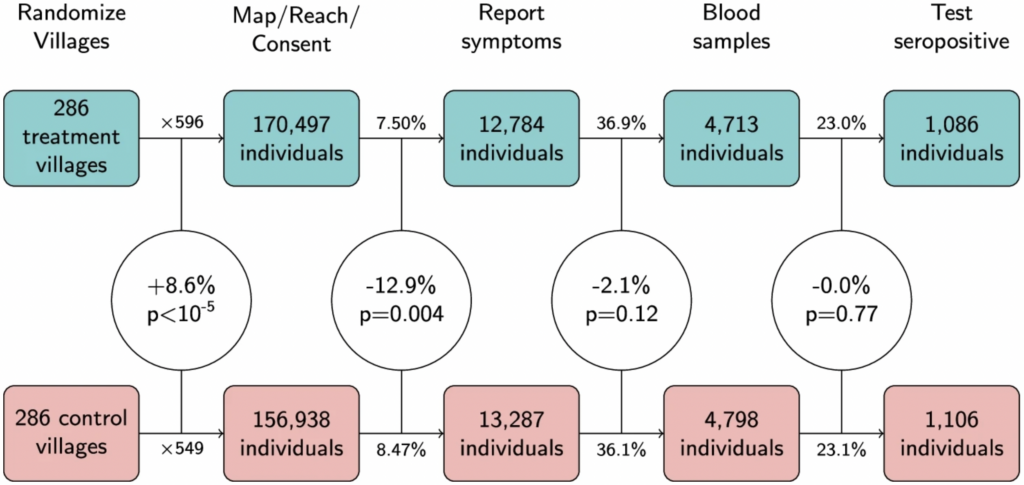
Headings across the top represent different stages of the experiment: first villages were randomized; then individuals within those villages were sought for consent; then they reported their symptoms etc.
The main thing to notice is that there was a statistically significant 8.6% difference between the treatment and control arms in the number of people who agreed to take part – 170,497 versus 156,938. (For those well-versed in stats, the corresponding p-value was less than 0.00001.) This isn’t supposed to happen in an RCT.
As noted by Maria Chikina and colleagues, who wrote the critique, this difference arose because the staff who went out to the villages and sought people’s consent were unblinded (i.e., they knew whether they were visiting a treatment or a control village). As a consequence, those in the treatment arm behaved slightly differently from those in the control arm.
Crucially, the 8.6% difference is as large as the main result of the original study: seroprevalence in the treatment arm was 8.7% lower than in the control arm. This means the main result could be due to factors other than the experimental treatment – even though the study was technically an RCT.
In fact, when Chikina and colleagues calculated the difference in seroprevalence measured as a count rather than as a rate – i.e., by comparing the absolute number of cases in each arm, while ignoring the denominator – they found it was only 1.8%. And you could argue this is the “correct” way to calculate the difference, given that randomisation of the denominators failed.
Overall, the new critique doesn’t prove the original conclusions are wrong. But it does show the data are consistent with mask promotion campaigns having had zero causal influence on the outcome variables.











To join in with the discussion please make a donation to The Daily Sceptic.
Profanity and abuse will be removed and may lead to a permanent ban.
“There is absolutely no reason to continue with mass testing children. All it’s doing is prolonging the disruption and prolonging the fear.”
Excuse me. Isn’t that the whole point of this child abuse?
You took the words out of my mouth.
While the testing is bad enough, the jabbing of children with unnecessary and highly dangerous gene therapies is an an act of the utmost criminality. The instigators and the operatives who carry out this malicious practice will have to be locked away for the rest of their natural lives.
No, they need to be shot. So many times we have forgiven these evil people who instigate such horrors and every single time they lurk in the shadows and plot and plan. Johnson’s father is a eugenicist, Bill Gates whole ancestry is full of Bolsheviks and eugenicists. As are the Rockerfellers and Soros. They are quietly left to ‘disappear’ but they always return.
We either stop these people once and for all or we allow this evil to occur every 100 years. We NEVER LEARN. They are determined to depopulate us but we never understand that
Where’ve you been Dr Kingdon? Children have been subjected to a post-apocalyptic version of their educational setting and treated like disease vectors for over 18 months in a so-called pandemic which didn’t need to involve them at all, before being made the subjects of sinister medical experiments. But continued testing is beyond the pale is it?
I will watch with fascination as those behind this nightmare attempt to pivot away from taking any responsibility for it.
If the President of the Royal College of Paediatrics and Child Health says we must end mass testing, this just gives Boris Johnson another medical expert to ignore and implement the opposite.
It’s a bit late in the day for this. Anyway now that she has shown some bottle she needs to keep the pressure on and push for the casedemic to be ended.
What a shower. Pity she didn’t think of children when the scam started. A generation scarred while she looked on. Some legacy.
She is realising that her life and her career is on the line. If she had any compassion or thought for the children she would have stood up at the very beginning. There is no excuse for people in her position to have stayed silent for so long. Anna de Buisseret is correct. They know they have done wrong and they are now trying to distance themselves.
I keep reading Dr Klingon. Now it’s stuck.
How Worful.
It’s a start.
The sour remarks here are pointless.
Yes, I agree. I’ve not read the whole piece but the direct quotes from her are pretty unequivocal, and she’s not some retired expert but a serving head of a relevant body. These are the kind of people who have to start speaking up if we’re to get out of this madness.
That’s the point. Many of us here can sit on our anonymous (pro tem.) arses. This is somebody who, on current experience, has something to lose.
Yes I suppose so. Duly noted.
I don’t think we are being sour. We are being honest. She should have spoken up before. Of course it’s a start but in my experience these people are saving their own skin in the hope they can carry on in their profession. However, we really do not need people in these professions who do not put the children first. We need people who wish to serve. We now have a highly bureaucratic system of government which history shows leads to narcissism and unaccountability. Service to fellow humans is way down on the list.
Absolutely.. better late than never. The more people of her standing that put their heads above the parapet the better. She, and others like her will be being closely watched by her peers who will sense a shift. Its important she’s supported, not vilified.
There was a time when if the government said something needed to happen, it would happen. Not now. They said in summer ALL restrictions have ended. But the education sector and its overpaid leaders know better, just like the NHS. So they just basically do what the hell they like, and are seemingly beyond reproach.
We have a pathetic leader in charge who does not have the balls for a fight with the education authorities or the unions. So he just lets them do what they like, and the kids suffer.
I was not fan of Thatcher but, my god, it needs somebody like this more than ever to sort out these imbeciles running local authorities and their various assorted QUANGOS.
Fascinating article over in conservativewoman about how covid-19 was removed from the PHE High Consequence Infectious Disease list four days before the disastrous lockdown because to leave it on the list meant the legal obligation “to consider antiviral prophylaxis, and arrange as necessary.” With such medicines in play, the gene therapies would never been made legal.
This is all so filthy, and so very corrupt, there will absolute hell to pay when this all comes out.
I remember wondering at the time why they’d done this. Should have know it was more lies preparing the ground for the pretend need for vaccines.
Ironically, tho’ it was the correct decision.
When this comes out we may be too far down the line for those in control to care very much. More parents should learn to trust their own instincts instead of following a bureaucratic mantra. It seems to me the teenagers are beginning to ask more intelligent questions than their parents. I pray that we have at last created a real hunger for our youngsters to want a future they create and not a future given away by their parents through health fears.
The link:
https://www.gov.uk/guidance/high–consequence-infectious-diseases-hcid
”When this all comes out…” How, exactly? Find a court willing to listen and to be unbiased. Not easy.
She’s f****d then.
Mass testing of well people should be stopped full stop!
What did Kary Mullis say?
Before he died untimely.
There can only be one logical reason for testing well children and that is because not enough well adults are being tested to produce numbers to keep this shit show going.
Stop testing and it all folds. Its always been a testademic from the start.
Me thinks Dr Kingdon is holding back slightly…
And cases just keep going up in the UK. Despite all the npi’s! lockdowns, quarantining, masks, socials distancing, track and trace, two weekly lft tests, testing centres on every corner of the country. Oh dear, anyone else accept this gov’t would consider changing tack. How about approving early treatments with repurposed drugs and simply following the Sweden model for starters.
They’re NOT ”cases”.
It’s time children were taken out of school and taught in small hubs at home. The education system is totally broken and dangerous. The teaching unions are causing division and have are no use anymore.
Some in those teaching union positions need taking outside for a good old fashion lesson, and I’m not talking domestic science..
And how can we be sure they’re not ”plants”? (Besides their IQ, of course.) They would need to be watched.
Everyone, especially carers and parents need to get a load of these Consent Checklists printed.
Why wouldn’t you?
They should be put on car windscreens and through letterboxes everywhere. Any parent or carer who criticizes or doesn’t understand this checklist is basically a mouth-breathing fool and should not be responsible for anyone, child, adult, or family goldfish.
“First, do no harm!”
This checklist does no harm it will very likely do the polar opposite.
It will save lives!
BandStand in BlakePark – Bridgwater – Somerset. Every Sunday 10am meet like-minded people who can see the bleedin’ obvious.
Telegram: Connecting Warriors.
Other venues are available all over the country but you won’t find their details on MSM.
If unsure A good start would be Telegram groups for your area. “A Stand in the Park – Bracknell & Wokingham”. Via posts from our very own ‘Lockdown Sceptic’ A regular here on DS
Here’s the flip side.
The problem is that we’ve been fed so much coercive garbage that we hesitate to believe someone like this person is ‘kosher’. Perhaps she is, and I hope so, but why didn’t she say something way before now, when the damage has begun? Doesn’t she realise that her message is now undermined and diminished by what goes on around her? If she doesn’t then she is naive and shallow. Or perhaps coerced herself.
Noting the inexorable rise is “cases” I do wonder what the age breakdown is – but cannot find it anywhere. If all the positives are in children who are at low risk from developing serious disease there’s another good reason to stop testing them. Mind you, testing is a shambles anyway. We booked Day 2 tests for our return from france. One came, one did not. Despite numerous emails and phone calls the problem with the supplier remains unresolved – but NHS 119 stepped in and are sending a test! Madness.